VA Disability Rating for Cancer in Remission – Full Guide
- Foreword
- Part 1: Introduction
- Part 2: Understanding VA Disability Ratings
- Part 3: VA Disability Rating for Active Cancer
- Part 4: Transitioning to Remission — What Happens Next?
- Part 5: Residual Effects and Secondary Conditions
- Part 6: The Reexamination Process
- Part 7: Total Disability Based on Individual Unemployability (TDIU)
- 12. Frequently Asked Questions (FAQ)
Foreword
If you’re reading this, there’s a good chance you—or someone close to you—has already walked a hard road: a cancer diagnosis, the long and often grueling process of treatment, and now, the delicate phase known as remission. First, allow us to say this plainly: what you’ve endured is extraordinary. And if you’re a veteran, you’ve likely carried the weight of that experience on top of everything your service demanded of you.
You’re here not to revisit the cancer, but to understand what happens next—specifically, how the VA handles disability ratings when cancer is no longer “active” but the impact, clearly, doesn’t just vanish.
This isn’t just about benefits—it’s about recognition. Recognition that remission doesn’t always mean restoration. That just because your oncologist says “clear,” it doesn’t mean you’re done reckoning with what cancer took from you. And perhaps most importantly, it’s about knowing that the VA system can work for you—if you know how to work with it.
This article is designed as a final stop, not a first glance. It’s not here to sell you shortcuts or dazzle you with buzzwords. It’s here to clarify every part of the VA disability rating process specific to cancer in remission—because this is one of those topics where half-answers and outdated forum posts only lead to confusion.
By the time you finish reading, you’ll understand:
- What happens to your VA rating after cancer treatment ends.
- How residual effects and secondary conditions factor in.
- What the reevaluation process actually looks like.
- And how to position yourself for the rating you’ve rightfully earned.
You’ll also find clarity on tricky areas like protected ratings, TDIU, and appeals—and a real-world sense of how to navigate the bureaucracy with strategy, not frustration.
So let’s start from the beginning. Not the diagnosis—but the system you now have to navigate. You’ve already fought one war. Let’s talk about how to win this one, too.
Introduction
Let’s address the big question up front: If my cancer is in remission, does that mean I lose my VA disability benefits?
The short answer? Not necessarily. But the long answer is the one that matters—because it hinges on several factors, from how the VA interprets your medical records to how well your residual symptoms are documented, and even how long ago your initial cancer rating was awarded.
Here’s the reality many veterans don’t hear soon enough: The end of active cancer treatment is not the end of your eligibility for compensation. It’s just the beginning of a different chapter in how the VA evaluates your condition.
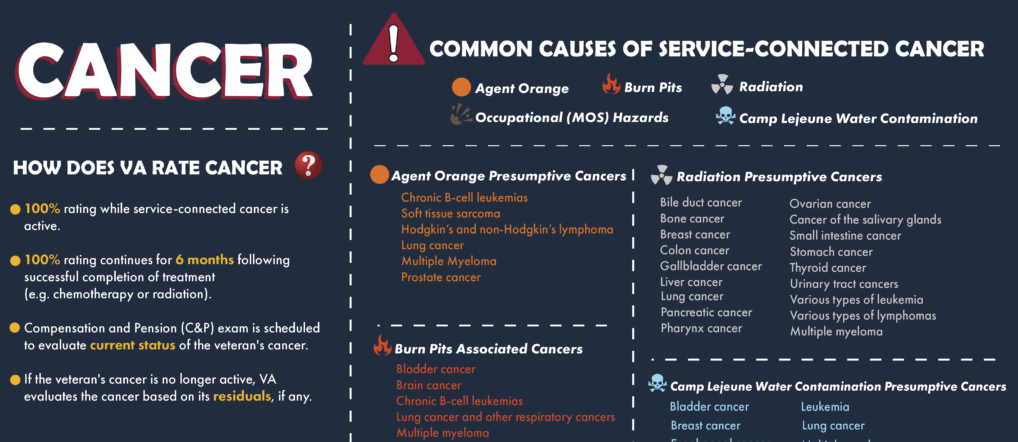
You see, the VA does grant an automatic 100% disability rating for most service-connected cancers while they are active—that is, while you’re undergoing surgery, chemotherapy, radiation, or other intensive treatments. This rating typically stays in place for at least six months after your last treatment. But after that window, the VA initiates a process called reevaluation—and this is where the waters get murky.
