Unfavorable Intermediate-Risk Prostate Cancer: A Comprehensive Guide
- Understanding Prostate Cancer Risk Stratification
- Defining Unfavorable Intermediate-Risk Prostate Cancer
- Diagnostic Evaluation and Staging
- Treatment Options for Unfavorable Intermediate-Risk Prostate Cancer
- Combining Radiation and Hormonal Therapy in Treatment Plans
- Monitoring During and After Treatment
- Quality of Life Considerations Post-Treatment
- Genomic Classifiers and Risk Reassessment
- Impact of Comorbidities on Treatment Decisions
- Radiologic Evaluation and MRI in Risk Refinement
- Surgery Versus Radiation in This Subgroup
- Comparing Unfavorable Intermediate-Risk and High-Risk Prostate Cancer
- Importance of Gleason Score Patterns
- Role of Genomic Testing and Molecular Classifiers
- Hormonal Therapy Considerations and Duration
- Risk of Upgrading After Surgery
- Follow-Up Strategy After Primary Treatment
- Future of Personalized Therapy in Intermediate-Risk Prostate Cancer
- Psychosocial Impact and Support Mechanisms
- Summary and Final Considerations
- Survivorship and Long-Term Health Outcomes
- Frequently Asked Questions (FAQ)
Understanding Prostate Cancer Risk Stratification
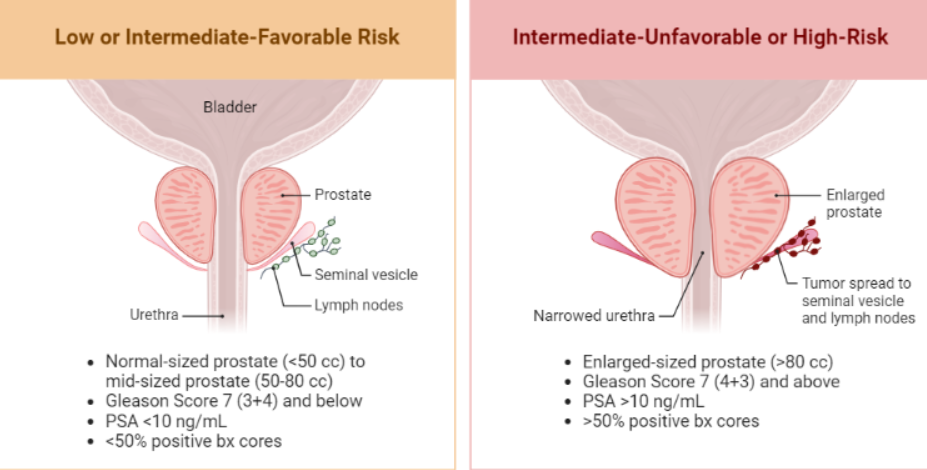
Prostate cancer is categorized into risk groups to guide treatment decisions and predict outcomes. The National Comprehensive Cancer Network (NCCN) classifies prostate cancer into low, intermediate, and high-risk categories based on prostate-specific antigen (PSA) levels, Gleason score, and tumor stage. Intermediate-risk prostate cancer is further subdivided into favorable and unfavorable groups to better tailor treatment approaches.
Defining Unfavorable Intermediate-Risk Prostate Cancer
Unfavorable intermediate-risk prostate cancer is characterized by one or more of the following features:
- Gleason score of 4+3=7
- PSA levels between 10-20 ng/mL
- Tumor stage T2b or T2c
- Multiple intermediate-risk factors
Patients in this category have a higher likelihood of disease progression compared to those with favorable intermediate-risk prostate cancer.
Diagnostic Evaluation and Staging
Accurate diagnosis and staging are crucial for effective management. Diagnostic procedures include:
- PSA Testing: Measures the level of prostate-specific antigen in the blood.
- Digital Rectal Exam (DRE): Assesses the prostate for abnormalities.
- Prostate Biopsy: Determines the Gleason score and cancer grade.
- Imaging Studies: MRI and CT scans evaluate the extent of the disease.
These assessments help in confirming the diagnosis and planning appropriate treatment strategies.
