Unintentional Weight Loss in Pancreatic Cancer
Unintentional Weight Loss in Pancreatic Cancer: What It Means and How to Respond
- Why Does Unintentional Weight Loss Happen in Pancreatic Cancer?
- How the Tumor Affects the Body’s Metabolism and Nutrient Absorption
- How Common Is Weight Loss in Patients with Pancreatic Cancer?
- Clinical Observations by Stage and Tumor Location
- What Causes Weight Loss in Pancreatic Cancer: A Closer Look
- Danger Signs: When Weight Loss Requires Urgent Medical Attention
- How Weight Loss Is Diagnosed and Measured in Cancer Patients
- Treating and Managing Weight Loss in Pancreatic Cancer
- Can Weight Loss Be Prevented in Pancreatic Cancer Patients?
- Will the Weight Return After Treatment?
- What Oncology Experts Say About Weight Loss in Pancreatic Cancer
- 15+ Frequently Asked Questions (FAQ)
Why Does Unintentional Weight Loss Happen in Pancreatic Cancer?

Unintentional weight loss is one of the hallmark symptoms of cancer, and in the case of pancreatic cancer, it’s especially common and often severe. Unlike weight loss due to diet or exercise, this type occurs without effort and can significantly impact physical strength, immunity, and prognosis.
In many patients, the loss of weight is the first noticeable sign that something is wrong. It often appears before a formal diagnosis is made, contributing to the late detection that characterizes pancreatic cancer. The weight loss may be rapid, exceeding 10% of body weight within a few weeks or months, and is typically accompanied by fatigue, appetite changes, and digestive discomfort.
This symptom is not just about appearance—it reflects serious metabolic and systemic disruptions caused by the cancer itself and its effects on nearby organs. It can be a warning sign of disease progression or complication and should always be addressed urgently.
How the Tumor Affects the Body’s Metabolism and Nutrient Absorption
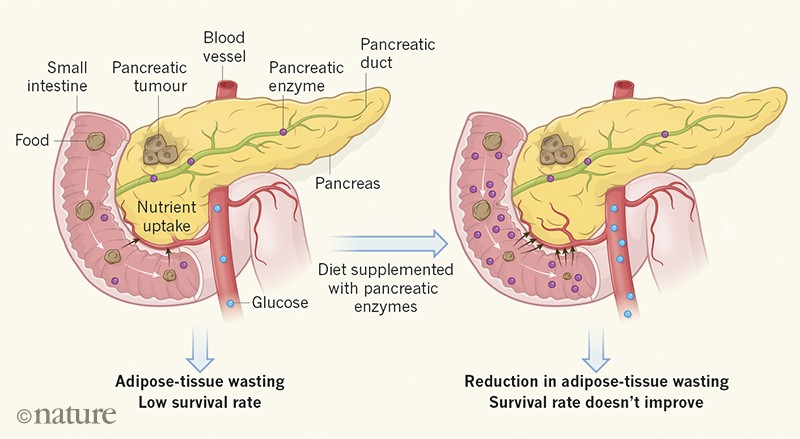
Pancreatic tumors interfere directly with the digestive process, which is central to maintaining a healthy weight. The pancreas produces enzymes necessary for digesting fats, proteins, and carbohydrates. When a tumor impairs this function, it leads to malabsorption and nutrient deficiency—even when the patient eats regularly.
In addition, cancer cells consume enormous amounts of energy to grow and spread. This forces the body to break down muscle and fat reserves, leading to cachexia—a severe form of cancer-associated weight loss marked by muscle wasting and inflammation.
Furthermore, pancreatic tumors often cause systemic inflammation, elevating levels of cytokines like IL-6 and TNF-alpha. These molecules promote catabolism (breakdown of tissue), reduce appetite, and impair the brain’s ability to regulate hunger and energy balance.
Some treatments for pancreatic cancer, including chemotherapy or advanced local ablation methods like NanoKnife Pancreatic Cancer therapy, can exacerbate nausea, vomiting, or digestive upset, further contributing to caloric deficit and tissue loss.
How Common Is Weight Loss in Patients with Pancreatic Cancer?
Unintentional weight loss is extremely common in pancreatic cancer, reported in up to 85–90% of patients at the time of diagnosis. It is often more pronounced in advanced stages, though even early-stage patients can experience significant changes due to exocrine insufficiency or early systemic effects.