You might be thinking, “If my scans are clean and my treatment’s done, how do I justify a continued rating?” Fair question. The answer lies in something called residuals—the lingering physical and mental effects that persist even after the cancer is gone. Think chronic fatigue, nerve damage from chemo, bowel dysfunction, sexual health issues, lymphedema, anxiety, PTSD, or any of the countless ways cancer changes the body long after remission is declared.
Now here’s the catch: the VA doesn’t assume residuals. They have to be proven. That’s why understanding how to document your symptoms, work with your doctors, and frame your claims can make the difference between keeping a meaningful rating—or watching it get slashed unfairly.
And here’s something else: not all cancers are treated equally. Some are considered presumptively service-connected, meaning the VA accepts without argument that your military service caused the illness (think Agent Orange and certain blood cancers, or Gulf War toxic exposure and brain tumors). Others require a lot more medical evidence to link your diagnosis to your service.
This brings us to a deeper, more uncomfortable truth: many veterans fall through the cracks during remission. Why? Because once the “active cancer” label drops off, the burden of proof shifts back onto you. The system becomes less automatic, more bureaucratic. And if you’re not prepared, you could unknowingly accept a lower rating than you’re entitled to—leaving benefits, and frankly justice, on the table.
We wrote this guide because too many veterans are given surface-level answers. “It depends” isn’t enough. You deserve a roadmap that covers every angle: legal, medical, procedural. Not a brochure. Not a soundbite. A complete understanding.
In the sections ahead, we’ll break down every piece of this puzzle—from how ratings work, to what happens at reexaminations, to strategies for navigating appeals and maximizing your compensation post-remission. Because when it comes to cancer and VA ratings, remission isn’t the end. It’s the start of something new—and we’ll make sure you’re ready for it.
Understanding VA Disability Ratings
The VA disability rating system can be confusing—there’s no sugarcoating it. Even veterans who have been through the process before often find themselves scratching their heads when faced with the percentages, schedules, and combined ratings. But understanding how the VA assigns disability ratings isn’t just academic; it’s essential if you want to get the benefits you deserve, especially when it comes to something as complex as cancer in remission.
| Disability #1 | Disability #2 | Combined Rating (VA Math) | Explanation |
|---|---|---|---|
| 50% | 50% | 75% → Rounded to 80% | 50% of remaining 50% is 25%; 50 + 25 = 75% |
| 70% | 30% | 79% → Rounded to 80% | 30% of remaining 30% is 9%; 70 + 9 = 79% |
| 60% | 20% | 68% → Rounded to 70% | 20% of remaining 40% is 8%; 60 + 8 = 68% |
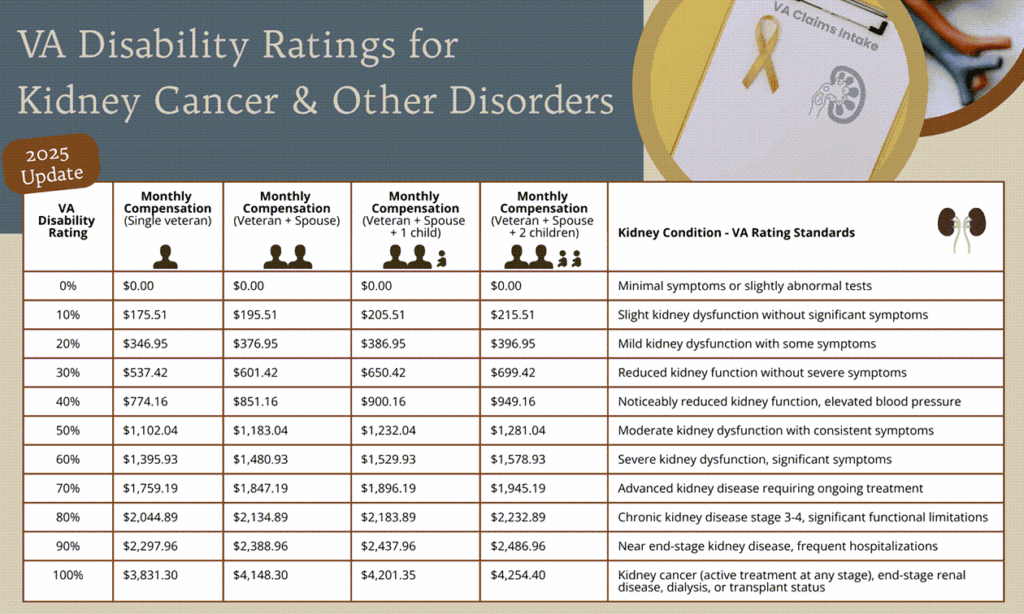
At its core, the VA disability rating is a percentage that reflects how much your service-connected condition impairs your ability to live and work. Ratings range from 0% to 100%, increasing in increments of 10%. A 0% rating means the VA acknowledges your condition is related to service but it’s not currently disabling enough to warrant monthly compensation. A 100% rating means you’re considered totally disabled because of your service-connected condition.
