What a Dry Cough at Night Means and When to See a Doctor
Why a Dry Cough Gets Worse at Night
A dry cough at night is a nonproductive cough that does not bring up mucus or phlegm. It often feels like a tickle or irritation in the throat or upper airways. This type of cough results from inflammation or hypersensitivity of the cough reflex, which can become more pronounced during sleep. Many people notice their symptoms intensify after lying down, disrupting rest and sometimes persisting despite minimal daytime coughing.
What Happens When You Lie Down
When the body moves into a horizontal position during sleep, gravity no longer helps clear mucus from the upper airways. This change allows secretions from the nose or sinuses to accumulate in the back of the throat, known as postnasal drip. The resulting irritation stimulates cough receptors in the pharynx and larynx, leading to bouts of nighttime coughing. Reduced gravitational drainage means even small amounts of mucus or inflammation can trigger repeated cough reflexes, especially in people with sensitive airways.
- Reduced gravitational drainage increases postnasal drip.
- Mucus accumulation irritates throat and airway receptors.
- Dry airflow and minor inflammation can trigger persistent coughing.
Additionally, airflow dynamics in the supine position may alter how air passes through the throat, slightly increasing dryness or tickling sensations that prompt a cough. This combination of mucus pooling and airway irritation explains why nighttime dry cough can persist even in the absence of infection.
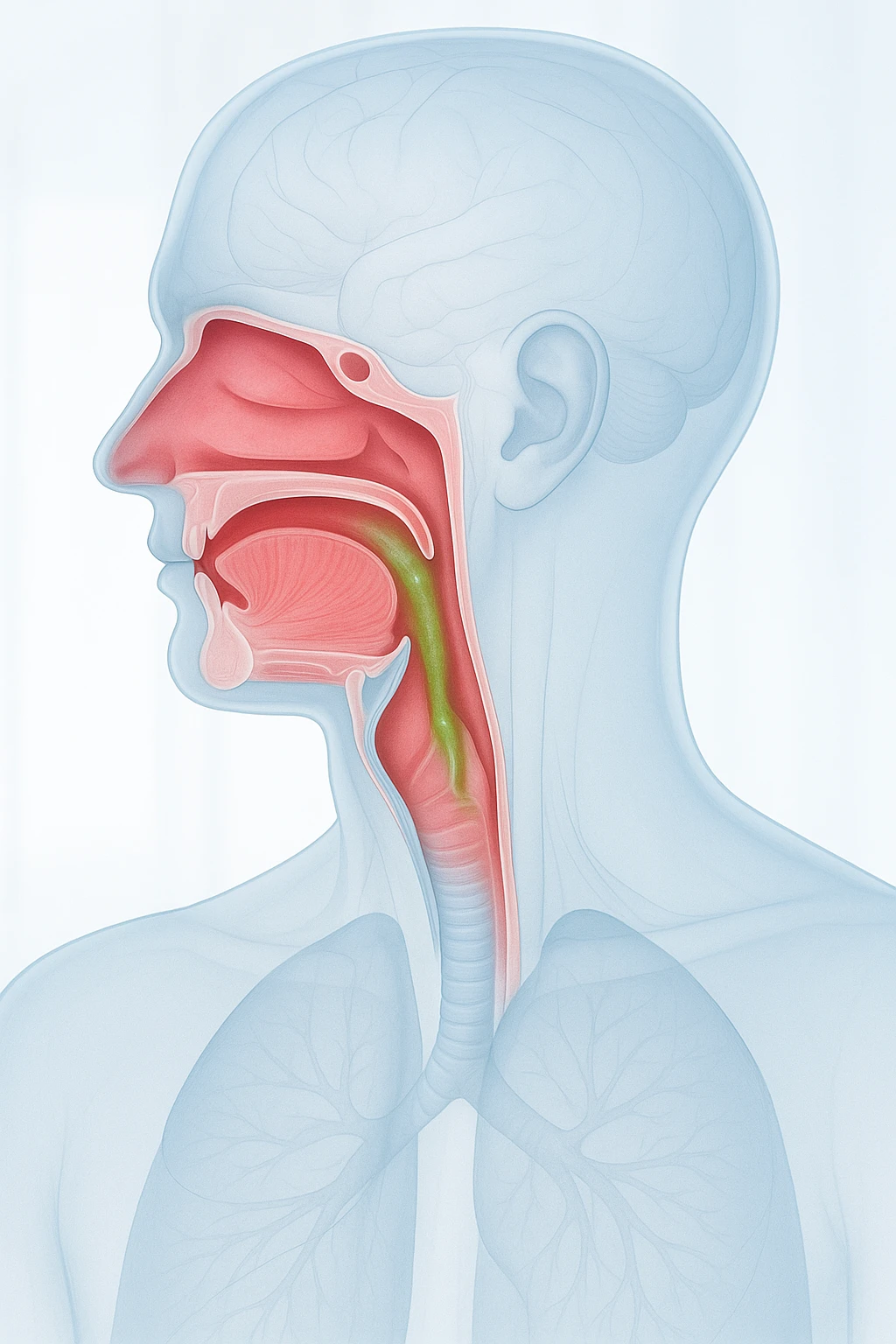
Reflux and Sensitivity of the Cough Reflex
Another frequent reason a dry cough worsens at night is gastroesophageal reflux. When lying flat, acid from the stomach can travel upward into the esophagus and sometimes reach the throat. This process, called laryngopharyngeal reflux, irritates the lining of the throat and activates cough receptors. Even small, repeated reflux episodes may produce significant coughing without noticeable heartburn.