Treatment Options for Unfavorable Intermediate-Risk Prostate Cancer
Management of unfavorable intermediate-risk prostate cancer involves a combination of therapies tailored to the patient’s specific condition. Treatment options include:
- Radical Prostatectomy: Surgical removal of the prostate gland.
- External Beam Radiation Therapy (EBRT): Targets cancer cells with high-energy rays.
- Brachytherapy: Implantation of radioactive seeds directly into the prostate.
- Androgen Deprivation Therapy (ADT): Reduces androgen levels to slow cancer growth.
The choice of treatment depends on various factors, including patient age, overall health, and personal preferences.
Combining Radiation and Hormonal Therapy in Treatment Plans
For patients classified with unfavorable intermediate-risk prostate cancer, the integration of external beam radiation therapy (EBRT) and androgen deprivation therapy (ADT) has shown superior outcomes compared to radiation alone. Radiation therapy directly targets prostate tumors, while ADT lowers testosterone levels, which fuel prostate cancer growth.
Studies such as RTOG 9408 have demonstrated improved survival rates in patients who received both EBRT and short-term ADT. Typically, ADT is administered for 4–6 months in this subgroup, with the goal of reducing recurrence and improving local control.
A common point of discussion with patients is whether combining therapies leads to excessive side effects. While fatigue and sexual dysfunction are more prevalent, many clinicians consider these manageable and worthwhile, especially in younger men with otherwise long life expectancy. Interestingly, this therapeutic rationale echoes strategies used in other cancers where hormone-sensitive cells drive progression, such as in [breast cancer without a detectable lump](на этом месте ссылка).
Monitoring During and After Treatment
Active monitoring is crucial during and after the treatment of unfavorable intermediate-risk prostate cancer. PSA levels serve as a key biomarker for assessing response to therapy and detecting early recurrence. The standard follow-up schedule includes PSA testing every 3–6 months for the first two years and then every 6–12 months thereafter.
In addition to PSA, digital rectal exams (DRE) and occasional imaging may be warranted based on symptoms or rising PSA levels. MRI is the preferred modality for assessing local recurrence, while bone scans are typically reserved for those with significantly elevated PSA or symptoms suggestive of metastasis.
It’s essential to educate patients that a PSA “bounce” is common after radiation and does not necessarily indicate failure. Providing psychological support during this uncertain phase helps patients cope with anxiety, which is especially important when personal.
Quality of Life Considerations Post-Treatment
Managing life after treatment is just as important as choosing the right therapeutic path. Men treated for unfavorable intermediate-risk prostate cancer often report concerns around urinary incontinence, erectile dysfunction, fatigue, and emotional well-being. Recovery expectations should be discussed transparently during the decision-making process.
Some men benefit from pelvic floor physical therapy, medications for erectile function, or testosterone management under specialist supervision. Support groups and counseling also play a valuable role, especially for those struggling with identity and body image changes.
It’s critical to emphasize that many men with this risk group go on to live full, active lives. Survivorship care should be holistic, addressing physical, emotional, and sexual health—not just cancer surveillance.