When it comes to cancer, the VA grants an automatic 100% rating while the disease is active—that is, during treatment. This is a recognition of how profoundly cancer affects your life in this phase, regardless of your ability to work. The VA does not require proof of unemployability or daily impairment during active cancer treatment; the diagnosis alone warrants full compensation.
But after treatment ends and remission begins, the VA’s approach changes. They no longer rate the cancer itself but rather the residual effects left behind by cancer and its treatment. This means that instead of a single, overarching cancer rating, your disability rating may consist of multiple separate ratings for different conditions—like neuropathy, fatigue, or depression—that stem from your cancer experience.
And here’s an important point that trips up many veterans: VA ratings don’t add up like simple math. For example, if you have two disabilities each rated at 50%, you might expect a combined rating of 100%. But the VA uses a combined ratings table that reflects the whole person concept—your body can’t be 150% disabled. Instead, they combine these percentages in a way that usually results in a combined rating less than the simple sum—in this example, about 75% or 80%.
Why does this matter? Because your total combined rating determines your monthly compensation, access to benefits, and eligibility for programs like Total Disability based on Individual Unemployability (TDIU). Understanding this formula helps you see how your different residuals affect your overall benefits.
Another key piece is how the VA assigns ratings for each condition. They use the Schedule for Rating Disabilities (VASRD), which provides detailed criteria for each diagnosis. For instance, peripheral neuropathy might be rated from 10% for mild symptoms to 80% for severe involvement of all limbs. Mental health conditions like depression have their own rating scale based on how much they interfere with occupational and social functioning.
A crucial takeaway here is that the VA relies heavily on medical evidence and documentation. They don’t guess or make assumptions. If your records say “mild symptoms,” that’s what they rate. If you underreport symptoms or your doctors don’t document them carefully, you risk a lower rating than your true level of disability.
Finally, it’s important to recognize that VA disability ratings are dynamic. They can increase, decrease, or stay the same over time, depending on changes in your condition and medical evidence. That’s why understanding this system fully arms you to advocate effectively and maintain the compensation you deserve.
For veterans navigating remission and benefits, it helps to understand how the 60% rating for prostate cancer is applied in practice.
VA Disability Rating for Active Cancer
If there’s one part of the VA disability process that’s surprisingly straightforward, it’s this: if your cancer is active and service-connected, the VA will assign you a 100% disability rating. No need to fight for it. No need to prove how badly your symptoms affect your ability to work or function. The diagnosis and documentation of active, service-connected cancer are enough. It’s one of the few areas where the VA’s rules offer immediate, unambiguous support.
But—and there’s always a “but” with VA benefits—this simplicity is temporary. The automatic 100% rating applies only while the cancer is considered active, or while you are undergoing treatment. That treatment might include surgery, radiation therapy, chemotherapy, immunotherapy, hormone therapy, or other forms of ongoing medical intervention. Once treatment ends and the cancer is in remission, the VA doesn’t just keep the 100% rating going indefinitely.
This is where things shift, and where many veterans feel blindsided.
The VA allows the 100% rating to continue for six months following the cessation of treatment—this is sometimes called the “convalescent period.” After those six months are up, the VA initiates a reevaluation process to determine whether your condition still warrants a 100% rating. In practice, this means they stop looking at your cancer as the primary disability and start examining the residual effects of your condition and treatment.
You might ask: “What counts as the ‘end’ of treatment?” That’s not always easy to pin down. In many cases, it’s the final chemo session or radiation treatment. But what if you’re receiving long-term hormonal therapy? What if your oncologist is still actively monitoring you every few months? The VA’s rules here are not always crystal clear, and interpretations can vary. Generally, if the treatment is considered curative or intensive, the clock starts ticking after it ends. Maintenance or surveillance therapy may not reset that six-month buffer—but sometimes you can argue that it should, depending on how aggressive or ongoing the treatment is.
