When Breast Cancer Spreads to the Skin: Understanding Symptoms, Stages, and Treatment
- How Does Breast Cancer Reach the Skin?
- Recognizing the Symptoms of Skin Metastases
- Staging Skin Metastases in Breast Cancer
- Common Locations and Visual Patterns of Skin Involvement
- Available Treatment Options for Skin Metastases from Breast Cancer
- Prognosis and Survival with Skin Involvement
- Emotional and Physical Burden of Visible Metastases
- How Skin Metastases Compare to Other Metastatic Patterns
- Diagnostic Tools for Confirming Skin Metastases
- Differentiating Skin Metastases from Other Skin Conditions
- Rare Subtypes and Unusual Presentations
- Case Study Insights: Learning from Clinical Patterns
- Skin Metastases in Elderly Breast Cancer Patients
- The Role of a Multidisciplinary Team in Care
- Can Skin Metastases Be Prevented?
- Emerging Research and Future Directions
- FAQ – Frequently Asked Questions about Breast Cancer Metastasis to the Skin
How Does Breast Cancer Reach the Skin?
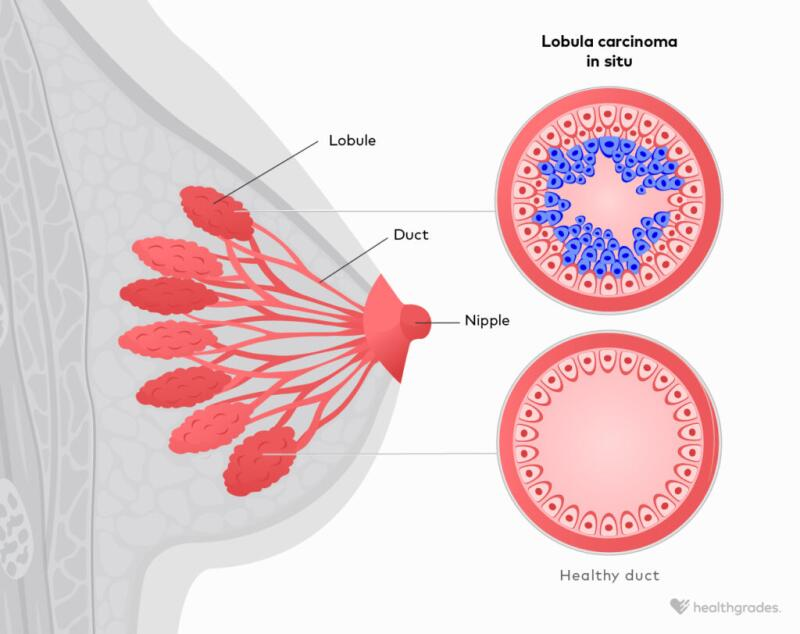
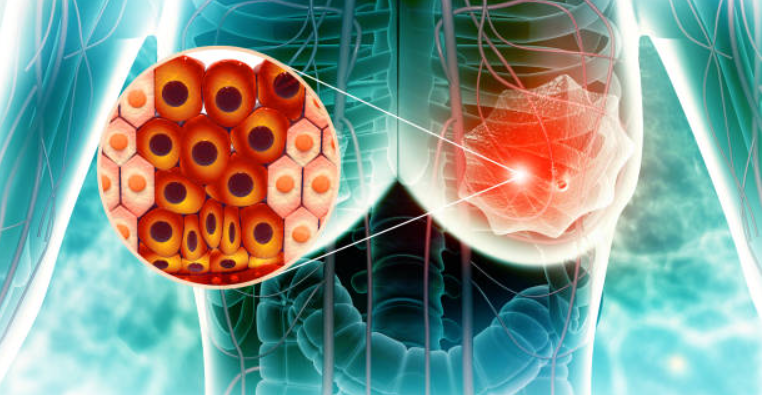
Breast cancer can extend to the skin through various pathways. The most common route is hematogenous spread, where cancer cells travel through the bloodstream and seed into the dermis. Another pathway is lymphatic spread, particularly in cases where nearby lymph nodes have already been compromised. In some instances, direct invasion may also occur, especially with tumors located close to the chest wall or surface skin.