- Reflux allows acid to reach the throat more easily when lying down.
- Throat irritation triggers cough receptors even without heartburn.
- Repeated irritation increases cough reflex sensitivity.
Over time, repeated reflux or postnasal secretions can heighten cough reflex sensitivity. The nerves responsible for triggering a cough may become overreactive, responding to minimal stimulation such as temperature changes or dryness. This reflex hypersensitivity helps explain why nocturnal coughing can continue even after the original trigger has resolved.
Major Respiratory Causes of Nighttime Dry Cough
Several respiratory conditions can cause a dry cough at night. These disorders share a common feature: airway irritation or inflammation that worsens when lying down or during sleep. Understanding these mechanisms helps explain why nocturnal coughing can persist even without infection or mucus production.
Postnasal Drip and Upper Airway Inflammation
Upper airway cough syndrome, also known as postnasal drip, is among the most frequent causes of nighttime cough. In this condition, excess mucus from the nasal passages or sinuses drips into the throat, especially when lying down. The constant trickling of mucus irritates the throat and activates cough receptors, leading to persistent dry coughing during sleep.
- Occurs more frequently when lying flat due to mucus drainage into the throat.
- Often linked with allergic rhinitis, sinusitis, or environmental irritants.
- Produces a dry, tickling cough rather than chest congestion.
Asthma and Eosinophilic Conditions
Asthma is another major cause of nocturnal coughing. The airways in asthma are hypersensitive and can narrow in response to triggers such as allergens or temperature changes. At night, natural circadian rhythms cause mild airway constriction, which can worsen existing inflammation. As a result, patients may experience coughing, wheezing, or shortness of breath after going to bed or in the early morning.
- Asthma symptoms often worsen at night due to circadian airway narrowing.
- Common symptoms: coughing, wheezing, or early-morning breathlessness.
- Nonasthmatic eosinophilic bronchitis causes dry cough without wheezing or obstruction.
Nonasthmatic eosinophilic bronchitis presents similarly to asthma but without airway narrowing. It involves inflammation dominated by eosinophils, a type of white blood cell. Both conditions emphasize the role of airway inflammation and hypersensitivity in producing nocturnal cough.
Environmental Triggers
Environmental factors in the bedroom can also contribute to nighttime dry cough. Common irritants include dust, pet dander, smoke, or low humidity, all of which can inflame the respiratory mucosa. People with allergies or sensitive airways are particularly vulnerable. Even small amounts of airborne irritants can sustain nighttime coughing, especially in poorly ventilated rooms.
- Dust and pet dander often accumulate in bedding and carpets.
- Dry air or smoke exposure worsens airway irritation.
- Proper ventilation and allergen control can help reduce symptoms.
Other Medical Causes Beyond the Airways
While most cases of dry cough at night begin in the respiratory tract, several non-respiratory conditions can also provoke or worsen this symptom. These include gastrointestinal reflux, medication side effects, and cardiovascular problems that affect how the lungs function during rest.