The next question is often: “What happens if my cancer comes back?” In that case, you can—and absolutely should—file a new claim or request an increased rating. The VA can reinstate the 100% disability rating for a cancer recurrence, but they won’t do it automatically. You must provide updated medical documentation showing that the cancer has returned and that treatment has resumed. Timeliness matters here. The sooner you submit this information, the faster your benefits can be adjusted.
It’s also worth noting that for some types of cancer—especially those considered incurable or likely to recur—the VA may decide that your 100% rating should be permanent and total. That means no more reevaluations, no risk of reduction. This isn’t common, but it happens in cases of aggressive or metastatic cancers where long-term stability is unlikely.
However, if your cancer goes into remission and the VA sees no significant lasting effects, your rating could drop dramatically—even to 0%. That can be a devastating blow after months or years of treatment. But here’s the thing: a reduction doesn’t mean the end of the road. If you’re dealing with fatigue, pain, mobility issues, nerve damage, or mental health struggles, those residuals can and should be rated separately. The key is making sure those symptoms are well documented, both in your medical records and during your Compensation & Pension (C&P) exam.
The takeaway here is simple: the 100% rating during active cancer treatment is real and guaranteed, but it doesn’t last forever. Knowing this ahead of time gives you the power to prepare for what comes next—so that you’re not left with a drastically reduced rating and no idea why. You’ve fought hard to get here. Don’t let your benefits vanish just because the cancer’s no longer visible.
Transitioning to Remission — What Happens Next?
Let’s say the scans are clean. Your oncologist uses the word remission. Maybe cautiously, maybe with a smile, maybe after months (or years) of uncertainty. It’s a word that feels like a finish line—until you start wondering what it means for your benefits.
“Does remission mean I’m cured in the eyes of the VA?”
Not exactly.
“Does remission mean I’m no longer disabled?”
Not necessarily.
And here’s the part that surprises—and frustrates—many veterans: remission doesn’t eliminate your right to compensation. But it does change the battlefield. You’re no longer being rated based on the cancer itself. You’re now rated based on the aftermath—the symptoms, side effects, and functional losses that linger long after treatment ends.
This phase is where things often get fuzzy, bureaucratic, and emotionally exhausting. The VA doesn’t hand you a map, but we will.
The 6-Month Countdown
When your active cancer treatment ends—meaning the last round of chemo, the final zap of radiation, or the recovery from surgical removal—the VA typically continues your 100% rating for six months. That’s six months of what they consider a “convalescent period.”
During that time, many veterans assume their benefits are locked in. But behind the scenes, the gears are already turning. The VA is preparing for a reevaluation, which will determine what your rating should be now—in this new, post-treatment chapter.
So what does the VA look for when that reevaluation begins?
From Disease to Damage: The Shift in Focus
Once remission is on the table, the VA’s attention shifts from the cancer diagnosis itself to the residuals: what did the cancer—and more importantly, its treatment—leave behind?
Residuals may be:
- Physical: fatigue, joint stiffness, bowel issues, nerve damage, erectile dysfunction, infertility, lymphedema, pain, scarring.
- Neurological: cognitive fog, chemo brain, balance problems, hearing loss (if related to head/neck radiation).
- Mental/emotional: anxiety, depression, PTSD-like symptoms, fear of recurrence, sleep disorders.
- Functional: trouble maintaining employment, difficulty with daily tasks, lack of energy or stamina, chronic infections or immunosuppression.
Here’s what the VA will not do: they will not assume these residuals exist. They won’t extrapolate. They won’t read between the lines.
They’ll rate only what’s documented, what’s measurable, and what’s tied directly to your service-connected condition.
Reevaluation Isn’t a Form — It’s a Test
Sometime after the six-month window, you’ll receive a VA C&P exam request—either through the mail, online, or via a call from a third-party contractor. Many veterans assume this is a rubber-stamp appointment. It’s not.
The exam is effectively the VA’s way of asking: Is this veteran still experiencing impairments? And if so, how severe are they?
Your rating could be:
- Maintained at 100% if your residuals are catastrophic or the cancer is still deemed active in some form.
- Reduced to a lower rating based on identified complications.
- Dropped to 0% (yes, zero) if the VA determines that your remission is “complete” and your residuals are “noncompensable.”
