When Breast Cancer Spreads to the Liver: Symptoms, Treatments, and Hope
- What Does Liver Metastasis Mean in Breast Cancer?
- Early Warning Signs and Symptoms of Liver Metastasis
- How Breast Cancer Reaches the Liver
- How It’s Diagnosed: Imaging, Blood Tests, and Biopsy
- How Doctors Classify the Extent of Liver Involvement
- Treatment Overview: Local and Systemic Approaches
- Liver Function Impact and How It Shapes Treatment
- Comparison of Metastasis Sites in Breast Cancer
- Symptoms That May Signal Liver Failure
- Living With Stage IV Breast Cancer: Emotional and Physical Realities
- The Role of Genetic Markers in Treatment Planning
- Understanding Prognosis and Survival Rates
- When Surgery Is an Option for Liver Metastases
- How Clinical Trials Are Expanding Treatment Possibilities
- Caregiver Support and Decision-Making During Progression
- Comparing Liver Metastasis Outcomes With Other Cancer Types
- Frequently Asked Questions (FAQ)

What Does Liver Metastasis Mean in Breast Cancer?
When breast cancer metastasizes to the liver, it signifies that cancer cells have broken away from the original tumor in the breast, traveled through the bloodstream or lymphatic system, and lodged themselves in liver tissue. These cells don’t transform into liver cancer—they remain biologically breast cancer, which is crucial for determining treatment. This condition is considered stage IV or advanced metastatic breast cancer, indicating that the disease is now systemic rather than localized.
Liver metastases may occur months or even years after initial treatment for breast cancer, sometimes during remission. In other cases, liver involvement may be detected during a recurrence or at the time of first diagnosis. Because of its extensive blood supply and detoxification role, the liver is one of the most common sites for secondary tumor development, alongside the lungs, bones, and brain. The presence of liver metastases changes the overall treatment strategy, shifting the focus from cure to long-term control, quality of life, and management of organ function.
Early Warning Signs and Symptoms of Liver Metastasis
Liver metastases often begin silently, without noticeable symptoms. That’s why regular imaging and bloodwork are crucial for breast cancer survivors—even those in remission. However, as the tumor burden in the liver grows, clinical symptoms typically begin to emerge.
One of the earliest signs is unexplained fatigue. Patients often report feeling exhausted even after adequate rest. This fatigue is due in part to the liver’s role in detoxification and energy regulation, which becomes impaired when tumor cells disrupt its function. Another common symptom is right-sided abdominal discomfort or pain, sometimes described as a dull ache or a sensation of pressure under the rib cage.
Jaundice—a yellowing of the skin and whites of the eyes—can develop if tumors block the liver’s bile ducts. This is often accompanied by dark-colored urine and pale stools, indicating a problem with bile flow. Loss of appetite, nausea, unexplained weight loss, and fluid buildup (ascites) in the abdomen are also possible. These symptoms may progress gradually or come on more suddenly in aggressive subtypes.
How Breast Cancer Reaches the Liver
Breast cancer spreads through a process called hematogenous dissemination, in which cancer cells invade blood vessels near the tumor and travel through the circulatory system. Because the liver filters a large volume of blood—especially from the digestive tract and abdominal region—it becomes a natural landing zone for these wandering malignant cells.
Once in the liver, the cancer cells can survive and begin to divide, forming colonies. This ability to colonize new tissue depends on both the biology of the cancer cells and the environment of the liver. Tumors that are HER2-positive or triple-negative often spread more aggressively. Additionally, a compromised immune system or genetic mutations in the tumor may allow these cells to evade destruction and take root.
The process is influenced by microscopic factors like chemokines and adhesion molecules, which help cancer cells stick to the liver’s interior and attract new blood vessels to feed the growing tumors (angiogenesis). Although the spread is invisible at first, these micrometastases can later grow into large, detectable lesions.
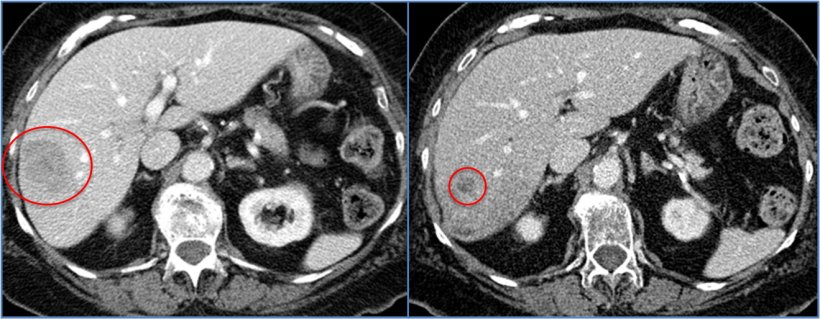
How It’s Diagnosed: Imaging, Blood Tests, and Biopsy
Diagnosing liver metastases begins with clinical suspicion—usually triggered by new symptoms or abnormal blood tests. One of the most common early clues is a rise in liver enzymes such as ALT (alanine aminotransferase), AST (aspartate aminotransferase), and ALP (alkaline phosphatase), which may indicate liver irritation or dysfunction. Elevated bilirubin levels or abnormal albumin and coagulation values also point toward liver involvement.