Genomic Classifiers and Risk Reassessment
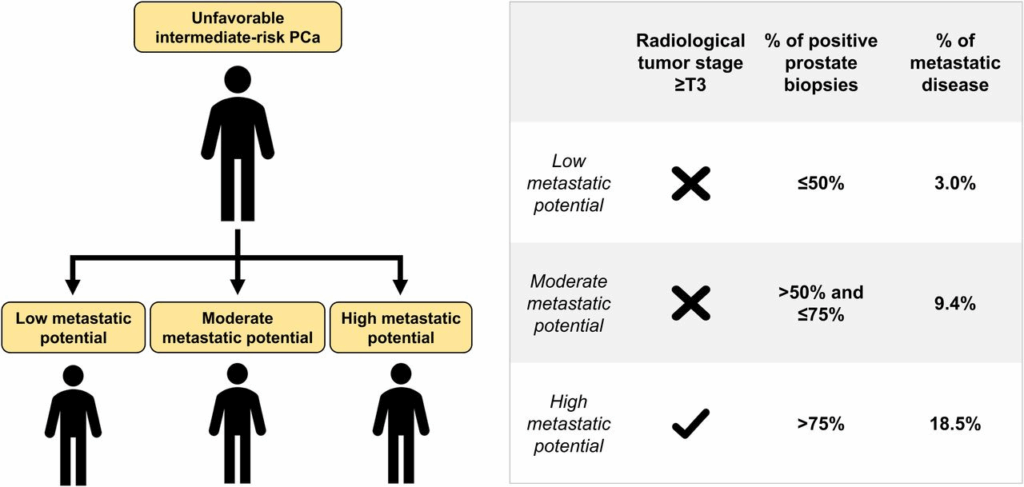
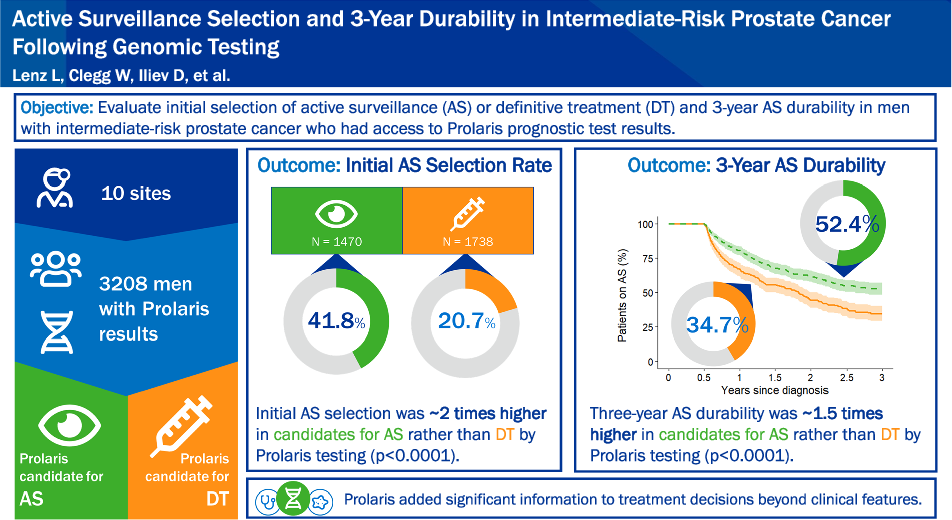
Recent years have seen the emergence of genomic testing as a decision-making tool in prostate cancer care. Tests such as Decipher, Prolaris, and Oncotype DX assess the biological aggressiveness of prostate tumors beyond clinical features alone.
In unfavorable intermediate-risk patients, these tests can refine risk estimates and guide the intensity of treatment. For instance, a patient with a high Decipher score might benefit from longer ADT or more aggressive radiation, while a low score might support de-escalation strategies.
Genomic classifiers also help differentiate which patients may progress toward high-risk or metastatic disease—important information when long-term planning includes secondary prevention or surveillance for related conditions like peritoneal metastasis in colon cancer.
Impact of Comorbidities on Treatment Decisions
Comorbidities play a crucial role in selecting appropriate therapies for men with unfavorable intermediate-risk prostate cancer. Conditions such as diabetes, cardiovascular disease, and chronic obstructive pulmonary disease (COPD) can significantly limit treatment options and tolerance.
For instance, androgen deprivation therapy (ADT) can worsen glycemic control in diabetics and increase thrombotic risk in those with heart disease. These considerations often prompt oncologists to favor radiation monotherapy or minimally invasive surgery for frailer patients.
Pre-treatment assessments, including the Charlson Comorbidity Index and geriatric screening tools, help guide individualized planning. Moreover, emerging risk calculators now integrate both tumor and patient health data, aiming to balance oncologic control with life expectancy and personal priorities.
Radiologic Evaluation and MRI in Risk Refinement
Modern radiologic imaging — especially multiparametric MRI (mpMRI) — has revolutionized how we stage and stratify prostate cancer. For unfavorable intermediate-risk disease, mpMRI aids in confirming extracapsular extension, seminal vesicle invasion, and suspicious lymph nodes.
These findings can reclassify patients into a higher risk category, directly impacting therapeutic choices such as the extent of radiation field or inclusion of pelvic lymph nodes. mpMRI also helps with biopsy targeting, improving diagnostic accuracy and reducing misclassification.
