Understanding Early Stage Eyelid Cancer Through Clinical Images and Medical Insight
- What Is Eyelid Cancer and Why Early Detection Matters
- Most Common Types of Eyelid Cancer
- Early Stage Eyelid Cancer Pictures: What They Show
- Differentiating Benign vs Malignant Eyelid Lesions
- Risk Factors for Eyelid Cancer Development
- Diagnosing Eyelid Cancer in Its Early Stage
- Treatment Options for Early Stage Eyelid Cancer
- Eyelid Cancer vs Other Skin Cancers: Key Differences
- Prognosis of Eyelid Cancer When Detected Early
- The Role of Imaging in Staging and Management
- Reconstructive Surgery After Tumor Excision
- Preventive Measures and Early Warning Signs
- Public Awareness and Misconceptions About Eyelid Cancer
- Comparing Eyelid Cancer to Other Facial Skin Cancers
- Long-Term Management and Surveillance
- Integrating Early Detection Strategies into Eye Care
- FAQ
What Is Eyelid Cancer and Why Early Detection Matters
The Role of the Eyelid in Ocular Health
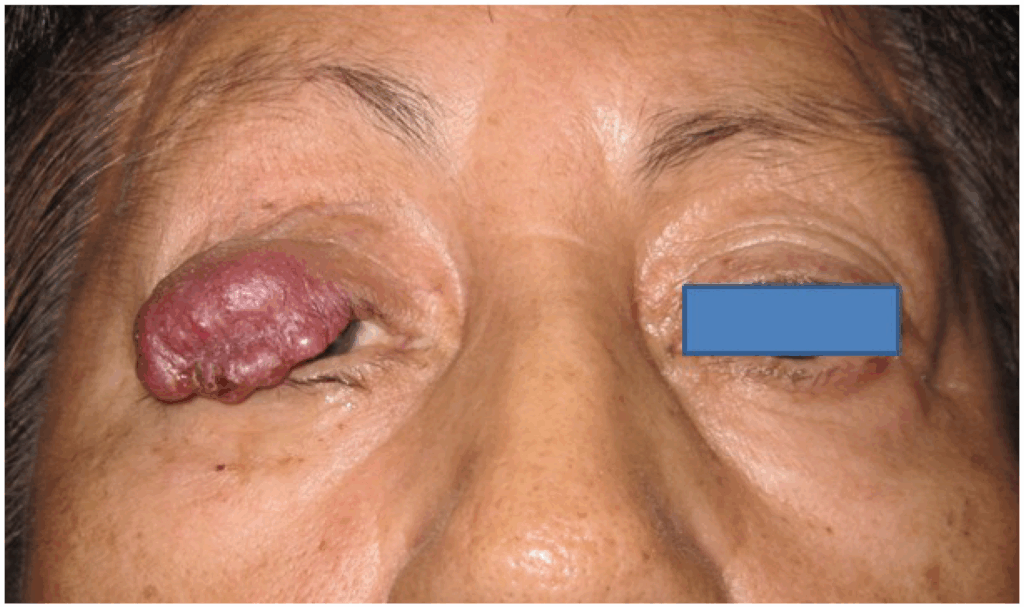
Eyelid cancer is a malignant growth originating in the tissues of the eyelid. Although rare compared to other forms of skin cancer, it can have profound implications for both vision and facial structure due to the eyelid’s anatomical and functional importance. The eyelids are responsible for protecting the eye, distributing tears, and facilitating blinking. A cancerous lesion in this area risks invading the orbit, affecting nearby lymph nodes, or damaging the tear drainage system.
Early-stage eyelid cancer is often localized and highly treatable, making prompt recognition essential. However, its initial appearance may mimic benign lesions like styes, chalazions, or age-related skin changes. Failure to identify and treat it early can result in tissue destruction, visual impairment, and metastasis to nearby structures. Early detection is therefore not just about aesthetics—it’s about preserving vision and preventing local spread.
Most Common Types of Eyelid Cancer
Basal Cell Carcinoma Leads the Statistics
Basal cell carcinoma (BCC) is the most prevalent form of eyelid cancer, representing about 85–90% of cases. It typically arises on the lower eyelid due to cumulative sun exposure and usually grows slowly. BCCs are rarely metastatic but can become locally destructive if untreated, especially near the medial canthus where they may invade the lacrimal system or orbit.