Reflux-Related Cough
Gastroesophageal reflux disease (GERD) is a frequent non-respiratory cause of nocturnal dry cough. When lying flat, stomach acid can flow backward into the esophagus and upper airway. This backflow, known as microaspiration, irritates the throat and stimulates cough receptors. Even without heartburn, reflux irritation can cause persistent coughing through both chemical injury and vagal reflexes.
- Acid reflux irritates the throat and upper airway, even without heartburn.
- Microaspiration and vagal reflexes trigger nocturnal coughing.
- Repeated reflux episodes heighten cough reflex sensitivity.
Medication-Related and Cardiac Causes
Medications such as ACE inhibitors, used for blood pressure control, can cause a persistent dry cough that is sometimes worse at night. This effect results from heightened cough reflex sensitivity caused by peptide accumulation in the airways. The cough usually resolves once the medication is changed under medical supervision.
- ACE inhibitors may cause a chronic, dry, often nocturnal cough.
- Mechanism involves increased airway sensitivity.
- Symptoms improve after adjusting or discontinuing the medication.
Left-sided heart failure is another systemic cause of nighttime cough. When cardiac function declines, fluid can accumulate in the lungs (pulmonary congestion). Lying down redistributes this fluid, irritating the airways and triggering coughing, often accompanied by shortness of breath. Recognizing this pattern is crucial, as it signals a need for prompt cardiovascular assessment.
- Heart failure causes pulmonary congestion and airway irritation.
- Cough appears with shortness of breath when lying down.
- Indicates possible cardiac dysfunction needing evaluation.
How Clinicians Evaluate Persistent Nighttime Cough
When a dry cough at night persists for several weeks, clinicians conduct a structured evaluation to identify the cause. The aim is to distinguish mild, self-limiting cases from those signaling respiratory, gastrointestinal, or cardiovascular disease. A detailed medical history and physical examination guide appropriate testing.
Clinical Assessment and Key Questions
During evaluation, clinicians assess cough duration, timing, and pattern. They ask about nighttime triggers such as lying down, reflux, or allergen exposure. Patients are questioned about medication use, environmental conditions, and associated symptoms like wheezing or shortness of breath. These details help pinpoint whether asthma, reflux, or airway irritation is likely.
- Timing and pattern of cough (e.g., after lying down, early morning)
- Potential triggers: allergens, medications, environmental factors
- Associated symptoms: reflux, wheezing, or shortness of breath
- Medication review, including ACE inhibitors or other agents
- Smoking history or occupational exposures
Diagnostic Tests and Red Flags
Testing depends on findings from the initial assessment. Common tests include chest imaging to rule out infection, spirometry to check for asthma, and pH monitoring or endoscopy to confirm reflux. Allergy testing may also help identify triggers that worsen nocturnal cough.
| Test or Assessment | Purpose |
|---|---|
| Chest X-ray / Imaging | Detect infection or structural abnormalities |
| Spirometry | Assess airway obstruction or asthma |
| pH monitoring / Endoscopy | Identify reflux-related causes |
| Allergy testing | Determine environmental or allergenic triggers |
Red flags that require urgent medical attention include coughing up blood, chest pain, unexplained weight loss, or significant shortness of breath. These symptoms may indicate serious underlying disease and should be evaluated promptly.
When to See a Doctor
- Cough lasting longer than three weeks
- Nighttime cough disrupting sleep
- Chest discomfort, wheezing, or shortness of breath
- Unexplained weight loss or coughing up blood
Early assessment allows for targeted treatment and helps prevent chronic airway irritation or complications from undiagnosed conditions.
Relief, Prevention, and Long-Term Management of Dry Cough at Night
Effective management of a dry cough at night focuses on identifying and treating the root cause while reducing symptom burden and improving sleep quality. Because nocturnal coughing may arise from respiratory, gastrointestinal, or systemic conditions, therapy must be tailored to the individual rather than limited to cough suppression alone. Early diagnosis and appropriate intervention can prevent chronic cough cycles and associated airway irritation.
Targeted Medical Treatment
Treatment strategies are directed at the underlying cause. For upper airway conditions such as allergic rhinitis or sinus inflammation, antihistamines or nasal corticosteroids may reduce postnasal drip. Asthma-related cough improves with inhaled corticosteroids or bronchodilators, which reduce airway inflammation and hyperreactivity. If gastroesophageal reflux is involved, acid suppression and dietary management are central to symptom control. When cough is medication-induced, clinicians may review current prescriptions and substitute or adjust the offending drug, such as discontinuing ACE inhibitors under supervision.