Clinical studies have shown that weight loss exceeding 5% of total body mass in less than six months is associated with worse overall survival in pancreatic cancer. In many cases, this symptom appears before the cancer is identified, which is why it is often a red flag in diagnostic evaluations.
In later stages, cachexia—a profound and often irreversible syndrome of weight and muscle loss—affects approximately 50–70% of patients. This condition not only limits physical resilience but also reduces the body’s ability to tolerate cancer therapies.
Weight loss is also more common in tumors located in the head of the pancreas, which often obstruct the bile duct and digestive enzymes earlier than tumors in other locations.
Clinical Observations by Stage and Tumor Location
The extent and severity of weight loss in pancreatic cancer vary significantly depending on tumor location and cancer stage.
In localized disease (stage I or II), patients may begin to lose weight due to reduced pancreatic enzyme output and subtle metabolic disruptions. This can occur even before symptoms like jaundice or abdominal pain develop.
By stage III, where the tumor may involve major blood vessels or regional lymph nodes, metabolic demand increases dramatically. Inflammatory responses rise, appetite declines further, and nutrient absorption may be significantly impaired.
In metastatic or stage IV cases, weight loss is often profound. Cachexia becomes more pronounced, muscle mass declines rapidly, and patients may struggle to maintain even minimal nutritional intake. This not only affects quality of life but also reduces eligibility for certain treatments, including surgery or aggressive chemotherapy.
Tumors in the pancreatic head tend to present with earlier weight loss due to ductal obstruction, while tail or body tumors might progress further before symptoms are noted—often resulting in more dramatic weight loss once detected.
What Causes Weight Loss in Pancreatic Cancer: A Closer Look
Unintentional weight loss in pancreatic cancer is driven by a combination of local and systemic mechanisms that evolve as the disease progresses. Each factor contributes to the breakdown of energy balance in the body.
1. Malabsorption Due to Enzyme Deficiency
The pancreas produces enzymes that digest food. When a tumor impairs this function, it results in exocrine pancreatic insufficiency (EPI). Patients may eat adequately, but nutrients—especially fats—pass through the digestive system undigested, leading to steatorrhea (fatty stools), bloating, and weight loss.
2. Appetite Suppression
Inflammation caused by tumor cytokines suppresses the hypothalamic regulation of hunger. Many patients with advanced pancreatic cancer experience early satiety, nausea, or complete loss of interest in food, even in the absence of gastrointestinal obstruction.
3. Systemic Inflammation and Cachexia
Pro-inflammatory cytokines such as TNF-α and IL-6 accelerate protein breakdown and fat loss, even in well-nourished individuals. This catabolic state is resistant to simple calorie supplementation and often continues despite eating efforts.
4. Metabolic Demand of the Tumor
Cancerous cells are highly metabolically active. They draw energy from glucose and amino acids at a much higher rate than healthy cells, forcing the body into a chronic energy deficit. This is compounded in patients with larger or fast-growing tumors.
5. Treatment Side Effects
Chemotherapy, radiation, or novel interventions like NanoKnife Pancreatic Cancer ablation may reduce appetite or impair gastrointestinal comfort. Nausea, vomiting, diarrhea, and mucositis all contribute to insufficient caloric intake.
Understanding the multifactorial nature of weight loss allows clinicians to tailor treatment not just toward tumor control, but also metabolic and nutritional stabilization.
Danger Signs: When Weight Loss Requires Urgent Medical Attention
While some degree of weight loss may be expected during cancer treatment, there are warning signs that indicate more serious underlying issues. Recognizing them early is critical for timely intervention.
- Rapid weight loss (more than 5–10% in 1–2 months)
- Severe fatigue or weakness affecting mobility or daily activity
- Muscle wasting visible in limbs, shoulders, or back
- Loss of appetite for more than 5 days
- Signs of dehydration, including low urine output, dizziness, or dry mouth
- Steatorrhea or persistent diarrhea, indicating poor nutrient absorption
- Inability to tolerate food due to vomiting, pain, or early satiety
In the context of symptoms of cancer, any sudden or escalating weight loss should be treated as a clinical red flag. Such changes may signal progression, metabolic imbalance, or complications like bowel obstruction or treatment toxicity.
Healthcare providers often recommend prompt lab tests, imaging, and referral to a nutrition specialist when these signs appear, even mid-treatment. Addressing the issue early can prevent hospitalization and restore treatment eligibility.
