Yellow Skin (Jaundice) in Bile Duct Cancer
Yellow Skin (Jaundice) in Bile Duct Cancer: Understanding the Significance and Care
- Why Does the Skin Turn Yellow in Bile Duct Cancer?
- The Biological Mechanism Behind Jaundice in Cancer
- How Common Is Jaundice in Bile Duct Cancer?
- Causes of Jaundice in Cancer: Not Just Tumor Growth
- When Yellow Skin Signals an Emergency
- How Doctors Diagnose the Source of Jaundice
- Treating and Relieving Jaundice in Bile Duct Cancer
- Can Jaundice Be Prevented or Detected Early?
- Does Yellow Skin Go Away Over Time?
- What Doctors Say About Managing Jaundice in Bile Duct Cancer
- Summary and Internal References
- 15 Questions to Ask Your Doctor About Jaundice in Bile Duct Cancer (FAQ)
Why Does the Skin Turn Yellow in Bile Duct Cancer?

The yellowing of the skin, also known as jaundice, is one of the most recognizable signs of bile duct cancer. This symptom, while visually striking, is not just cosmetic—it indicates a serious disruption in the body’s ability to process and eliminate bile. In bile duct cancer, the tumor can block the normal flow of bile from the liver to the intestines, leading to a buildup of bilirubin in the bloodstream.
Jaundice is often the first noticeable symptom of bile duct cancer, especially when the tumor is located near the hepatic hilum or in the extrahepatic ducts. As bilirubin levels rise, yellow pigment begins to deposit in the skin and sclera (white of the eyes).
In some patients, jaundice may be accompanied by dark urine, pale stools, and itching, making it not only a visual issue but a source of significant discomfort and distress.
The Biological Mechanism Behind Jaundice in Cancer
The liver constantly produces bile, a fluid rich in bilirubin—a waste product formed from the breakdown of red blood cells. This bile travels through a network of ducts into the intestines, where it helps digest fats and is eventually excreted.
In bile duct cancer, a tumor can obstruct this drainage system. The backup of bile causes bilirubin to accumulate in the bloodstream and deposit into tissues. This systemic rise in bilirubin causes the yellow discoloration of the skin, mucous membranes, and eyes.
If the obstruction is complete or rapidly progressing, jaundice can appear suddenly. Partial blockage may lead to a more gradual onset, often missed in early stages.
Additionally, some patients receiving radiation therapy for bile duct cancer may experience inflammation that narrows the bile ducts, worsening jaundice symptoms even in the absence of significant tumor growth.
How Common Is Jaundice in Bile Duct Cancer?

Jaundice is extremely common in bile duct cancer, particularly in tumors of the extrahepatic (outside the liver) or perihilar regions. It is the most frequent presenting symptom in many cases.
According to clinical data:
| Tumor Location | Prevalence of Jaundice |
| Extrahepatic cholangiocarcinoma | 80–90% |
| Perihilar (Klatskin tumors) | 70–85% |
| Intrahepatic tumors | 20–30% (usually later) |
| Post-surgical recurrence | 50–60% if obstruction recurs |
Early jaundice often drives patients to seek care, making it a critical diagnostic clue. However, in some intrahepatic cases, jaundice may be absent until the disease is quite advanced.
This makes understanding the Bile Duct Cancer ICD-10 classification system important for properly identifying and coding various subtypes that affect jaundice presentation.
Causes of Jaundice in Cancer: Not Just Tumor Growth
Although tumor obstruction is the main driver of jaundice in bile duct cancer, there are multiple contributing factors that can worsen or mimic the condition:
| Cause Type | Examples |
| Mechanical Obstruction | Tumor mass, lymph node compression |
| Inflammatory Response | Post-surgical swelling, radiation therapy |
| Post-Intervention Scar Tissue | Strictures after stent placement or surgery |
| Metabolic Dysfunction | Liver metastases, bile acid imbalance |
| Infection | Cholangitis from bacterial overgrowth in stagnant bile |
| Drug-Induced Liver Injury | Chemotherapy toxicity, immunotherapy |
In some patients, jaundice may appear even after successful tumor removal due to scarring or treatment complications. This reinforces the importance of continual monitoring and integrated care.
When Yellow Skin Signals an Emergency
While jaundice can appear gradually, certain signs accompanying it should raise immediate concern. In patients with bile duct cancer, worsening yellowing of the skin may indicate either an acute obstruction, advancing tumor spread, or even infection such as ascending cholangitis—a potentially life-threatening complication.
