Vocal Cord Cancer
Vocal Cord Cancer: What You Need to Know
- What Is Vocal Cord Cancer?
- Common Symptoms and Warning Signs
- Understanding the Causes and Risk Factors
- Staging Vocal Cord Cancer: What It Means
- Diagnostic Process: How Vocal Cord Cancer Is Detected
- Primary Treatment Modalities for Vocal Cord Cancer
- Life After Treatment: Recovery and Rehabilitation
- Managing Voice Loss and Prosthetic Solutions
- Emotional and Psychological Impact of Vocal Cord Cancer
- Long-Term Monitoring and Follow-Up Care
- Common Misdiagnoses and Delays in Diagnosis
- Risk Factors and Preventive Actions
- Role of Genetics and Family History in Vocal Cord Cancer
- Reconstructive Surgery and Voice Rehabilitation
- Understanding the Role of HPV in Vocal Cord Cancer
- When Vocal Cord Cancer Spreads: Metastasis and Advanced Management
- 15+ FAQ: Vocal Cord Cancer
What Is Vocal Cord Cancer?

Vocal cord cancer is a type of laryngeal cancer that originates in the tissues of the vocal cords, located within the voice box (larynx) in the throat. These cords are responsible for sound production and are vital for speech, breathing, and swallowing. Most vocal cord cancers are squamous cell carcinomas, meaning they begin in the flat, thin cells lining the throat.
This cancer typically develops slowly and is often detected early because of noticeable voice changes. It may appear as a small lesion, ulcer, or lump directly on the vocal cords. While vocal cord cancer is considered rare compared to other cancers, early diagnosis dramatically improves the outcome.
From a clinical perspective, vocal cord cancer is a subset of laryngeal cancer, which is itself a category within head and neck cancers. It’s important to distinguish between cancers of the vocal cords and other parts of the larynx, as treatment options and prognosis can differ significantly.
Common Symptoms and Warning Signs
Vocal cord cancer symptoms often present early, especially when the tumor is located on the true vocal cords. The most recognizable symptom is persistent hoarseness that doesn’t resolve within two weeks. Because the vocal cords vibrate to produce sound, any structural disruption — even a small tumor — may cause noticeable changes in voice.
Additional warning signs include:
- A sore throat or feeling of something stuck in the throat
- Pain when speaking or swallowing
- Ear pain (referred otalgia)
- Persistent cough or coughing up blood
- Difficulty breathing or noisy breathing (stridor)
- Lump in the neck if the cancer has spread to lymph nodes
It’s essential to understand that these symptoms may also be caused by benign conditions such as laryngitis or vocal nodules. However, persistent or worsening symptoms warrant immediate medical evaluation.
Understanding the Causes and Risk Factors
Vocal cord cancer, like many malignancies, develops due to genetic mutations that cause cells to grow uncontrollably. While the exact triggers can vary, several risk factors increase the likelihood of developing this cancer:
- Tobacco use: The most significant and well-established risk factor. Both smoking and smokeless tobacco directly damage laryngeal cells.
- Excessive alcohol consumption: Often acts synergistically with tobacco to raise risk.
- HPV infection: Certain strains of the human papillomavirus, particularly HPV-16, have been linked to vocal cord and other head and neck cancers.
- Chronic acid reflux: Gastroesophageal reflux disease (GERD) can expose the vocal cords to stomach acid, causing irritation that may lead to cellular changes over time.
- Occupational exposure: Inhalation of wood dust, asbestos, or certain chemicals may increase risk.
It’s worth noting that vocal cord cancer is more common in men than women, typically diagnosed in people over 60. However, due to rising HPV-related cases, younger non-smokers are increasingly being diagnosed as well.
Staging Vocal Cord Cancer: What It Means
Staging describes how far the cancer has progressed and is essential for deciding the best treatment strategy. Vocal cord cancer uses the TNM system (Tumor, Node, Metastasis), which is then grouped into overall stages from 0 to IV.
The stages are defined as follows:
| Stage | Description |
| Stage 0 | Also known as carcinoma in situ. Abnormal cells are found only on the surface. |
| Stage I | Tumor is on one vocal cord with normal mobility. No spread. |
| Stage II | Tumor involves both cords or limits their movement. No lymph node involvement. |
| Stage III | Tumor has spread to nearby areas or lymph nodes in the neck. |
| Stage IV | Cancer has spread to distant tissues or organs (metastasis). |
Early-stage vocal cord cancer (Stages 0–I) has a high cure rate with localized treatment. As stages progress, treatment becomes more complex, often requiring combined modalities. That’s why early detection — especially when hoarseness is the only symptom — is so vital.