This last scenario—going from 100% to 0%—can feel like a gut punch, and it’s unfortunately not uncommon. But here’s what makes all the difference: preparation.
How to Prepare for Your Reevaluation Like a Pro
Let’s be blunt: if you show up to a C&P exam and say, “I’m doing okay,” and that’s all you say—you’re giving them the green light to minimize your rating.
You need to speak VA language, and that means:
- Get documentation in order.
- Recent oncologist notes.
- Reports from your primary care doctor.
- Symptom logs—daily fatigue levels, pain episodes, medication use, etc.
- If applicable, therapy notes or mental health assessments.
- Write a personal statement.
Explain in plain but specific terms how the cancer and treatment continue to impact your life. Use details. “Fatigue” is too vague. “I need to nap after 30 minutes of housework” is actionable. “I avoid social settings due to bowel urgency” is informative. - Don’t downplay your symptoms.
Veterans are famously stoic. You’ve been trained to understate pain and power through it. But the VA system isn’t grading toughness—it’s grading limitation. Be honest. Be clear. Be detailed. - Request support from a VSO rep.
Organizations like DAV, VFW, and American Legion can help you prepare your case. Some may even help attend your exam or file a supplemental claim if your rating gets reduced.
“What if my residuals develop later?”
Great question—and here’s some good news: you can always file for an increase. The VA doesn’t expect all residuals to appear within six months. Some issues—like lymphedema, delayed neuropathy, or psychological effects—may show up much later.
You can file a new claim at any time for a condition that’s secondary to your service-connected cancer. And the VA is obligated to evaluate it accordingly, whether your original cancer claim is still open or not.
“What if my rating gets reduced unfairly?”
Don’t panic. You have options.
You can:
- Request a higher-level review, asking a more senior VA reviewer to reconsider the decision.
- Submit a supplemental claim with new medical evidence.
- File a formal appeal with the Board of Veterans’ Appeals.
All of these paths are valid. And if you feel overwhelmed? That’s what VSOs and accredited claims agents are for. You do not have to go it alone.
There’s also a strong case for comparing how other chronic cancers are treated under the system. For example, Endometrial cancer and re-irradiation often raise similar follow-up questions.
Residual Effects and Secondary Conditions
By the time your cancer enters remission, the visible war may be over—but the internal battle often isn’t. The VA knows this, at least in principle. That’s why their rating system doesn’t stop at “remission.” Instead, it’s supposed to pivot: away from the disease itself and toward the damage left behind. That’s where residual effects and secondary conditions come into play—and they’re often what determine your compensation moving forward.
| Residual Condition | Possible Rating Range | Common Symptoms/Impacts |
|---|---|---|
| Peripheral Neuropathy | 10% – 80% | Numbness, tingling, burning pain in limbs |
| Chronic Fatigue | 10% – 60% | Daily exhaustion, limited endurance |
| Depression/Anxiety | 0% – 100% | Sleep issues, emotional volatility, isolation |
| Lymphedema | 10% – 40% | Swelling, heaviness, reduced mobility |
| Bowel/Bladder Dysfunction | 10% – 60%+ | Urgency, incontinence, lifestyle disruption |
| Sexual Dysfunction | 0% – Special Monthly Comp. | Erectile dysfunction, infertility, intimacy strain |
Let’s start with residual effects. These are the physical and psychological consequences of both the cancer and the treatments used to fight it. They’re not minor side notes; they can be deeply disruptive, even disabling. We’re talking about symptoms like peripheral neuropathy (nerve damage from chemotherapy), lymphedema (swelling from lymph node removal or radiation), chronic fatigue, organ dysfunction, and persistent pain in surgical sites or irradiated tissues. They’re not always dramatic, but they are persistent—and they affect your daily functioning in ways that the VA should compensate for, provided the symptoms are adequately documented.
It’s not just physical, either. Cancer survivors often deal with cognitive challenges—problems concentrating, slowed thinking, memory fog—commonly referred to as “chemo brain.” Others may find that the trauma of their diagnosis and treatment has triggered depression, anxiety, or PTSD-like symptoms. These mental health effects are just as real and compensable as physical ones, but they require proper medical documentation and, ideally, a professional nexus statement linking them to your cancer experience.
Then there are secondary conditions—those that aren’t direct effects of the cancer, but developed because of it or its treatment. These might include:
- Sexual dysfunction resulting from prostate cancer treatment.