The most critical red flags include:
| Associated Symptom | Potential Emergency Condition |
| Fever and chills | Bacterial cholangitis |
| Sudden severe abdominal pain | Acute bile duct blockage or perforation |
| Mental confusion | Hepatic encephalopathy due to rising bilirubin |
| Vomiting blood or black stool | Upper GI bleeding from portal hypertension |
| Rapid darkening of urine | Severe liver impairment |
When jaundice progresses quickly or is paired with systemic symptoms, emergency evaluation is essential. In many such cases, hospitalization, antibiotics, or urgent biliary drainage is required.
How Doctors Diagnose the Source of Jaundice
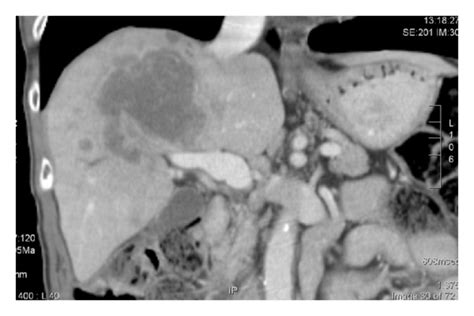
Determining the exact cause of yellow skin in bile duct cancer involves a structured diagnostic process that combines imaging, bloodwork, and occasionally endoscopic procedures. The goal is to assess whether the jaundice stems from direct tumor obstruction, inflammation, or liver dysfunction.
| Diagnostic Method | What It Reveals |
| Liver Function Tests (LFTs) | Bilirubin levels, liver enzyme patterns |
| Abdominal Ultrasound | Bile duct dilation, liver texture |
| MRCP (MRI Cholangiopancreatography) | Non-invasive imaging of biliary tree |
| ERCP (Endoscopic Retrograde Cholangiopancreatography) | Direct visualization and possible stent placement |
| CT Scan or PET-CT | Tumor size, metastasis, lymph node involvement |
| Biopsy (if needed) | Confirms malignancy or recurrence |
Blood tests may also screen for cholestasis markers and differentiate between radiation therapy side effects and malignant obstruction. A combination of tools provides the most accurate assessment and guides intervention.
Treating and Relieving Jaundice in Bile Duct Cancer
Management of jaundice in bile duct cancer aims to relieve the obstruction, reduce bilirubin buildup, and improve overall liver function. Depending on the cause, treatments can range from interventional procedures to medications.
| Treatment Option | Indication |
| Biliary Stenting (ERCP or PTC) | First-line for relieving obstruction |
| Surgical Bypass or Resection | In resectable tumors with curative intent |
| Chemotherapy or Radiation Therapy | To shrink tumors causing compression |
| Antibiotics | For infectious cholangitis |
| Ursodeoxycholic Acid or Cholestyramine | To ease itching and bile acid imbalance |
| Intravenous hydration and nutrition | To support liver recovery in advanced cases |
In patients with unresectable cancer, repeated stenting or permanent biliary drainage (e.g., percutaneous catheter) may be required to maintain bile flow. Relief of jaundice often improves appetite, energy, and quality of life dramatically.
Can Jaundice Be Prevented or Detected Early?
In high-risk patients or those with known bile duct cancer, proactive monitoring can sometimes delay or prevent severe jaundice episodes. While complete prevention isn’t always possible, early detection allows for less invasive management and reduced complications.
| Preventive Approach | Benefit |
| Regular bilirubin and LFT monitoring | Detects early biochemical changes |
| Surveillance imaging (CT/MRI) | Identifies narrowing or early obstruction |
| Stent maintenance and replacement | Prevents recurrent blockage or infection |
| Early symptom reporting | Itching, pale stool may precede jaundice |
| Minimizing hepatotoxic medications | Reduces liver stress in palliative cases |
In addition, minimizing certain triggers like dehydration or poor oral intake can help reduce the risk of biliary sludge and stone formation in narrowed ducts.
Does Yellow Skin Go Away Over Time?
Whether yellow skin (jaundice) resolves in patients with bile duct cancer depends heavily on the underlying cause, tumor location, and response to treatment. In many cases, jaundice can be significantly reduced or even fully reversed—especially if addressed early through biliary drainage or tumor reduction.
However, when the cancer is unresectable or has caused extensive scarring of the bile ducts, jaundice may persist despite treatment. In such cases, the focus shifts to managing symptoms, maintaining liver function, and improving patient comfort.
| Cause of Jaundice | Reversibility |
| Tumor compression (early stage) | Often reversible with stent or surgery |
| Post-radiation inflammation | Reversible with time and medications |
| Permanent bile duct stricture | May require repeated stenting |
| Extensive liver metastases | Often chronic and difficult to reverse |
| Infection-related (e.g. cholangitis) | Usually reversible with antibiotics |
In palliative settings, maintaining stable bilirubin levels can help patients continue systemic therapies and improve quality of life. But full resolution of jaundice is not always possible in advanced stages.