Other less frequent types include squamous cell carcinoma (SCC), sebaceous gland carcinoma, and melanoma. SCCs tend to be more aggressive than BCCs and may ulcerate or spread to lymphatic tissue. Sebaceous gland carcinoma is particularly deceptive, often masquerading as recurrent chalazions or blepharitis. Melanoma, while exceedingly rare on the eyelid, is the most dangerous due to its high metastatic potential.
Understanding the histologic origin of these cancers is key to recognizing their behavior, growth patterns, and likelihood of recurrence. Physicians rely on biopsy and imaging to confirm the diagnosis, as the clinical appearance can vary considerably.
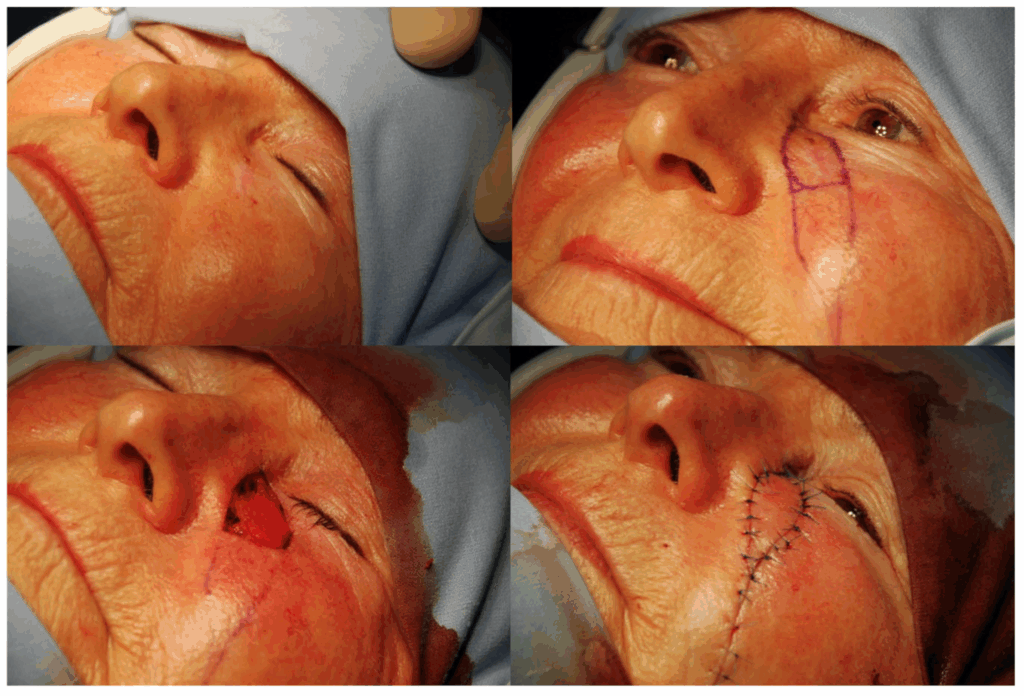
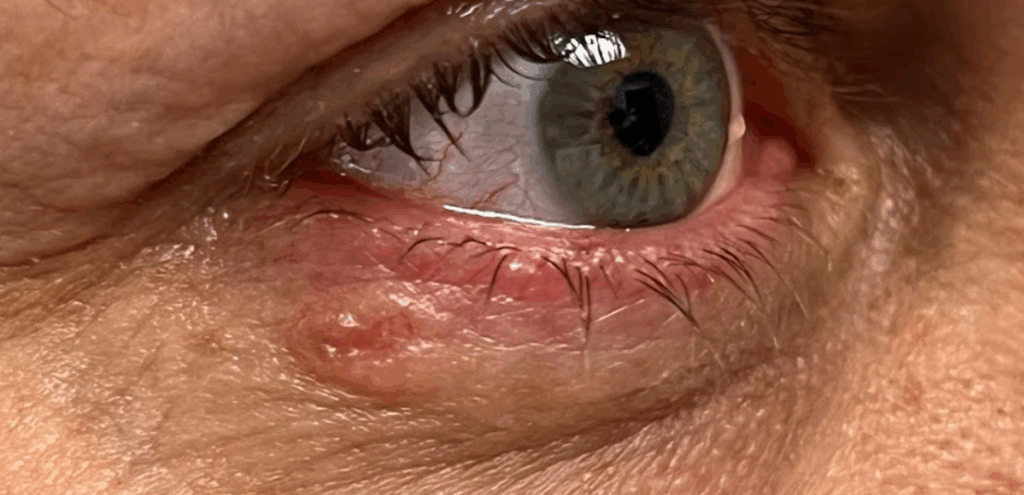
Early Stage Eyelid Cancer Pictures: What They Show
Recognizing Visual Cues in Clinical Context
Early-stage eyelid cancer may appear subtle, especially in its nascent forms. High-resolution clinical images often reveal small nodules, raised lesions, or skin thickening that might otherwise be dismissed. Some common visual characteristics include:
- Pearly or translucent nodules with visible capillaries (typical of BCC)
- Flat, scaly plaques that may crust or ulcerate (more typical of SCC)
- Yellowish nodules mimicking cysts (seen in sebaceous carcinoma)
- Irregular pigmentation or asymmetry in darker lesions (suggestive of melanoma)
Photographic comparisons with benign conditions are crucial for clinical education. For example, a stye or chalazion may resolve over weeks, whereas an eyelid carcinoma persists, evolves in shape, or begins to ulcerate. Dermoscopic images or high-contrast lighting can further highlight surface characteristics like telangiectasia or rolled borders.