Diagnostic Process: How Vocal Cord Cancer Is Detected
Diagnosis begins when a patient reports persistent hoarseness or other throat-related symptoms. The physician typically starts with a physical exam, then moves on to more specific procedures:
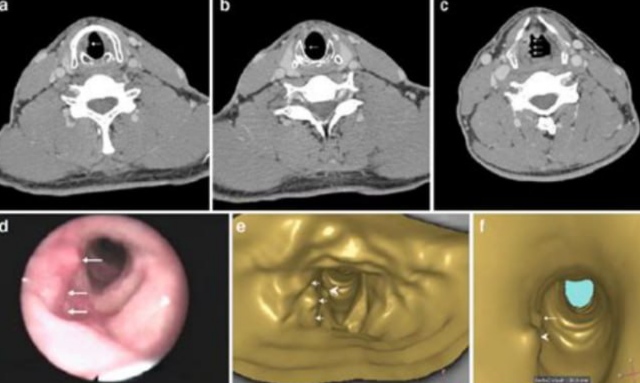
- Laryngoscopy: A flexible or rigid scope is inserted through the nose or mouth to visualize the vocal cords. This is often done in an ENT clinic under local anesthesia.
- Videostroboscopy: A high-speed camera system captures slow-motion videos of the vocal cord vibrations. It’s especially helpful for identifying small or subtle lesions.
- Biopsy: If a suspicious area is found, a tissue sample is collected—either in-office or during microlaryngoscopy under general anesthesia—and sent for histological analysis.
- Imaging Tests: CT, MRI, or PET scans help determine if the cancer has spread beyond the vocal cords to lymph nodes or distant organs
Primary Treatment Modalities for Vocal Cord Cancer
Treatment is tailored to the stage and location of the tumor, as well as the patient’s age, health status, and voice needs. The main treatment options are:
Radiation Therapy
Often the first-line treatment for early-stage vocal cord cancer. It preserves voice quality better than surgery and is non-invasive. Radiation is typically delivered five days a week over several weeks using external beam techniques.
Surgery
There are several surgical approaches depending on tumor extent:
- Cordectomy: Removal of part or all of a vocal cord.
- Partial laryngectomy: Resects larger sections but preserves speech.
- Total laryngectomy: Removes the entire voice box in advanced cases.
Advanced surgeries are increasingly performed with minimally invasive techniques like transoral laser microsurgery or robotic assistance.
Chemotherapy
Used mostly for advanced stages or recurrent cases. Common drugs include cisplatin or 5-FU. It may be combined with radiation (chemoradiation) for a more aggressive approach.
Targeted Therapy & Immunotherapy
Still under study but shows promise in select patients, particularly those with genetic markers or resistant tumors.
Side effects vary by treatment and may include fatigue, dry mouth, difficulty swallowing, or voice changes. A multidisciplinary care team—including oncologists, surgeons, and speech therapists—is essential for navigating this phase.
Life After Treatment: Recovery and Rehabilitation
Surviving vocal cord cancer is only part of the journey. Recovery focuses on restoring physical function, emotional well-being, and communication ability. Key aspects include:
- Speech and Voice Therapy: Critical for patients who have undergone surgery or radiation. Therapy begins shortly after treatment and may last for months. Techniques include breath control, articulation exercises, and digital feedback.
- Swallowing Rehabilitation: Some treatments affect swallowing muscles. Therapy helps retrain safe eating and prevent aspiration.
- Nutritional Support: A dietitian may recommend soft foods, nutrient-dense smoothies, or supplements, especially during radiation or chemotherapy.
Many survivors also benefit from peer support and psychological counseling. For broader context, it’s helpful to explore how cancer impacts emotional and social health across diagnoses.
Patients are advised to avoid smoking, limit alcohol, and follow up consistently with their care team.
Managing Voice Loss and Prosthetic Solutions
In advanced cases requiring total laryngectomy, patients lose natural voice production. However, modern prosthetics and training can help restore communication:
Common Prosthetic Options:
| Device | Description |
| Electrolarynx | A handheld vibrating device that creates mechanical voice sounds. Easy to use but sounds robotic. |
| Tracheoesophageal Puncture (TEP) | A valve placed between the windpipe and esophagus allows air to create sound. Produces a more natural voice. |
| Esophageal Speech | A technique to trap and release air from the esophagus to create vibration. Difficult to master, but no devices are needed. |
With proper support, many patients return to normal activities—even public speaking—with confidence. Speech-language pathologists are crucial in teaching these skills and guiding emotional adjustment.
Emotional and Psychological Impact of Vocal Cord Cancer
Vocal cord cancer profoundly affects self-expression and identity. For many patients, the voice is tied not only to communication but also to self-esteem, relationships, and professional roles. The emotional burden may manifest as:
- Anxiety and depression due to altered speech, uncertainty about outcomes, and social withdrawal.