When compared to standard TRUS (transrectal ultrasound), mpMRI provides superior anatomical detail, especially in anterior tumors or lesions near the apex. The integration of mpMRI findings into the clinical decision process is now standard at many centers of excellence.
Surgery Versus Radiation in This Subgroup
The decision between radical prostatectomy and radiation therapy remains controversial in the unfavorable intermediate-risk cohort. While both modalities offer curative potential, their risk profiles and post-treatment side effects differ substantially.
Surgery provides pathologic staging, which can further guide adjuvant therapies. It also removes the prostate in totality, which may be preferred by younger, healthier patients. However, it carries risks of urinary incontinence and erectile dysfunction.
Radiation therapy, particularly when combined with short-course ADT, offers equivalent oncologic outcomes in many studies. It is often preferred in older patients or those with higher surgical risk. Shared decision-making, informed by PSA kinetics, MRI findings, and biopsy data, remains essential.
This dilemma of choosing optimal primary therapy is not unlike the complexity surrounding colon cancer peritoneal metastases, where treatment depends on disease burden, genetics, and overall functional status.
Comparing Unfavorable Intermediate-Risk and High-Risk Prostate Cancer
| Feature | Unfavorable Intermediate-Risk | High-Risk |
| PSA Level | 10–20 ng/mL | >20 ng/mL |
| Gleason Score | 4+3=7 | 8–10 |
| Biopsy Core Involvement | >50% | Often extensive |
| Number of Risk Factors | 2 or more intermediate-risk features | At least 1 high-risk feature |
| Risk of Recurrence | Moderate | High |
| Preferred Treatment | RT + short-term ADT or surgery | RT + long-term ADT ± chemotherapy |
| Molecular Testing Recommended? | Often | Strongly Recommended |
| Role of Genomics | Helpful for clarification | Often decisive for therapy selection |
Importance of Gleason Score Patterns
Within the intermediate-risk category, the Gleason scoring system plays a pivotal role in prognostication. Unfavorable intermediate-risk prostate cancer typically includes a Gleason score of 4+3, rather than 3+4. This subtle reversal reflects a predominance of poorly formed or fused glands, indicating a more aggressive histological profile.
Gleason 4+3 tumors are more likely to show extraprostatic extension and a higher incidence of positive surgical margins. These patients have increased risks of biochemical recurrence after both radiation and surgery. As a result, they are often managed similarly to high-risk patients, with more aggressive treatment strategies and closer follow-up.
Histopathologic review by experienced genitourinary pathologists is essential, especially if initial biopsies were performed at smaller centers with less expertise.
Role of Genomic Testing and Molecular Classifiers
Genomic tools such as Decipher®, Prolaris®, and Oncotype DX® are increasingly used to clarify prognosis in men with unfavorable intermediate-risk disease. These assays evaluate expression patterns of dozens of cancer-related genes, offering insights beyond standard histology.
A patient with a borderline risk profile may be reclassified based on these molecular signatures, influencing decisions on adding ADT, extending radiation fields, or even considering active surveillance in select low-aggression cases. Furthermore, these tests provide a quantitative recurrence risk score, helping guide follow-up intensity and imaging frequency.
It’s worth noting that similar genomic testing is also being applied in breast malignancies, especially in cases where no mass is found on palpation.
Hormonal Therapy Considerations and Duration
Androgen deprivation therapy (ADT) is a key component in treating unfavorable intermediate-risk prostate cancer, especially when combined with external beam radiation therapy (EBRT). Most guidelines recommend 4 to 6 months of ADT, which has been shown to improve progression-free survival without excessive toxicity.
Short-course ADT reduces testosterone levels, slowing tumor growth and enhancing radiation sensitivity. However, side effects such as fatigue, hot flashes, libido loss, and metabolic disturbances must be monitored. Newer agents like GnRH antagonists may offer fewer cardiovascular risks than traditional LHRH agonists, making them preferable in patients with cardiac history.
Duration should be personalized based on response indicators, tolerability, and patient comorbidities.
Risk of Upgrading After Surgery
Despite pre-treatment risk stratification, final pathology after radical prostatectomy may reveal a more advanced or aggressive cancer than initially suspected — a phenomenon known as “upgrading.” This occurs in approximately 25–35% of men with unfavorable intermediate-risk features.