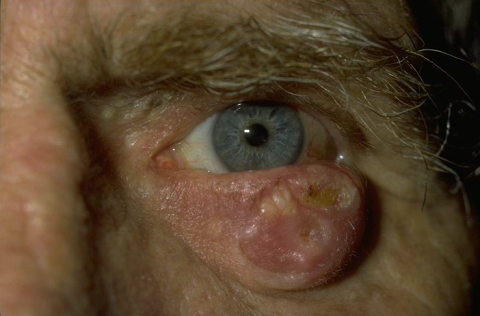
Differentiating Benign vs Malignant Eyelid Lesions
Clinical and Histological Distinction
To avoid misdiagnosis, clinicians must be trained to differentiate early-stage cancer from benign lesions. Chalazions, styes, papillomas, and even actinic keratoses can resemble malignancies in certain stages. Unlike benign lesions that usually resolve or remain stable, cancerous lesions persist, evolve, or bleed.
A biopsy remains the gold standard in confirming malignancy, but initial clinical clues may include chronicity, irregular margins, loss of eyelashes, and distortion of lid architecture. Dermoscopy and optical coherence tomography (OCT) are increasingly used to evaluate skin depth and vascular patterns.
Below is a table comparing benign and malignant features:
| Feature | Benign Lesions | Malignant Eyelid Lesions |
| Duration | Resolves within weeks | Persists or slowly enlarges |
| Appearance | Symmetric, well-demarcated | Irregular, asymmetric |
| Symptoms | Painful (e.g., styes) | Usually painless, but ulcerative |
| Eyelash Involvement | Usually intact | May cause lash loss or misdirection |
| Ulceration or Bleeding | Rare | Possible, especially in SCC |
| Growth Behavior | Static or regressing | Progressive |
By combining clinical expertise with image-based recognition, dermatologists and ophthalmologists can confidently diagnose early-stage cancers and initiate timely intervention.
Risk Factors for Eyelid Cancer Development
UV Exposure and Beyond
The most significant risk factor for developing eyelid cancer is prolonged ultraviolet (UV) radiation exposure. This is especially relevant for the lower eyelid, which receives the most sun due to its anatomical orientation. UV light can induce DNA mutations in skin cells over time, triggering carcinogenic pathways, particularly in fair-skinned individuals or those with a history of severe sunburns.
Other risk factors include advancing age, immunosuppression (such as in transplant recipients or those undergoing chemotherapy), and a personal or family history of skin cancer. Exposure to radiation, chronic inflammatory eye diseases, and certain genetic disorders like xeroderma pigmentosum also raise risk.
Notably, individuals with chronic eyelid inflammation or previous trauma in the periocular region may develop cancerous changes as part of long-term tissue degeneration. Wearing protective sunglasses and applying broad-spectrum sunscreen around the eyes remain essential for prevention, especially in high-risk individuals. “7 symptoms of colon cancer in women” – both topics highlight how important it is to know the early signs of cancer in vulnerable areas of the body.
Diagnosing Eyelid Cancer in Its Early Stage
The Process of Clinical Confirmation
The diagnostic pathway for eyelid cancer begins with a detailed history and physical examination. When a suspicious lesion is observed, clinicians assess the lesion’s duration, progression, appearance, and associated symptoms such as bleeding or lash loss. Given the similarity to benign conditions, confirmation through biopsy is essential.
An incisional biopsy is often performed to remove a small tissue sample for histopathological analysis. In certain cases, especially if malignancy is strongly suspected, an excisional biopsy may be preferred to remove the entire lesion. This sample is then analyzed for cellular atypia, invasive patterns, and cancer subtype classification.