Once these cancerous cells lodge in the skin, they form nodules or plaques that may mimic benign conditions like dermatitis or infections. For many patients, skin metastases may appear near the original tumor site, but they can also emerge in distant regions like the abdomen, scalp, or even the back.
Recognizing the Symptoms of Skin Metastases
Cutaneous metastases from breast cancer are often misdiagnosed in early stages due to their deceptive appearance. The most common presentations include firm, painless nodules that may be red, purple, or flesh-toned. These lesions typically do not respond to topical treatments and tend to grow over time.
Inflammatory breast cancer—a highly aggressive subtype—can produce rapid, widespread skin involvement that mimics an infection. Patients may notice redness, swelling, warmth, and a thickened or “peau d’orange” (orange-peel) texture. Itching, tenderness, and ulceration may also be present as the condition progresses.
It is crucial to differentiate these symptoms from other skin conditions through biopsy and imaging, especially for patients with a history of breast cancer or current treatment.
Staging Skin Metastases in Breast Cancer
Once skin involvement is confirmed, staging becomes essential to assess the overall extent of disease. In most cases, the presence of cutaneous metastases signifies stage IV breast cancer—indicative of distant spread. However, there are nuances depending on how the cancer reached the skin and whether internal organs are involved.
For example, patients with isolated skin lesions and no detectable visceral spread may have a different prognosis and treatment approach compared to those with concurrent metastases to the liver or brain. Breast cancer metastasis to liver – In cases where skin lesions appear alongside liver involvement, systemic treatment options often take priority.
Imaging studies such as PET-CT, MRI, and targeted ultrasound help visualize both cutaneous and internal metastases. Skin biopsies with immunohistochemistry also aid in confirming origin, especially in patients with multiple malignancies or unusual histology.
Common Locations and Visual Patterns of Skin Involvement
The skin lesions of metastatic breast cancer often develop in recognizable patterns depending on the underlying tumor biology and spread route. Below is a comparative overview of locations and appearances:
| Location | Presentation | Possible Underlying Mechanism |
| Chest wall | Firm nodules or plaques | Local recurrence or direct extension |
| Abdomen or flank | Red papules or ulcers | Hematogenous spread |
| Scalp or head | Flesh-colored or violaceous nodules | Distant skin seeding via bloodstream |
| Around mastectomy scar | Clustered lesions or thickened skin | Locoregional recurrence |
| Lower back or limbs | Isolated nodules or indurated patches | Rare distant cutaneous dissemination |
These appearances can evolve over time. Initially subtle, they may coalesce or ulcerate, leading to discomfort, infection, or psychological distress due to visibility and stigmatization.
Available Treatment Options for Skin Metastases from Breast Cancer
When breast cancer spreads to the skin, treatment must be tailored to the extent of disease, biology of the tumor, and the patient’s overall health. In most cases, systemic therapy forms the cornerstone of management. This includes chemotherapy, hormone therapy, targeted therapy (like HER2 inhibitors), or immunotherapy—depending on receptor status and mutation profile.
Local treatments may complement systemic therapy, particularly when lesions are painful, ulcerated, or affecting quality of life. Options include radiation therapy, cryotherapy, laser ablation, or topical chemotherapy agents like 5-fluorouracil.
Surgical excision is less common but may be performed if lesions are isolated and resectable. In some cases, palliative excision improves hygiene and comfort. A multidisciplinary team—including oncologists, dermatologists, and palliative care specialists—usually develops a comprehensive plan. The aim is not only to reduce tumor burden but to preserve skin integrity and emotional well-being.
Prognosis and Survival with Skin Involvement
The presence of skin metastases generally indicates a more advanced stage of breast cancer. However, prognosis varies significantly. Patients with limited cutaneous spread and responsive tumor biology may live for several years, especially with effective systemic treatment. Conversely, widespread skin involvement, especially with resistance to therapies, may shorten survival to a matter of months.
Studies show that median survival after the appearance of skin metastases ranges from 6 to 24 months, depending on tumor subtype and treatment response. Those with HER2-positive or hormone receptor-positive cancers tend to have better outcomes than those with triple-negative disease.
Psychological support is a critical component of care. For many patients, visible metastases serve as a constant reminder of illness progression. These challenges parallel those seen in advanced neurological malignancies like brain cancer in dogs, where caregiver support and patient dignity become central themes in care.