- Fear of recurrence, especially in the early years post-treatment.
- Grief over loss of normal voice or physical ability.
Psychosocial support is essential. Counseling from a psychologist or oncology social worker helps process the emotional toll. Joining survivor support groups—online or in person—can foster resilience through shared experiences.
Mental wellness should be addressed as proactively as physical symptoms. Evidence shows that patients who engage with support services have better outcomes and quality of life.
Long-Term Monitoring and Follow-Up Care
After initial treatment, patients enter a critical follow-up phase aimed at detecting recurrence or secondary cancers early. A typical post-treatment care plan may include:
- Frequent laryngoscopies every 1–3 months for the first year, then at wider intervals.
- Regular imaging if there was lymph node involvement or high-stage disease.
- Blood tests or PET scans if symptoms return or spread is suspected.
Patients are urged to report changes such as hoarseness, pain, or difficulty breathing immediately. Long-term follow-up is also vital for evaluating treatment side effects like radiation fibrosis, scar tissue formation, or secondary tumors.
This stage underscores the importance of understanding the broader stages cancer progression to ensure continued vigilance beyond remission.
Common Misdiagnoses and Delays in Diagnosis
Unfortunately, vocal cord cancer can be misdiagnosed, especially in early stages when symptoms mimic benign conditions like:
- Laryngitis
- Acid reflux (LPR)
- Vocal cord nodules or cysts
Delays in diagnosis may occur if hoarseness is dismissed, especially in non-smokers or younger adults. Primary care physicians may treat symptoms with reflux medication or rest, losing valuable time.
Early referral to an ENT specialist is essential when symptoms persist beyond 2–3 weeks. Misdiagnosis is a preventable barrier—public awareness and clinical education both play roles in reducing it.
Risk Factors and Preventive Actions
Understanding risk factors empowers prevention and early detection. The most significant contributors to vocal cord cancer include:
- Tobacco use: The single biggest risk. Smoking or chewing tobacco greatly increases likelihood.
- Alcohol: Combined with tobacco, it multiplies the risk synergistically.
- HPV (Human Papillomavirus): Particularly type 16, now recognized in a subset of laryngeal cancers.
- Gastroesophageal reflux disease (GERD) and laryngopharyngeal reflux (LPR): Chronic irritation can promote cell changes over time.
Preventive strategies include:
- Quitting smoking and avoiding secondhand smoke
- Reducing alcohol intake
- Vaccination against HPV
- Managing reflux through diet and medication
- Avoiding unnecessary vocal strain
Additionally, protective measures for professional voice users—like singers, teachers, and call center workers—are critical. Routine vocal checkups and early ENT evaluation can help detect early lesions before they progress.
Role of Genetics and Family History in Vocal Cord Cancer
While vocal cord cancer is primarily linked to lifestyle and environmental exposures, there is growing interest in the role of genetics. Unlike cancers such as breast or colon cancer, a clear hereditary pattern has not been firmly established for laryngeal cancers. However, emerging studies suggest:
- Genetic polymorphisms in enzymes that process carcinogens (e.g., CYP1A1, GSTM1) may increase susceptibility.
- Family history of head and neck cancers could reflect shared environmental risks or subtle genetic predispositions.
- HPV-related cancers may follow familial clustering patterns tied to immune response genes.
Despite this, routine genetic testing is not currently part of standard care for vocal cord cancer. However, those with a strong family history of head and neck malignancies should inform their doctors and consider early screening.
Understanding genetic risk factors becomes especially relevant when comparing patterns seen in Cancer clusters across different organ systems.
Reconstructive Surgery and Voice Rehabilitation

When surgery involves partial or complete removal of vocal cord tissue, reconstructive options play a crucial role in restoring voice and breathing function. Approaches include:
- Laryngoplasty: Reshaping or repositioning remaining vocal structures.
- Voice prostheses: Devices like tracheoesophageal puncture valves enable air-powered speech.
- Electrolarynx: A handheld device that vibrates to produce robotic voice when placed on the neck.
- Esophageal speech: A technique where air is redirected into the esophagus to generate sound.
Success in voice recovery depends on surgical technique, extent of cancer, and patient participation in speech therapy. Early engagement with speech-language pathologists ensures optimal adaptation.
Rehabilitation can take months and often requires tailored exercises, breathing training, and emotional support to adjust to new vocal identity.
Understanding the Role of HPV in Vocal Cord Cancer
Human papillomavirus (HPV), particularly HPV-16, has become a notable factor in head and neck cancers—including those affecting the vocal cords. Key insights:
- HPV-positive cancers are biologically distinct from tobacco-related ones.
- They tend to occur in younger individuals with little or no smoking history.
- Prognosis is generally better, with stronger response to radiation and chemotherapy.