Advanced imaging such as high-frequency ultrasound or MRI may be used to evaluate tumor depth, orbital invasion, or regional lymph node involvement. Sentinel lymph node biopsy is rare in eyelid cancers but may be considered in aggressive subtypes like sebaceous carcinoma or melanoma.
Prompt diagnosis not only improves outcomes but also reduces the risk of disfiguring surgical interventions. When eyelid cancer is caught in the early stage, treatment is usually highly successful.
Treatment Options for Early Stage Eyelid Cancer
Balancing Oncologic Control and Cosmetic Function
The primary goal in managing early eyelid cancer is to completely remove malignant cells while preserving eyelid structure and function. Surgical excision remains the gold standard, often performed using Mohs micrographic surgery. This technique allows for precise removal of cancerous tissue with minimal damage to surrounding healthy skin, making it ideal for delicate facial areas.
For small or superficial tumors, cryotherapy or radiation therapy may be employed, particularly in patients who are poor surgical candidates. Radiation is effective for tumors that cannot be fully excised or those recurring after surgery. Topical chemotherapeutic agents such as 5-fluorouracil or imiquimod are occasionally used for superficial basal cell carcinoma but are rarely employed in the periocular area due to the risk of ocular toxicity.
Sebaceous and squamous cell carcinomas often require more aggressive management due to their higher metastatic potential. In rare cases, adjunct therapies such as lymph node dissection or systemic chemotherapy may be necessary.
Surgical planning involves ophthalmologists and oculoplastic surgeons to ensure functional eyelid reconstruction. Techniques such as flap rotation or skin grafts are used to maintain eyelid closure, blinking, and tear film integrity.

Eyelid Cancer vs Other Skin Cancers: Key Differences
Why Location Matters Clinically
While basal cell and squamous cell carcinomas occur throughout sun-exposed skin, eyelid cancers are uniquely challenging due to the region’s anatomical complexity and cosmetic sensitivity. The eyelid houses delicate structures like the meibomian glands, tear ducts, and orbital rim, which can be affected even by small tumors.
Unlike skin cancers on the trunk or limbs, those on the eyelid pose a higher risk of affecting ocular function, vision, and facial symmetry. This mandates a multidisciplinary approach that includes dermatologists, oncologists, and oculoplastic surgeons.
Moreover, the close proximity of the eyelid to the brain and lymphatic pathways raises concern for rapid local invasion. Thus, even early-stage lesions warrant urgent and precise treatment. Failure to intervene early may result in loss of the eye or extensive reconstructive surgery. “Can cancer cause low phosphate levels” – reminding that even seemingly local types of cancer can affect the general condition of the body.
Prognosis of Eyelid Cancer When Detected Early
Survival Rates and Long-Term Outlook
When diagnosed at an early stage, eyelid cancer generally has an excellent prognosis, particularly in the case of basal cell carcinoma (BCC), which grows slowly and is rarely metastatic. Surgical removal in these cases often leads to complete cure, with five-year survival rates exceeding 95% for localized BCCs.
For squamous cell carcinoma (SCC), early-stage detection also significantly improves outcomes, though the recurrence rate is somewhat higher than with BCC. The prognosis becomes more guarded if SCC spreads to the lymphatic system or shows perineural invasion.
Sebaceous gland carcinoma poses more challenges due to its deceptive appearance and greater tendency for local recurrence or distant metastasis, especially if diagnosis is delayed. Early intervention, however, greatly increases the likelihood of complete removal and long-term control.
Regular follow-up is essential in all cases, even after apparently successful treatment. Recurrence, while rare, can occur several years later, and early-stage re-treatment offers a better functional and cosmetic result.
The Role of Imaging in Staging and Management
Tools for Defining Extent and Invasion
In early-stage eyelid cancer, imaging is not always necessary if the tumor is small and clearly superficial. However, when deeper invasion is suspected, advanced imaging techniques help define the tumor’s extent and guide treatment planning.
High-frequency ultrasound is particularly useful in evaluating soft tissue involvement around the lesion. MRI offers excellent contrast resolution for detecting perineural spread, orbital invasion, or proximity to critical structures such as the lacrimal gland. CT scans are employed when bony involvement is suspected, especially in more aggressive or neglected lesions.
Imaging becomes essential in sebaceous gland carcinoma or when melanoma is suspected, as both can metastasize to regional lymph nodes or distant organs. PET-CT may be indicated in those cases to assess metabolic activity and detect occult spread.