How Weight Loss Is Diagnosed and Measured in Cancer Patients
Diagnosing and monitoring weight loss in cancer patients goes far beyond tracking the number on a scale. A comprehensive assessment is required to determine the severity and cause.
Body Weight History
Oncologists will compare the current weight to baseline measurements taken prior to diagnosis or during earlier stages of treatment. A loss of 5% or more within six months is clinically significant.
Body Mass Index (BMI) and Lean Muscle Mass
BMI can be misleading in cancer patients, especially if fluid retention masks actual tissue loss. More accurate assessments may include bioelectrical impedance analysis (BIA), DEXA scans, or CT-based body composition measurements to assess lean muscle mass.
Laboratory Tests
- Albumin and prealbumin levels are used to evaluate protein nutrition status.
- C-reactive protein (CRP) and interleukin-6 may signal systemic inflammation and cachexia.
- Fecal elastase testing helps diagnose exocrine pancreatic insufficiency.
Functional Assessment
Tools like the Karnofsky Performance Scale or Eastern Cooperative Oncology Group (ECOG) score help measure the physical impact of weight loss on daily life.
Early and ongoing evaluation is essential for initiating nutrition therapy, adjusting medications, or modifying treatment plans.
Treating and Managing Weight Loss in Pancreatic Cancer

Managing unintentional weight loss in pancreatic cancer requires a comprehensive approach that addresses both the underlying disease and its nutritional consequences. The goal is to preserve muscle mass, stabilize weight, and improve treatment tolerance.
1. Pancreatic Enzyme Replacement Therapy (PERT)
For patients with EPI, enzyme supplements like pancrelipase restore digestive function. This improves nutrient absorption and can lead to meaningful weight stabilization or gain.
2. Nutritional Counseling and Supplementation
Registered dietitians create high-calorie, high-protein meal plans tailored to the patient’s needs and tolerance. Oral nutritional supplements or fortified smoothies may be recommended for those with appetite challenges.
3. Appetite Stimulants and Pharmacologic Support
Medications like megestrol acetate or corticosteroids can stimulate appetite in selected patients. Anti-nausea drugs and acid reducers may also improve eating comfort.
4. Treatment Optimization
If a specific cancer therapy is causing severe GI side effects, dosage adjustments, therapy switches, or supportive medications (e.g., antidiarrheals) can reduce negative impact on weight.
5. Palliative and Integrative Care
Specialists in palliative care work with oncology teams to manage cachexia, pain, and energy deficits. Acupuncture, psychosocial support, and light exercise programs may enhance overall well-being.
When applied early, these interventions not only improve nutritional status but can extend survival and reduce hospitalizations in patients with advanced pancreatic cancer.
Can Weight Loss Be Prevented in Pancreatic Cancer Patients?
While complete prevention of weight loss in pancreatic cancer may not always be possible, especially in advanced cases, proactive measures can slow its progression and improve a patient’s overall condition. The key lies in early nutritional intervention and routine monitoring.
Early Detection and Monitoring
Routine weight tracking and body composition assessments during treatment can catch early signs of muscle or fat loss. Even minor changes in appetite or energy should be reported and addressed immediately.
Nutritional Planning from Diagnosis
Engaging a clinical dietitian at the time of diagnosis allows for the creation of an individualized nutrition plan. This might include high-protein meals, small frequent portions, and easy-to-digest foods to account for reduced pancreatic function.
Enzyme Replacement and Supplement Use
For patients with malabsorption, pancreatic enzyme replacement therapy (PERT) should be initiated early—even before symptoms of steatorrhea appear. Supplementing with fat-soluble vitamins (A, D, E, K) and omega-3 fatty acids may also support metabolic resilience.
Treatment Planning with Nutrition in Mind
Chemotherapy and procedures like NanoKnife Pancreatic Cancer ablation can be adjusted to reduce GI toxicity. Integrating supportive medications to control nausea, acid reflux, or delayed gastric emptying helps patients maintain intake during therapy.
Though weight loss is common, a proactive, multidisciplinary approach can delay or reduce the severity of cachexia and improve quality of life.
Will the Weight Return After Treatment?
Whether lost weight returns after cancer treatment depends on several factors: the stage of the disease, treatment outcome, and the degree of metabolic or muscular damage that occurred during therapy.