Diagnosis may involve testing biopsy tissue for p16 protein, a marker indicating active HPV infection. This impacts treatment planning and can influence the intensity of therapy used.
HPV vaccination for adolescents is a promising preventive tool. It not only reduces the risk of cervical and anal cancers but is increasingly recognized for protecting against oropharyngeal and laryngeal cancers.
When Vocal Cord Cancer Spreads: Metastasis and Advanced Management

Although most vocal cord cancers are diagnosed early, advanced stages can involve local invasion or distant metastasis, particularly if left untreated. The progression includes:
- Regional spread to lymph nodes in the neck
- Extension into surrounding structures such as the thyroid cartilage or esophagus
- Distant metastasis, though rare, may reach lungs or bones
Treatment in these cases becomes more aggressive, often combining surgery, chemotherapy, and radiation. Palliative care plays a greater role, focusing on comfort, breathing support, and quality of life.
Advanced cases are frequently categorized under the later end of the stages cancer scale, where survival rates drop significantly, but individualized treatment can still yield meaningful results.
15+ FAQ: Vocal Cord Cancer
1. Can vocal cord cancer be misdiagnosed as laryngitis?
Yes, especially in early stages. Both conditions can cause hoarseness, but cancer symptoms persist beyond two weeks and do not improve with standard treatments. Persistent hoarseness should be evaluated by an ENT specialist to rule out malignancy.
2. Is there a link between acid reflux and vocal cord cancer?
Chronic acid reflux (GERD) can cause ongoing irritation of the vocal cords. While not a direct cause, this inflammation may contribute to cellular changes that, over time, increase the risk of developing cancer in the area..
3. How long can someone live with untreated vocal cord cancer?
Survival without treatment varies greatly. Early-stage vocal cord cancer may grow slowly, but eventually, untreated cancer can spread locally or metastasize. Prognosis worsens significantly the longer treatment is delayed.
4. Can you feel a lump in the throat with vocal cord cancer?
Not typically. Unlike some head and neck cancers, vocal cord cancer usually presents with voice changes. A lump sensation is more likely if the tumor grows large or involves nearby tissues like the epiglottis or throat wall.
5. What’s the difference between glottic and supraglottic cancers?
Glottic cancers arise on the vocal cords themselves and are the most common. Supraglottic cancers develop above the cords and may spread more quickly due to richer lymphatic drainage, often leading to later diagnosis.
6. Is vocal cord cancer considered aggressive?
Not in early stages. Glottic cancer is often slow-growing and has a high cure rate. However, once it spreads beyond the larynx or to lymph nodes, it behaves more aggressively and becomes harder to treat.
7. Can vocal cord cancer affect breathing?
Yes, especially in advanced stages. A growing tumor can narrow the airway, leading to shortness of breath, stridor (noisy breathing), or the need for a tracheostomy in severe cases.
8. How often should a person be screened if they’re high risk?
There’s no universal screening protocol. However, smokers, heavy alcohol users, or individuals with chronic vocal symptoms should undergo yearly ENT exams and laryngoscopy if symptoms persist.
9. Can women get vocal cord cancer?
Absolutely. Although historically more common in men due to smoking patterns, vocal cord cancer does occur in women. The gender gap has been narrowing as smoking rates have changed.
10. Does radiation therapy always cause voice loss?
Not necessarily. Modern techniques aim to preserve the voice, and many patients regain near-normal function post-treatment. Temporary hoarseness is common, but long-term damage is less frequent with targeted therapy.
11. Are there dietary changes recommended for patients during treatment?
Yes. Patients may need softer foods to minimize throat discomfort. Staying hydrated and avoiding spicy, acidic, or rough-textured foods can help reduce irritation during radiation or post-surgical healing.
12. How is vocal cord cancer staged using the TNM system?
TNM stands for Tumor size (T), Node involvement (N), and Metastasis (M). A T1N0M0 cancer means a small tumor with no node spread or metastasis, while higher scores (e.g., T4N2M1) indicate more advanced disease.
13. Can secondhand smoke increase the risk of vocal cord cancer?
Yes. Prolonged exposure to secondhand smoke carries a similar carcinogenic risk as direct smoking, particularly in poorly ventilated environments. It contributes to chronic irritation and DNA damage in throat tissues.
14. What role do dental professionals play in early detection?
Dentists and hygienists trained to recognize oral and throat abnormalities may spot early signs during routine exams, especially in patients who smoke or report chronic hoarseness.
15. Are certain professions at higher risk?
Yes. Those with chronic voice strain—such as singers, teachers, public speakers—and those exposed to airborne irritants (e.g., construction workers, welders) may be at slightly elevated risk, especially when combined with smoking or alcohol use.