- Hormonal imbalances after thyroid or testicular cancer.
- Gastrointestinal problems from abdominal surgeries or radiation.
- Osteoporosis due to long-term corticosteroid use or hormonal therapy.
- Mental health conditions brought on or exacerbated by the trauma and disruption of cancer.
To be clear, these conditions don’t have to be diagnosed during treatment. They might emerge months or even years later. The important part is showing that they’re at least as likely as not to be linked to your service-connected cancer. That’s where a solid medical nexus opinion comes in—a letter or evaluation from a treating provider or VA examiner explicitly stating the connection. Without this link, your claim can be denied even if your symptoms are severe and well-documented.
So how does the VA rate all of this?
Each residual or secondary condition is evaluated under its own section of the VA Schedule for Rating Disabilities (VASRD). Fatigue might be rated under chronic fatigue syndrome. Neuropathy gets its own code, as does lymphedema. Depression and anxiety fall under the mental health ratings schedule, which can range from 0% to 100% depending on how much they interfere with your occupational and social functioning.
And here’s the kicker: each of these ratings can be stacked—but not added. As we covered earlier, the VA uses a combined ratings formula that reflects the idea that no one can be more than 100% disabled. So two 50% ratings don’t make 100%; they make 75%, which rounds up to 80%. That’s why documenting every condition and making sure nothing gets overlooked is critical—because it takes multiple well-rated residuals to approach a full 100%.
Now, let’s talk about documentation. This can’t be overstated: if your doctor doesn’t note your symptoms in the record, the VA won’t consider them. You may be dealing with intense fatigue or limited mobility, but if your medical records say “veteran doing well” or “no complaints,” the VA is going to assume everything’s fine. You need detailed notes that describe not just the presence of symptoms, but their severity, frequency, and impact on your daily life.
If your current providers aren’t familiar with the VA’s expectations, it’s worth speaking up. Explain that your disability rating depends on how thoroughly your symptoms are documented. If possible, get second opinions or see specialists who can provide targeted evaluations—neurologists for nerve damage, psychologists for mental health, physical therapists for mobility issues, and so on.
Residual effects and secondary conditions aren’t always immediately visible—not to your friends, not to your providers, and certainly not to a C&P examiner on a tight schedule. But they’re real. And the law says that if your service-connected cancer led to real, documented impairments—even after remission—you are entitled to compensation for them.
So if you’re feeling worse than your current rating reflects, or if new symptoms have cropped up that your initial claim didn’t cover, this is the moment to act. The VA system may not be proactive, but with the right documentation, guidance, and persistence, it will respond.
The Reexamination Process
For many veterans, the most unsettling part of surviving cancer isn’t just the health aftermath—it’s the sudden shift in tone from the VA. One day, you’re being told your cancer entitles you to a 100% disability rating, no questions asked. The next, you receive a letter scheduling a “reexamination,” as if the system wants to quietly take back what it once gave without a fight. If you’ve reached this point, know this: you’re not alone, and you’re not powerless. But you do need to understand exactly what’s happening—and what the VA is really looking for.
This reexamination, often triggered about six months after the conclusion of your last cancer treatment, isn’t a ceremonial box-check. It’s the VA’s way of saying, “We’re reassessing whether you’re still this disabled.” But here’s the catch—they’re no longer evaluating the cancer itself. The focus has now turned to what the cancer and its treatment left behind. That includes residuals like chronic pain, nerve damage, persistent fatigue, mobility issues, and mental health conditions that may have developed during or after your battle with the disease. These effects may be invisible to others, but if they impact your function, they’re real—and the VA needs to recognize that.
Veterans often head into this process unprepared, believing their prior 100% rating or medical history will speak for itself. It won’t. The examiner you see may not be a VA doctor at all, but a contractor hired to perform a quick evaluation based on preset criteria. Some spend less than twenty minutes with you. Some barely skim your medical file. This means that how you communicate your current condition matters just as much as what’s on paper.
If your fatigue now limits how far you can walk, if your hands still go numb from chemotherapy-induced neuropathy, if your anxiety spikes every time you think about follow-up scans—that needs to be said. And not just casually. You must give shape to your symptoms. Tell them how your daily life is impacted: the missed workdays, the social withdrawal, the inability to focus, the moments when pain or dysfunction changes your plans. This isn’t exaggeration—it’s evidence. It’s what the system demands, even if the tone is clinical.