In Resectable or Early-Stage Disease
Patients who undergo surgery and achieve remission—especially those with stage I or II tumors—often regain weight within 6–12 months after treatment ends. With PERT and good dietary support, normal digestion can resume, leading to steady recovery.
In Advanced or Metastatic Cases
In patients with pancreatic cancer at stage III or IV, weight regain is more difficult due to ongoing inflammation, poor appetite, and reduced muscle reserves. In many of these cases, the goal shifts from regaining weight to maintaining strength and minimizing further loss.
After Immunotherapy or Local Ablation
Patients treated with less invasive therapies, such as NanoKnife Pancreatic Cancer, may experience fewer gastrointestinal side effects, improving their chance to stabilize weight during and after treatment.
Ultimately, patients who can control symptoms, eat comfortably, and receive proper enzyme support are most likely to regain or stabilize weight over time.
What Oncology Experts Say About Weight Loss in Pancreatic Cancer

According to leading oncologists and palliative care specialists, unintentional weight loss is one of the most challenging symptoms to manage in pancreatic cancer—and one of the most predictive of outcomes.
Dr. Elena Vargas, GI oncologist at MD Anderson, notes:
“Unexplained weight loss is often the first sign that brings patients into our clinics. By the time we diagnose pancreatic cancer, many have already lost 10% or more of their body weight, which impacts treatment tolerance and recovery.”
Dr. Michael Chan, a surgical oncologist, emphasizes:
“We’ve learned that addressing nutrition early—not as an afterthought—is critical. Patients receiving PERT, high-calorie meal support, and exercise therapy show better resilience, even with advanced symptoms of cancer like fatigue and weakness.”
Experts advocate for early involvement of dietitians, oncologic rehab teams, and palliative care professionals. They also stress that weight loss should be treated as a clinical complication, not a cosmetic or secondary issue—especially because it often signals deeper metabolic dysfunction.
15+ Frequently Asked Questions (FAQ)
1. Is weight loss always a sign of pancreatic cancer?
Not always. But if weight loss is unintentional, rapid, and combined with fatigue, jaundice, or digestive changes, it should be evaluated immediately for possible underlying causes like cancer.
2. How much weight loss is concerning?
Losing more than 5% of body weight within 6 months without trying is considered clinically significant and should prompt medical evaluation.
3. Can enzyme therapy really stop weight loss?
Yes, for many patients. Pancreatic enzyme replacement therapy improves nutrient absorption, reducing stool fat and improving calorie utilization.
4. Why does cancer cause loss of muscle, not just fat?
Cancer induces a catabolic state, where muscle breakdown is prioritized by inflammatory signals and energy demands—even if food intake is adequate.
5. Can cachexia be reversed?
In early stages, yes—especially with nutritional and pharmacologic support. In late stages, full reversal may not be possible, but stabilization is often achievable.
6. Is weight loss worse in certain stages of pancreatic cancer?
Yes. Advanced stages (III and IV) tend to show more severe cachexia due to higher metabolic burden and poor appetite.
7. Should patients exercise during treatment?
Light activity, such as walking or stretching, can help maintain muscle mass and improve energy levels. Always consult your care team first.
8. How can families help manage eating challenges?
Offer small, frequent, energy-dense meals without pressure. Focus on comfort foods the patient enjoys and adjust textures if chewing is difficult.
9. Do weight loss and malnutrition affect survival?
Yes. Severe weight loss correlates with reduced treatment response and shorter overall survival in pancreatic cancer.
10. Are appetite stimulants safe and effective?
In selected patients, medications like megestrol or corticosteroids may help. They should be used under supervision due to potential side effects.
11. When should I ask for a referral to a dietitian?
At the time of diagnosis, or as soon as weight loss, nausea, or appetite changes begin. Early intervention leads to better outcomes.
12. Is feeding tube placement common?
In cases of severe malnutrition or when oral intake fails, feeding tubes (PEG or jejunal) may be considered temporarily to stabilize nutrition.
13. What role does hydration play in managing weight?
Hydration helps support metabolism, prevent fatigue, and improve appetite. Dehydration worsens treatment side effects and energy loss.
14. Can alternative diets help with weight gain?
Only if supervised. High-fat or keto-style diets may harm patients with fat malabsorption. Individualized nutrition plans are safer.
15. Will weight return after successful treatment?
In early stages, yes. In advanced cases, weight may stabilize rather than return. Focus often shifts to maintaining strength and function.