Upgrading often results from under-sampling during biopsy or hidden high-grade disease within the prostate. These findings can affect decisions about adjuvant radiation, extended hormone therapy, and surveillance imaging. High-volume surgical centers typically report more accurate correlations between biopsy and final pathology.
Interestingly, genetic predisposition and family history — such as in families with hereditary myeloma — may correlate with more biologically aggressive behavior in prostate cancer as well.
Follow-Up Strategy After Primary Treatment
Once definitive treatment is completed—be it surgery, radiation, or a combination—ongoing surveillance becomes critical for early detection of recurrence. The cornerstone of follow-up is serial PSA testing, typically every 3–6 months for the first 2 years, then every 6–12 months thereafter.
In post-prostatectomy patients, any detectable PSA warrants investigation, while those treated with radiation are monitored for a rise of 2 ng/mL above the nadir. Additionally, digital rectal exams may still be useful in some cases, particularly after radiation therapy.
Advanced imaging, such as PSMA PET scans, is increasingly used if recurrence is suspected. The goal is to detect early relapse when salvage therapy has the highest chance of success.
Future of Personalized Therapy in Intermediate-Risk Prostate Cancer
Precision approaches are redefining treatment standards
The future of managing unfavorable intermediate-risk prostate cancer lies in personalization. Molecular profiling and gene-expression analysis now provide oncologists with tools to differentiate indolent tumors from aggressive ones even within the same clinical category. This enables tailored treatment intensity — for instance, determining whether a patient might benefit from short-course ADT versus long-course, or if radiation margins can be minimized to reduce side effects.
New therapeutic paradigms on the horizon
Several trials are testing focal therapies such as high-intensity focused ultrasound (HIFU) and irreversible electroporation in well-characterized intermediate-risk groups. While traditionally reserved for low-risk disease, these modalities may offer a middle-ground solution in highly selected unfavorable intermediate-risk cases, especially where the patient profile contraindicates standard interventions.
Incorporating digital and AI tools
Artificial intelligence and machine learning algorithms are emerging to predict recurrence risk and treatment response based on imaging and pathology datasets. By enhancing prognostic accuracy, they assist physicians in navigating the nuanced treatment spectrum of intermediate-risk disease.
Psychosocial Impact and Support Mechanisms
Emotional toll of an “intermediate” label
Being classified as “unfavorable intermediate-risk” creates a dual emotional burden. On one hand, it’s not the worst-case scenario, but on the other, the risk of progression is real. Patients often describe feeling caught in a gray zone — unsure if they should be worried or reassured. This ambiguity can lead to heightened anxiety, decisional regret, and stress.
Importance of counseling and peer networks
Timely referral to psycho-oncology services, mental health counseling, and survivorship support groups is essential. These avenues not only improve quality of life but can also influence adherence to therapy, especially when long-term side effects are involved. Sharing experiences with others facing similar diagnoses — including those with breast cancer without a lump, who often deal with uncertainty — can foster understanding and emotional resilience.
Summary and Final Considerations
Unfavorable intermediate-risk prostate cancer is a heterogeneous entity that demands personalized management. Accurate staging, detailed histopathology, and appropriate integration of imaging and genomic tools are essential. Treatment choices—between surgery, radiation, and hormonal therapy—must be tailored to the patient’s biology, comorbidities, and preferences.
Effective long-term management hinges not only on the right therapy but on vigilant surveillance, emotional support, and lifestyle integration. As our understanding deepens, the lines between intermediate and high-risk categories may continue to evolve.
By maintaining a multidisciplinary approach, we can achieve both oncologic success and a high quality of life for these patients.
Survivorship and Long-Term Health Outcomes
What happens after primary treatment?
After curative-intent therapy (surgery or radiation), the focus shifts to survivorship. Many men live long, healthy lives, but close monitoring is crucial, especially in the first 5 years. PSA monitoring, lifestyle adjustments, and management of any lasting side effects — like urinary incontinence or erectile dysfunction — form the core of follow-up care.
Managing comorbidities and general health
Men treated for intermediate-risk prostate cancer are often older and may already have hypertension, diabetes, or cardiac concerns. It becomes vital to coordinate urologic oncology care with primary and cardiology care. Long-term survival isn’t just about cancer recurrence — cardiovascular events are also a leading cause of mortality in these patients.