What Doctors Say About Managing Jaundice in Bile Duct Cancer

Oncologists and hepatobiliary surgeons view jaundice as a key clinical indicator—not just a symptom, but a sign that demands prompt attention. According to multiple specialists, early drainage and accurate staging are critical to avoid complications like cholangitis or liver failure.
Doctors emphasize that jaundice is never just cosmetic—it signals a disruption in liver-biliary function and often marks disease progression. Interventions like biliary stents or targeted therapy are not only palliative but sometimes essential for survival.
A leading hepatologist notes:
“If a bile duct cancer patient develops yellow skin, it’s a message from the body that something is obstructed. We don’t wait—we image, we drain, and we act. The longer bilirubin is elevated, the harder it is on the liver.”
For patients receiving radiation therapy, oncologists recommend pre-emptive bile duct mapping and close follow-up imaging, as delayed effects can appear months later.
Summary and Internal References
Yellow skin is not only a visible warning sign in bile duct cancer, but also a clinical marker of underlying obstruction or liver dysfunction. Whether caused by the tumor itself, treatment complications, or other hepatic conditions, jaundice requires timely diagnosis and thoughtful intervention.
With a combination of stenting, medication, surgical planning, and close monitoring, many patients can experience relief. However, in advanced cases, management is often focused on comfort and function rather than cure.
To further understand how skin changes reflect underlying cancer progression, or how radiation therapy contributes to bile duct complications, you can explore more through related articles.
Также полезно обсудить классификацию Bile Duct Cancer ICD-10, особенно при подготовке к лечению или взаимодействии со страховыми и клиническими учреждениями.
15 Questions to Ask Your Doctor About Jaundice in Bile Duct Cancer (FAQ)
1. Is my yellow skin caused directly by the tumor?
Jaundice in bile duct cancer is often caused by the tumor compressing or invading the bile ducts, which blocks the normal flow of bile and leads to a buildup of bilirubin in the bloodstream.
2. Can this symptom be reversed?
In many cases, yes. If the blockage is addressed early with stenting or surgery, the yellow discoloration may diminish or disappear entirely. However, in advanced stages or with liver damage, jaundice may persist.
3. Do I need a stent to relieve the blockage?
A biliary stent is a common and effective way to relieve jaundice caused by obstruction. Your doctor will assess whether ERCP or percutaneous stenting is appropriate for your case.
4. Is my liver still functioning properly?
Liver function tests (LFTs) will help determine whether your liver is handling the bilirubin load effectively. Persistent jaundice may indicate compromised liver function.
5. Could this be due to radiation therapy?
Yes. Radiation therapy can inflame or scar the bile ducts, leading to narrowing (strictures) and jaundice, even after initial treatment success.
6. Do I have signs of infection like cholangitis?
Fever, chills, and worsening jaundice may indicate cholangitis—a serious infection requiring urgent antibiotics and drainage.
7. What tests do I need to determine the blockage’s location?
Tests like MRCP, ERCP, ultrasound, or CT scan will help locate the obstruction and guide treatment decisions.
8. Is chemotherapy still safe with my bilirubin levels?
High bilirubin levels may affect your ability to receive chemotherapy safely. Your doctor may need to modify your regimen or delay treatment until levels improve.
9. How can we reduce itching caused by bile buildup?
Itching, or pruritus, can be treated with medications like cholestyramine or antihistamines, and improved bile flow may also relieve this symptom.
10. Will my appearance return to normal if the blockage resolves?
Often, yes. Once bilirubin levels drop, the yellowing of the skin and eyes usually fades within days to weeks, depending on how long it persisted.
11. Can my jaundice come back after treatment?
Yes, particularly if the tumor recurs or the stent becomes blocked. Regular monitoring helps catch these problems early.
12. Should I avoid certain foods or medications?
Yes, avoid hepatotoxic (liver-damaging) drugs and limit alcohol. A low-fat diet may also reduce bile burden.
13. How will this affect my prognosis?
Jaundice may indicate advanced disease or complications, but successful management can still lead to improved survival and quality of life.
14. What symptoms should lead me to the ER?
Seek emergency care if jaundice is accompanied by fever, severe abdominal pain, confusion, or vomiting blood.
15. Can you explain what Bile Duct Cancer ICD-10 code applies to my case?
The Bile Duct Cancer ICD-10 classification (e.g., C24.0 for extrahepatic cholangiocarcinoma) helps with clinical documentation and insurance coverage. Your care team can clarify the exact code used in your file.