Too many veterans minimize what they’re going through. Maybe it’s habit. Maybe it’s pride. But the VA doesn’t interpret humility—it interprets documentation. If you tell the examiner you’re “doing okay,” they may assume your impairments are minimal. The burden is on you to be honest, specific, and unflinching.
And what happens after the exam? You wait. The VA will analyze the examiner’s report and issue a decision. Sometimes your rating is maintained, sometimes reduced, sometimes reevaluated and split across multiple new conditions with individual ratings. And yes, sometimes they get it wrong—badly. If your rating is reduced unfairly or if important symptoms are dismissed, you have the right to push back. You can submit new evidence, request a higher-level review, or initiate a formal appeal. The VA must give you advance notice before any reduction takes effect, which gives you time to respond strategically.
There are also longer-term considerations. In some cases, veterans can avoid future reexaminations if their conditions are deemed “permanent and total.” This often applies when residuals are clearly irreversible or progressive. If your oncologist or specialist believes that your impairments will not improve, you may be able to have your rating reclassified as permanent—locking it in and relieving you of the need for further exams.
And if you’re newly in remission, articles like Terminal Cancer Couloir may feel emotionally distant now, but they still frame the long view — worth reflecting on.
The reexamination phase can feel cold and transactional, especially after something as emotionally and physically traumatic as cancer. But it’s also a critical opportunity. It’s your chance to define, clearly and credibly, what remission has cost you. This is not about dramatizing your experience—it’s about owning it. Bringing the invisible into the light. And ensuring that the VA doesn’t overlook what you’re still carrying, simply because the worst is over on paper.
Total Disability Based on Individual Unemployability (TDIU)
There’s a unique kind of frustration that comes with surviving cancer only to discover that you now exist in a grey zone—not sick enough to qualify for a full VA rating, but not well enough to hold down a regular job. Maybe your neuropathy makes fine motor work impossible. Maybe your fatigue forces you to nap midday just to function. Maybe your anxiety, once managed, now flares unpredictably. You might have a 70% combined rating. Or 80%. Or even 60%. But you know, in your bones, that you can’t work the way you used to. And that’s where Total Disability based on Individual Unemployability, or TDIU, becomes incredibly important.
TDIU is one of the VA’s more humane policies—on paper, at least. It recognizes that a veteran may not meet the strict formula for a 100% disability rating, but still be effectively unable to work because of service-connected conditions. For cancer survivors, this often reflects reality. The rating system carves up your condition into parts—this nerve damage is worth 30%, that fatigue is worth 20%, your depression maybe 10%—and somehow those fragments don’t quite add up to the whole truth: that you’re no longer capable of maintaining stable, gainful employment.
The term “substantially gainful employment” is the legal heart of TDIU. What the VA means is: work that isn’t marginal, that pays above the poverty line, and that a reasonable person could maintain regularly. If your service-connected conditions prevent you from doing that kind of work, you may qualify for TDIU—even if your combined rating doesn’t hit 100%.
But of course, you still have to make the case.
And this is where many veterans stumble—not for lack of legitimacy, but for lack of clarity. The VA isn’t interested in whether you’re working your dream job or whether your condition is generally inconvenient. They want to see that your symptoms directly interfere with your ability to hold a steady job. If your fatigue causes you to call out sick every week, or your nerve pain makes it impossible to type, or your cognitive issues cause you to make mistakes you never used to make—that’s relevant. The question isn’t whether you’re technically employed now. The question is whether your condition allows you to engage in meaningful, sustainable work on a consistent basis.
It’s not just about your symptoms—it’s about how they translate into functional limitations. That distinction matters.
And no, the VA won’t intuit this. You’ll have to put it in writing. Often, that means submitting VA Form 21-8940, which sounds like just another form, but it’s actually your opportunity to tell the story the ratings system can’t fully capture. Your medical records are critical here, but so is your narrative. The more your personal account aligns with your documented impairments, the stronger your case.
If you’re denied, it’s not the end. Veterans are denied TDIU all the time—not because they’re undeserving, but because the picture painted for the VA lacked definition. Sometimes there’s not enough evidence. Sometimes it’s presented in a way that fails to tie everything together. Often, it’s just the system working the way bureaucracies do: inconsistently and imperfectly. But appeals are possible, and many veterans win them—especially with legal help or the support of a VSO who understands how to frame the claim properly.