- Allergic rhinitis or sinus inflammation: antihistamines or nasal corticosteroids
- Asthma-related cough: inhaled corticosteroids or bronchodilators
- Reflux-associated cough: acid suppression and dietary adjustment
- Medication-induced cough: clinician review and modification of therapy
Symptomatic relief measures such as adequate hydration or using a humidifier in dry environments may provide temporary comfort but should complement-not replace-treatment of the primary cause. This multifaceted approach ensures both short-term relief and long-term resolution.
Environmental and Lifestyle Adjustments
Behavioral and environmental modifications play an important role in reducing nighttime cough. Elevating the head of the bed helps limit reflux-related irritation by keeping stomach acid from reaching the throat. Minimizing bedroom irritants such as dust, pet dander, and smoke can reduce airway inflammation and improve nighttime breathing. Maintaining moderate humidity levels also prevents dryness that can trigger coughing episodes.
- Elevate the head of the bed to reduce reflux irritation.
- Reduce exposure to dust, pet dander, and smoke in the bedroom.
- Maintain comfortable humidity to prevent airway dryness.
- Avoid heavy meals or alcohol before bedtime.
Regular sleep routines and avoidance of heavy meals or alcohol before bedtime can further reduce cough-provoking stimuli. Together, these simple adjustments support medical treatment and improve sleep quality in individuals with recurrent nocturnal cough.
Prognosis and Preventive Care
Most causes of dry cough at night respond well once the underlying condition is addressed, with symptom improvement typically occurring within weeks of targeted therapy. Persistent or worsening cough despite treatment warrants re-evaluation to rule out less common or serious etiologies. Recognizing early warning signs-such as persistent breathlessness, chest pain, or swelling of the legs-should prompt timely medical assessment to exclude cardiac or systemic disorders.
- Improvement expected within weeks after addressing the underlying cause.
- Seek re-evaluation for persistent or worsening symptoms.
- Monitor for warning signs such as breathlessness, chest pain, or leg swelling.
Proactive management and follow-up care help prevent chronic airway hypersensitivity and maintain respiratory health. Addressing triggers early not only relieves discomfort but also reduces the likelihood of recurrence and associated sleep disruption.
Frequently Asked Questions About Dry Cough at Night
- Why does my dry cough get worse when I go to bed?
- Lying flat can cause mucus or acid reflux to irritate the throat, making coughing more frequent at night. Gravity also reduces drainage from the upper airways.
- Can acid reflux really cause a nighttime cough even without heartburn?
- Yes. Stomach acid can reach the throat through silent reflux, irritating the vocal cords and activating cough receptors during sleep.
- Is it normal for asthma symptoms to worsen at night?
- Asthma often flares at night because airway inflammation and narrowing increase during sleep. This natural rhythm can trigger coughing or wheezing in sensitive individuals.
- What role do allergies play in a dry cough at night?
- Allergens such as dust mites or pet dander commonly found in bedding can irritate the airways. Keeping the bedroom clean and well-ventilated may lessen irritation.
- Could my medication be causing my nighttime cough?
- Some blood pressure medicines, particularly ACE inhibitors, can trigger a persistent dry cough that is more noticeable at night. Adjusting medication should be discussed with a clinician.
- When should a nighttime cough be considered serious?
- If the cough lasts longer than three weeks or is accompanied by shortness of breath, chest pain, or swelling, it should be medically evaluated.
- How does heart failure cause coughing during sleep?
- In left-sided heart failure, fluid may build up in the lungs when lying down. This fluid irritates the airways, causing a dry cough and breathlessness at night.
- Are there home adjustments that help reduce nocturnal coughing?
- Elevating the head of the bed, maintaining moderate humidity, and avoiding heavy meals before sleep can help minimize reflux and airway irritation.
- Why does my throat feel dry or tickly when I lie down?
- Airflow changes and mouth breathing at night can dry the throat, making the cough reflex more sensitive and triggering a tickling sensation.
- Can a dry cough at night go away on its own?
- It may resolve once the underlying cause, such as postnasal drip, reflux, or allergies, is treated. Persistent or worsening symptoms should always be assessed by a healthcare provider.