If laboratory results are concerning, imaging studies are the next step. A CT scan of the abdomen provides detailed images and can detect even small lesions in the liver. MRI offers even greater sensitivity, especially for distinguishing between benign liver cysts and malignant tumors. For detecting metabolic activity, PET scans (positron emission tomography) can show areas where glucose uptake is unusually high—often a sign of active cancer.
When imaging alone is not conclusive, a liver biopsy may be recommended. In this procedure, a small tissue sample is extracted—usually under ultrasound or CT guidance—and examined under a microscope. This allows doctors to confirm that the cancer cells in the liver share the same characteristics (e.g., hormone receptors, HER2 status) as the primary breast tumor. Biopsy also rules out other potential liver lesions, like primary liver cancer or infections.
How Doctors Classify the Extent of Liver Involvement
Once liver metastasis is confirmed, the next step is to assess the extent of spread. Oncologists consider several key factors: how many lesions are present, their size, whether they are confined to one lobe or spread across both, and how deeply they penetrate into the liver’s vascular system.
A patient with one or two small, localized tumors may have a very different treatment plan than someone with diffuse, multifocal involvement. The presence of tumors in both lobes of the liver often limits surgical or ablative treatment options, shifting the focus to systemic therapy. Some doctors use descriptive terms like “oligometastatic” (limited number of metastases) versus “widespread” to communicate these differences.
Additionally, liver function status plays a central role. Even if the tumor burden is moderate, impaired liver function can limit chemotherapy choices or increase the risk of toxicity. Monitoring liver-related markers and using scoring systems like Child-Pugh or MELD (though more common in liver cirrhosis) may help guide decisions about aggressiveness of care and expected outcomes.
Treatment Overview: Local and Systemic Approaches
Treating breast cancer that has spread to the liver requires a systemic plan, as the disease is no longer confined to a single organ. Hormonal therapy is often used for hormone receptor-positive cancers, while HER2-positive tumors respond to targeted treatments like trastuzumab or pertuzumab. Chemotherapy may be used alone or in combination, especially for triple-negative breast cancers. Local treatments include radiofrequency ablation (RFA), transarterial chemoembolization (TACE), or even surgical resection in highly selected cases. These methods target liver lesions directly and may be considered when the disease is stable or responds well to systemic therapy.
Liver Function Impact and How It Shapes Treatment
The liver plays a vital role in metabolizing chemotherapy and maintaining nutrient balance. When it’s compromised by tumor growth, standard treatments may need to be modified or delayed. Elevated bilirubin levels, poor clotting ability, or signs of hepatic encephalopathy may indicate the liver is under stress. Doctors use blood tests like ALT, AST, ALP, and bilirubin to monitor liver function throughout treatment. Managing side effects and preserving liver health becomes just as critical as controlling tumor progression.