Linking survivorship to family and hereditary insights
Recent studies are exploring whether relatives of patients with intermediate-risk profiles have elevated risks for other malignancies. In a similar way, those affected by medullary thyroid cancer with microcalcifications are now part of genetic counseling pathways.
Frequently Asked Questions (FAQ)
What defines unfavorable intermediate-risk prostate cancer?
Unfavorable intermediate-risk prostate cancer includes patients with clinical stage T2b–T2c, a Gleason score of 4+3=7, or PSA between 10–20 ng/mL, particularly when multiple intermediate-risk features are present. These cases often exhibit more aggressive biological behavior than favorable intermediate-risk disease.
How does Gleason 4+3 differ from 3+4 in prostate cancer?
While both sum to Gleason score 7, 4+3 indicates a higher proportion of poorly formed cancer glands, suggesting a more aggressive tumor. This pattern is associated with higher recurrence rates and a greater likelihood of extracapsular extension or seminal vesicle invasion.
Can patients with unfavorable intermediate-risk disease undergo active surveillance?
Generally, active surveillance is not recommended for this group due to the higher risk of progression. However, ongoing trials are exploring whether select patients with favorable genomic profiles might safely defer treatment.
Is surgery or radiation better for this risk group?
Both radical prostatectomy and radiation therapy with short-term ADT are considered appropriate. The choice depends on patient comorbidities, preferences, and potential side effects. Some evidence suggests radiation with ADT may offer better biochemical control.
What role does androgen deprivation therapy (ADT) play?
ADT is commonly used with radiation in unfavorable intermediate-risk cases. A short course (4–6 months) improves outcomes by enhancing radiosensitivity and suppressing tumor growth. ADT is usually not required with surgery unless high-risk features are found postoperatively.
What are the chances of upgrading after surgery?
Approximately 25–35% of patients with intermediate-risk disease are upgraded to higher Gleason scores upon examination of the prostate specimen after surgery. This underscores the limitations of needle biopsy and the importance of thorough pathological assessment.
How is recurrence monitored after treatment?
PSA testing is the primary surveillance tool, performed every 3–6 months for the first 2 years, then every 6–12 months. Rising PSA levels may indicate recurrence and prompt further imaging or salvage therapy.
What is the life expectancy for patients with this diagnosis?
With appropriate treatment, many men live 10–15 years or more, particularly if the disease is confined to the prostate. Prognosis depends on the presence of adverse features, comorbidities, and response to therapy.
How do genomics influence treatment decisions?
Genomic classifiers like Decipher or Prolaris assess tumor aggressiveness beyond Gleason score, helping guide whether to add ADT, extend radiation, or consider closer follow-up. They add precision to treatment planning.
Are there side effects from radiation and hormone therapy?
Yes. Radiation may cause bowel or urinary issues, while ADT can lead to fatigue, hot flashes, weight gain, and reduced libido. These effects are usually manageable but must be considered when planning therapy.
How does this diagnosis affect quality of life?
Many men experience emotional distress, changes in sexual function, and anxiety about recurrence. Support groups, psychological counseling, and open communication with healthcare providers can greatly improve coping and adjustment.
What imaging is used in evaluation or follow-up?
MRI is often used for local staging, while PSMA PET scans are increasingly used in recurrence assessment. Bone scans or CT may be indicated if high-risk features are present or PSA is rising after treatment.
Can lifestyle changes influence prognosis?
Healthy lifestyle habits—like a balanced diet, regular exercise, and smoking cessation—can support treatment tolerance and reduce cardiovascular risks, especially during ADT. While they don’t replace treatment, they contribute to overall wellness.
How does this compare to other cancers with intermediate behavior?
Unfavorable intermediate-risk prostate cancer shares a transitional nature with conditions like colon cancer metastasis to the peritoneum, where individualized treatment and staging remain critical.
What’s next in research for this patient group?
Future studies are focusing on molecular subtyping, focal therapies, and risk-adaptive treatment regimens. The goal is to refine intermediate-risk categorization and reduce overtreatment while maintaining excellent survival.