Emotional and Physical Burden of Visible Metastases
Skin metastases often impact a patient’s sense of identity and self-esteem. Unlike internal tumors, these lesions are seen daily—in the mirror, by loved ones, or by strangers. This visibility can lead to social withdrawal, depression, and anxiety, especially if ulceration or odor is involved.
Physical symptoms, such as itching, bleeding, and pain, can severely disrupt sleep and daily function. Dressing wounds becomes a routine chore, and patients may feel embarrassed or burdened by constant care needs. In such situations, palliative dermatologic interventions can restore a sense of control.
Family members and caregivers play a pivotal role, helping with daily dressing changes, emotional support, and transport. Open communication, counseling, and access to support groups are invaluable resources during this phase of the disease.

How Skin Metastases Compare to Other Metastatic Patterns
Unlike internal organ metastases, skin involvement tends to be more symptomatic in daily life but not always immediately life-threatening. That said, skin metastases rarely occur in isolation. They may signal deeper progression of disease, prompting oncologists to search for metastases in organs such as the brain, bones, or liver.
For instance, patients who develop concurrent skin and central nervous system symptoms may be evaluated for cerebral involvement, which in animals like brain cancer in cats manifests with similar overlapping signs of systemic decline. In human patients, MRI of the brain is commonly ordered if neurological changes coincide with the appearance of skin lesions.
Understanding the overall pattern of spread helps tailor both treatment intensity and supportive care. Unlike solitary liver or lung metastases, skin lesions often provoke more visible distress, despite not being immediately fatal. That paradox makes them a complex challenge—both medically and emotionally.
Diagnostic Tools for Confirming Skin Metastases
Diagnosis of cutaneous metastases begins with a thorough clinical examination and patient history, especially in those with known breast cancer. However, because lesions can resemble benign skin conditions, definitive diagnosis requires a biopsy. A punch biopsy or excisional sample is taken from the lesion, then sent for histopathological and immunohistochemical analysis.
Markers such as estrogen receptor (ER), progesterone receptor (PR), and HER2/neu help determine if the lesion is a breast cancer metastasis or another skin-related disease. In patients with unusual lesion patterns or previous cancers, additional markers (like GATA3 or mammaglobin) may be used to confirm origin.
Imaging studies such as PET scans, CT scans, and sometimes MRI provide a wider view of metastatic spread. These tests are crucial not only to confirm diagnosis but also to guide treatment, especially when cutaneous lesions are the first sign of recurrence after years of remission.

Differentiating Skin Metastases from Other Skin Conditions
Skin metastases from breast cancer can closely mimic other dermatological conditions, particularly infections and inflammatory diseases. To avoid misdiagnosis, clinicians must consider several distinguishing characteristics:
| Condition | Typical Features | Distinctive Traits |
| Cellulitis | Red, warm, swollen skin; often tender and painful | Rapid onset; fever; responds to antibiotics |
| Inflammatory breast cancer | Diffuse redness, swelling, “peau d’orange” skin | Often involves a large area with pain and warmth |
| Skin metastasis | Firm, non-tender nodules or plaques; persistent | Unresponsive to antibiotics or steroids |
| Dermatitis | Itchy, red patches; may weep or flake | Improves with topical corticosteroids |
| Fungal infections | Circular rashes, sometimes scaling or cracked skin | Confirmed by KOH prep or culture |
Proper differentiation is essential. Misdiagnosis can lead to treatment delays and progression of systemic disease. For oncologists, awareness of dermatological mimics is just as important as oncologic expertise in these cases.
Rare Subtypes and Unusual Presentations
While most skin metastases appear as firm nodules or plaques, some cases present atypically. One rare form is zosteriform metastasis, where lesions follow a dermatomal distribution, mimicking shingles. Another is telangiectatic carcinoma, where metastases resemble vascular lesions with red or purple discoloration.
In certain patients, especially those with lobular carcinoma, metastases may form in areas like the eyelids, scalp, or behind the ears. These can be mistaken for other conditions like sebaceous cysts or dermatitis. The diversity of presentations requires clinicians to maintain a high index of suspicion, particularly for patients with a history of breast cancer.