One of the most persistent myths about TDIU is that it’s a kind of backdoor to 100%—a workaround. But that’s a misconception. TDIU is not a trick; it’s a legitimate recognition that numbers alone don’t always reflect the lived reality of disability. If your cancer and its aftermath have robbed you of your ability to earn a living, TDIU may be your most accurate rating—even if the percentages say otherwise.
It’s also worth noting that being granted TDIU can come with full 100% benefits—housing allowances, access to additional care, education benefits for dependents, and more. It’s a difference that can stabilize not just your income, but your family’s financial health as well.
Still, some veterans hesitate to pursue TDIU. They worry it labels them as unemployable, permanently sidelined. But here’s the truth: pursuing TDIU isn’t surrender. It’s recognition. It’s claiming space in a system that often wants to shrink your story down to digits and codes. If you’ve fought cancer, survived treatment, and live every day with the consequences—working or not—you’ve earned the right to have that reality reflected accurately in your benefits.
Frequently Asked Questions (FAQ)
1. How long does the 100% disability rating last after cancer treatment ends?
Typically, the VA grants a 100% disability rating for six months after your last cancer treatment. This period is considered a convalescent phase before reevaluation. However, this can vary slightly depending on your specific circumstances and the type of cancer.
2. Can I receive a disability rating if my cancer is in remission?
Absolutely. Even if your cancer is in remission, you may qualify for ratings based on residual effects from the cancer itself or its treatment, such as neuropathy, fatigue, organ dysfunction, or mental health conditions.
3. What kinds of residual effects does the VA recognize?
The VA recognizes a wide range of residuals, including but not limited to: chronic pain, nerve damage, lymphedema, cognitive difficulties (often called “chemo brain”), sexual dysfunction, depression, anxiety, and bowel or bladder problems.
4. How does the VA determine if my cancer is service-connected?
Service connection is established by showing a nexus—a medical link—between your cancer diagnosis and your military service. This can be based on exposure to certain hazards (e.g., Agent Orange, burn pits), documented in-service injuries, or presumptive conditions recognized by the VA.
5. What is Total Disability based on Individual Unemployability (TDIU), and how can it help me?
TDIU allows veterans who can’t work due to service-connected disabilities to receive compensation at the 100% level, even if their combined rating is less than 100%. It’s especially relevant for cancer survivors whose residual conditions impair their ability to maintain gainful employment.
6. Are there protections against my disability rating being reduced after remission?
Yes. If you’ve held a 100% rating for five, ten, or twenty years, the VA has protected rating rules that make it harder to reduce your benefits. These protections provide some security that your rating won’t be unfairly lowered.
Closing Thoughts
If you’ve made it this far, you’ve already demonstrated something many veterans quietly carry but rarely get credit for: persistence. You’ve walked through a diagnosis that reshaped your life. You’ve endured treatments, fear, and fatigue. And now, you’re navigating a system that often feels indifferent to the very things it was designed to support.
The VA disability process—especially for cancer survivors in remission—isn’t just about policy or paperwork. It’s about language. It’s about knowing how to take what’s lived and felt and turn it into something legible to a bureaucracy. That’s no small task. It requires you to hold two truths at once: that you’re lucky to be in remission, and that you’re still grappling with the price of survival.
This guide wasn’t meant to simplify your experience into formulas and flowcharts. It was meant to equip you—with language, with strategy, with clarity. Because understanding how the VA thinks, how ratings are determined, and how to make your case effectively can change not only the outcome of your claim but your relationship to the process itself.
So, what now?
Now you advocate—with purpose. Now you document with intention. Now you resist the urge to downplay your symptoms or talk yourself out of what you’ve earned. Because compensation isn’t charity. It’s not about what you deserve in theory—it’s about what the law, when properly applied, already entitles you to. Your job isn’t to beg for benefits; it’s to hold the system to its own standard.
And remember, you’re not alone. Whether it’s a Veteran Service Organization helping you submit your claim, a fellow survivor reminding you that invisible pain still counts, or a medical provider willing to put your truth on paper—support is out there. Use it. Rely on it. Build with it.
The VA rating system is never going to be perfect. But it can work in your favor—if you understand its logic and match it with your own voice, your own evidence, and your own resolve.
You’ve survived something most people can’t imagine. Now it’s time to make sure that survival is recognized in full—not as a footnote, not as an asterisk, but as the ongoing, daily reality that it is.
You’ve carried the weight. Let the system carry its share, too.