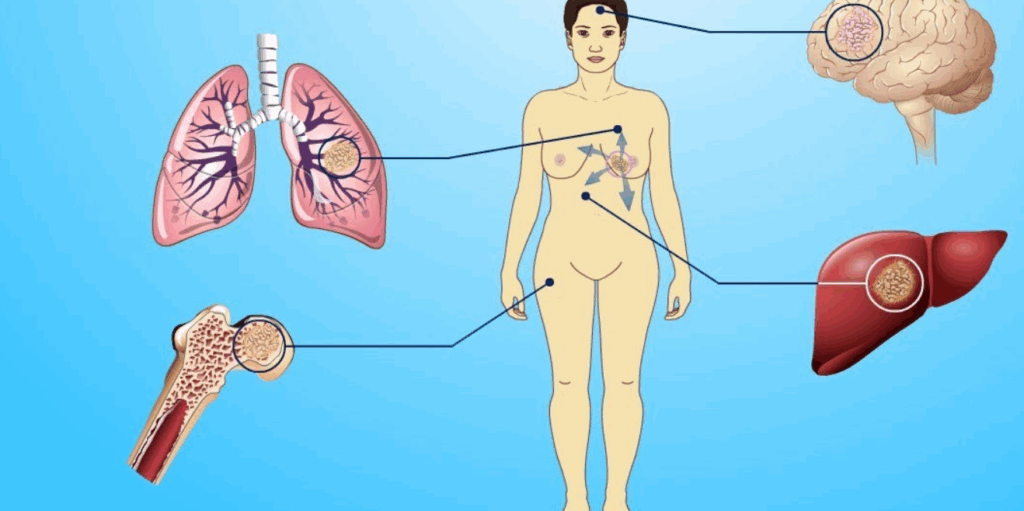
Comparison of Metastasis Sites in Breast Cancer
The liver is just one of several common sites for breast cancer metastasis. Below is a table comparing how metastasis affects different organs:
| Metastasis Site | Common Symptoms | Typical Treatments | Impact on Survival |
| Liver | Fatigue, jaundice, abdominal pain | Chemo, targeted therapy, local ablation | Moderate to significant |
| Lungs | Cough, shortness of breath, chest pain | Chemo, radiation, targeted therapy | Moderate |
| Bones | Pain, fractures, high calcium levels | Bisphosphonates, radiation, chemo | Often long-term management possible |
| Brain | Headaches, seizures, confusion | Radiation, steroids, targeted agents | More serious; often affects function |
Brain cancer in dogs – as a comparison of oncological processes in the brain and their symptoms.
Symptoms That May Signal Liver Failure
As liver metastasis progresses, it can impair the organ’s ability to filter toxins, produce proteins, and store nutrients. This dysfunction may manifest in several ways: jaundice is often one of the clearest signs, caused by the liver’s inability to process bilirubin. Ascites (fluid buildup in the abdomen) may cause noticeable swelling and discomfort. Other signs include confusion, irritability, or excessive drowsiness, which may point to hepatic encephalopathy—a condition where toxins affect brain function. These symptoms often emerge in advanced stages and require urgent medical attention to stabilize liver performance.
Living With Stage IV Breast Cancer: Emotional and Physical Realities
A diagnosis of liver metastasis changes the trajectory of breast cancer from curative to chronic care. Many patients can live for years with stable disease under proper treatment, but the emotional impact is profound. Fatigue, digestive discomfort, and medication side effects become part of daily life. Patients often describe feeling caught between managing symptoms and trying to maintain normalcy. Emotional support—whether through counseling, support groups, or spiritual care—can make a measurable difference. Bowel cancer stomach noises, as an example of another complex form of cancer where abnormal bodily signals may be a symptom.
The Role of Genetic Markers in Treatment Planning
Breast cancer is increasingly being treated based on its molecular and genetic profile. If the metastasized cells in the liver still express hormone receptors (ER/PR) or HER2 proteins, targeted therapy options remain viable. In recent years, genomic testing has identified mutations like PIK3CA, BRCA1/2, and ESR1 that can guide personalized treatment. Liquid biopsies, which analyze tumor DNA in the blood, now help monitor treatment response without repeated invasive scans. The more tailored the approach, the more likely it is that liver metastases can be stabilized long term.
Understanding Prognosis and Survival Rates
While a diagnosis of breast cancer with liver metastasis is serious, it is not always immediately terminal. Prognosis depends on several factors, including cancer subtype, number of liver lesions, response to treatment, and liver function status. For example, patients with hormone receptor-positive, HER2-negative tumors that respond well to hormonal therapy may live for several years post-diagnosis. By contrast, triple-negative breast cancer that spreads aggressively may be more difficult to control. Advances in systemic therapies and liver-directed treatments continue to improve outcomes year by year.
When Surgery Is an Option for Liver Metastases
Surgical resection of liver metastases from breast cancer is rare but possible in specific scenarios. Candidates are typically those with a limited number of lesions confined to one part of the liver, stable disease elsewhere, and excellent response to systemic therapy. In these cases, removing the liver tumors can significantly prolong survival and, in rare instances, achieve long-term remission. However, surgery carries risks, especially in a liver already under stress from cancer or chemotherapy. Multidisciplinary teams must evaluate resectability carefully, weighing the potential benefits against postoperative complications.
How Clinical Trials Are Expanding Treatment Possibilities
Many patients with liver metastases are now turning to clinical trials for access to next-generation therapies. These studies test innovative treatments such as antibody-drug conjugates, immunotherapies, and new forms of targeted radiation. Participating in a clinical trial can be an opportunity to receive cutting-edge care before it becomes widely available. Eligibility depends on cancer subtype, prior treatments, and overall health. Discussing clinical trial options with your oncologist early on can open the door to additional treatment pathways when standard options plateau.