There have even been documented cases where skin metastases were the first clue leading to a breast cancer diagnosis, especially in older individuals who hadn’t undergone recent screening. These instances underscore the importance of skin evaluation in both primary care and oncology settings.
Case Study Insights: Learning from Clinical Patterns
Real-world examples illustrate the variability of breast cancer skin metastases and emphasize the need for individualized care:
A 59-year-old woman, previously treated for HER2-positive breast cancer, noticed a cluster of red nodules around her mastectomy scar two years after completing therapy. Biopsy confirmed cutaneous metastasis. A new systemic regimen with trastuzumab deruxtecan was initiated, leading to partial regression of lesions over six months.
In another case, a patient developed a single purplish nodule on her upper back, which was misdiagnosed as a hemangioma for months. Only after it failed to resolve with conservative measures was it biopsied, revealing metastatic triple-negative breast cancer. This delay affected treatment planning and prognosis.
These stories highlight the value of vigilance in follow-up care. Both patients and healthcare professionals should be encouraged to report and evaluate any new skin findings promptly—regardless of how minor they may seem at first.
Skin Metastases in Elderly Breast Cancer Patients
As life expectancy increases, so does the prevalence of cancer in older adults. Breast cancer in the elderly often presents with subtler symptoms, and skin metastases may go unnoticed or be attributed to aging-related skin changes. This demographic also faces unique challenges such as frailty, comorbidities, polypharmacy, and reduced access to aggressive treatments.
Older patients with cutaneous metastases may be less likely to receive full-dose chemotherapy or invasive procedures due to cardiac or renal limitations. Instead, treatment often emphasizes quality of life, with more frequent use of hormonal agents, palliative radiotherapy, or local wound care.
Importantly, visible skin lesions can be a source of emotional distress and isolation in older adults, especially those living alone or in assisted living facilities. Geriatric oncology services play a crucial role in balancing effective cancer control with preservation of dignity, autonomy, and daily function.
The Role of a Multidisciplinary Team in Care
Cutaneous metastases require the expertise of multiple healthcare professionals. The oncologist leads systemic treatment planning, while dermatologists assist in diagnosis and local management. Palliative care specialists provide symptom relief, and wound care nurses help maintain skin integrity and hygiene.
Psychosocial support is also essential. Psychologists and social workers can assist with body image issues, depression, and practical challenges. For patients who develop neurologic symptoms or overlapping systemic complications, referral to other specialties may be necessary.
For example, a patient with skin lesions and new cognitive symptoms may be evaluated for cerebral spread, much like patients being screened for brain cancer in cats —emphasizing how changes in skin can be a window into broader systemic pathology.
This collaborative approach ensures that treatment is not only medically effective but also holistic, addressing every aspect of a patient’s experience—from pain to appearance to emotional wellness.
Can Skin Metastases Be Prevented?
Preventing skin metastases specifically is difficult, as they are typically a sign of systemic disease. However, early and aggressive treatment of primary breast cancer remains the best strategy to delay or prevent metastasis. This includes routine screening (like mammography), prompt evaluation of any suspicious symptoms, and adherence to recommended therapies.
Patients in remission should maintain regular follow-ups and self-examinations. Any new skin lesion—especially in or around the chest wall—should prompt immediate attention. While some recurrences are inevitable due to tumor biology, others may be caught early and managed effectively with minimal spread.
Ongoing surveillance is particularly important in those with prior high-risk features, including lymphovascular invasion, node-positive disease, or aggressive subtypes like inflammatory breast cancer. Patient education remains a cornerstone of recurrence monitoring.
Emerging Research and Future Directions
Research into skin metastases from breast cancer is expanding, particularly in the areas of targeted therapy, immunotherapy, and genetic profiling. New monoclonal antibodies and antibody-drug conjugates (like trastuzumab deruxtecan) have shown promise in managing HER2-positive cutaneous metastases, with some achieving durable responses.
Other trials are evaluating the role of checkpoint inhibitors in patients with triple-negative disease, while genomic sequencing may help identify which patients are at highest risk for skin involvement. Researchers are also investigating topical and intralesional therapies for localized disease control, aiming to provide better options for those who cannot tolerate systemic regimens.