Caregiver Support and Decision-Making During Progression
As liver metastases progress, caregiving needs often intensify. Family members may need to assist with meals, medications, mobility, and emotional support. Open conversations about the patient’s wishes—especially regarding quality of life, emergency care, or palliative transitions—help reduce anxiety and uncertainty. Hospice care may eventually be discussed, focusing on comfort, dignity, and pain control. Caregivers, too, need support and rest. In fact, acknowledging the emotional toll on those around the patient is essential for sustaining long-term care at home or in specialized facilities.
Comparing Liver Metastasis Outcomes With Other Cancer Types
While breast cancer is a common primary source of liver metastasis, it’s not the only one. Colorectal, pancreatic, and lung cancers frequently spread to the liver, often with different trajectories. Interestingly, metastatic behavior in animals—like in [brain cancer in cats](по-русски — здесь вставляется ссылка) or dogs—also shows that once cancer reaches the liver or brain, clinical symptoms shift significantly. By examining these cross-species patterns, researchers continue to uncover broader truths about how tumors interact with vital organs and how metastasis changes everything from treatment dynamics to survival expectations.
Frequently Asked Questions (FAQ)
What does it mean when breast cancer spreads to the liver?
It means that cancer cells from the breast have traveled through the bloodstream or lymphatic system and formed tumors in the liver. These metastatic cells are still breast cancer in origin, which affects how they are treated and classified.
Is liver metastasis from breast cancer a death sentence?
Not necessarily. While liver metastasis indicates stage IV cancer, many patients live for years with stable disease thanks to modern treatments. Survival depends on cancer type, response to therapy, and liver function.
What symptoms suggest breast cancer has reached the liver?
Common symptoms include fatigue, upper abdominal pain, nausea, weight loss, yellowing of the skin or eyes (jaundice), and dark urine. Some people may also develop fluid buildup in the belly or changes in mental clarity.
How is liver metastasis diagnosed in someone with breast cancer?
Diagnosis usually involves blood tests showing abnormal liver enzymes, followed by imaging like CT, MRI, or PET scans. A biopsy may be done to confirm that liver lesions are metastatic breast cancer.
Can liver metastases be treated with surgery?
Surgery is only an option for a small number of patients. It’s considered when liver involvement is limited, the rest of the disease is stable, and the tumors are resectable. Most patients receive systemic treatment instead.
What systemic treatments are used for liver metastases?
Hormonal therapy, chemotherapy, targeted agents (like trastuzumab for HER2-positive tumors), and immunotherapy may all be used. Treatment depends on the tumor’s biology and how well the liver is functioning.
Can liver metastases be completely cured?
While rare, long-term remission is possible in patients with limited disease who respond exceptionally well to treatment. However, in most cases, the focus is on long-term disease management rather than cure.
Does liver damage affect treatment options?
Yes. The liver metabolizes many drugs. If liver function is impaired, some treatments may need to be reduced, adjusted, or avoided altogether. This is why regular monitoring of liver function is essential during therapy.
What is the average survival time with breast cancer liver metastases?
Average survival varies. Some patients live 2–5 years or more with proper treatment. Those with aggressive tumors or poor liver function may have a shorter prognosis. The range is wide and highly individualized.
How fast do liver metastases grow?
Growth rate depends on the type of breast cancer. Triple-negative tumors may grow rapidly, while hormone-positive tumors often progress more slowly. Imaging every few months helps track disease activity.
Are there clinical trials for liver metastases from breast cancer?
Yes. Trials are testing new drugs, combinations, and precision therapies. These may offer hope when standard treatments are no longer effective. Your oncologist can help identify if you’re a candidate.
What is the role of palliative care?
Palliative care focuses on quality of life—managing pain, nausea, and fatigue. It can be provided alongside active cancer treatment and becomes especially important if curative treatment is no longer viable.
Can diet or lifestyle changes help with liver metastases?
While they can’t reverse metastasis, a healthy diet and reduced alcohol intake support overall liver health. Staying active within comfort limits, managing stress, and avoiding toxins can help maintain resilience.
How do doctors know if treatment is working?
Doctors monitor changes through regular imaging (MRI, CT, or PET scans), liver function tests, and physical assessments. Tumor shrinkage or stability is a sign of response, while new symptoms may prompt treatment reassessment.
When should someone consider hospice care?
Hospice may be considered when treatment stops controlling the disease or when side effects outweigh benefits. It focuses on comfort, dignity, and emotional support at the end of life, tailored to the patient’s wishes.