Artificial intelligence and machine learning are being applied to imaging and pathology to better detect subtle skin changes and predict metastatic behavior. These innovations could eventually allow earlier intervention and improved outcomes.
Importantly, cutaneous metastases are also being recognized as a marker in clinical trial stratification, acknowledging their physical, emotional, and prognostic impact. As awareness grows, patients can hope for treatments that are not only more effective but also more humane.
FAQ – Frequently Asked Questions about Breast Cancer Metastasis to the Skin
What are the first signs that breast cancer has spread to the skin?
The earliest signs often include firm, painless nodules or plaques on or near the chest wall, mastectomy scar, or in distant areas like the back or scalp. These lesions may appear reddish, flesh-colored, or even purplish, and unlike common skin rashes, they typically do not respond to topical creams or antibiotics.
Is skin metastasis a sign that breast cancer is terminal?
Not necessarily, but it does indicate stage IV cancer, which is considered advanced. The presence of skin metastases means the cancer has spread beyond the breast, but many patients can still achieve months or even years of quality life with the right treatment approach.
Can skin metastases appear even after mastectomy?
Yes. In fact, recurrence along the mastectomy scar is a common presentation of skin metastasis. Cancer cells can remain dormant for years and reappear in the skin, especially in the absence of systemic follow-up treatments or surveillance.
How is skin metastasis from breast cancer diagnosed?
Diagnosis typically requires a skin biopsy, where a sample of the lesion is removed and analyzed under a microscope. Additional imaging, such as PET-CT or MRI, helps determine the full extent of metastatic spread and informs treatment decisions.
Are skin metastases painful or itchy?
They can be, especially as they grow or ulcerate. While many begin as painless nodules, over time they may cause discomfort, itching, burning, or even bleeding. Some patients also report tightness or restricted movement if lesions are located near joints.
Can radiation therapy be used to treat skin metastases?
Yes. Radiation is commonly used for localized control of painful or ulcerated skin lesions. It may reduce tumor burden, ease symptoms, and delay further spread in certain regions, especially when systemic therapy is not sufficient alone.
How fast do skin metastases grow?
Growth rates vary depending on the cancer subtype and the effectiveness of treatment. Aggressive tumors like triple-negative breast cancer tend to progress more rapidly, while hormone receptor-positive types may evolve more slowly over months or even years.
Do all breast cancer patients eventually develop skin metastases?
No, most breast cancer patients do not experience skin metastasis. It is more common in those with advanced disease, high-risk tumor biology, or recurrence. It remains a relatively rare but serious manifestation.
Can skin metastases be removed surgically?
In select cases, yes. Surgical removal may be an option for small, isolated lesions that are causing discomfort or infection. However, surgery is usually combined with systemic treatment and is not considered curative for metastatic disease.
What’s the difference between inflammatory breast cancer and skin metastases?
Inflammatory breast cancer originates within the breast and involves skin changes due to lymphatic blockage, while skin metastases represent distant spread of cancer cells to the dermis. Both can cause redness and swelling but have different prognoses and treatment paths.
Can skin metastases occur without any other metastases?
Yes, though it’s uncommon. Some patients may present with cutaneous-only metastases, especially early in metastatic progression. However, further evaluation is always necessary to rule out internal involvement.
Is there a link between skin lesions and recurrence after remission?
Absolutely. Skin metastases may be the first visible sign of breast cancer recurrence, even years after remission. Any new lesion in a previously treated area should be evaluated with suspicion for possible recurrence.
What’s the prognosis for patients with skin metastases only?
Prognosis varies. Some patients with skin-only metastases respond well to systemic therapies and may live for several years. However, others may experience rapid progression, especially if additional organ involvement develops over time.
Are there any lifestyle changes that can help manage skin metastases?
While lifestyle changes cannot reverse skin metastases, proper skin hygiene, wound care, and nutrition can support overall health and improve tolerance to treatment. Emotional support and mental wellness practices are also beneficial.
Do skin metastases always indicate failure of previous treatment?
Not always. Cancer can adapt and evolve despite previous therapies. Skin metastases may arise as part of natural disease progression, particularly in aggressive subtypes, rather than due to a direct failure of earlier interventions.