These imaging modalities provide a roadmap for surgeons, radiotherapists, and oncologists, reducing the risk of incomplete excision and improving long-term outcomes.
Reconstructive Surgery After Tumor Excision
Balancing Aesthetic Restoration and Functional Recovery
Post-excisional reconstruction is often required after removal of eyelid cancers, especially when large portions of the lid are affected. The eyelid is a structurally complex organ that must maintain mobility, closure, and protection of the globe. Successful reconstruction aims to restore these functions while minimizing cosmetic deformity.
Depending on the size and location of the defect, techniques include local flaps, composite grafts, and tarsoconjunctival flaps. For small defects, primary closure or advancement flaps are sufficient. Larger defects may require multi-stage reconstructions involving grafts from the upper lid, cheek, or even ear cartilage to rebuild structural integrity.
Oculoplastic surgeons are integral to this process. Their understanding of both aesthetic principles and ocular anatomy allows for tailored solutions that preserve blink reflex, corneal coverage, and eyelid alignment.
Patient outcomes are typically excellent when managed by an experienced team, and many individuals regain full eyelid function without visible scarring or disfigurement.
Preventive Measures and Early Warning Signs
Empowering Patients with Knowledge
Prevention and early detection go hand in hand in reducing the burden of eyelid cancer. Protective behaviors—like wearing sunglasses with full UV protection, applying sunscreen near the eyes, and avoiding tanning beds—can reduce risk significantly. Early skin surveillance, especially in fair-skinned individuals or those with a history of skin cancer, allows for prompt identification of suspicious changes.
Patients should be educated on early warning signs: persistent nodules on the eyelid margin, ulceration, lash loss, distortion of lid shape, or unexplained bleeding. Regular self-examination and prompt dermatological evaluation for any new or changing lesion are essential habits.
Educational outreach—especially among elderly populations who are most at risk—can also aid in reducing the number of advanced cases. Eye care professionals, including optometrists, should be trained to identify suspect lesions during routine exams. “Pili multigemini cancer” – as an example of how seemingly unusual but benign conditions can be mistaken for malignant.
Public Awareness and Misconceptions About Eyelid Cancer
Challenges in Patient Education
Despite its seriousness, eyelid cancer often goes unrecognized by the public. Many patients mistake early symptoms for styes, chalazions, or signs of aging. Media attention typically focuses on melanoma or breast cancer, leaving periocular cancers under-discussed. This lack of awareness delays diagnosis, especially in non-dermatological settings like primary care or routine eye exams.
There is also a misconception that cancers around the eye are cosmetic issues rather than functional threats. However, these lesions can impair blinking, vision, and tear regulation, making them both medically and aesthetically significant.
Raising awareness requires collaboration between dermatologists, ophthalmologists, and primary care providers. Public campaigns that include actual early-stage photos—appropriately labeled and contextualized—could encourage earlier self-referral and better outcomes.
Comparing Eyelid Cancer to Other Facial Skin Cancers
| Feature | Eyelid Cancer | Facial Basal Cell Carcinoma | Facial Squamous Cell Carcinoma |
| Common Locations | Lower eyelid, medial canthus | Nose, cheeks, forehead | Cheeks, lips, ears |
| Risk of Vision Impact | High | Low | Low to Moderate |
| Surgical Complexity | High | Moderate | Moderate |
| Need for Reconstructive Surgery | Frequent | Occasional | Occasional |
| Cosmetic Sensitivity | Very high | High | Moderate |
| Common Misdiagnosis | Stye, chalazion | Acne, scar tissue | Keratosis |
| Delay in Diagnosis | Common | Less common | Variable |
This comparison helps underscore how eyelid cancer, while biologically similar to other skin cancers, poses unique diagnostic and therapeutic challenges due to its anatomical setting and cosmetic implications.
Long-Term Management and Surveillance
Why Follow-Up Matters Even After a “Cure”
Even after successful treatment of early-stage eyelid cancer, long-term follow-up is essential. Recurrence is possible, particularly with more aggressive types like sebaceous gland carcinoma or squamous cell carcinoma. Regular dermatologic and ophthalmologic surveillance ensures prompt identification of any new lesions or subtle changes at the excision site.
Follow-up typically includes periodic physical exams, patient education for self-monitoring, and in some cases, imaging. High-risk patients—those with genetic syndromes, prior radiation exposure, or a history of multiple skin cancers—may require more frequent evaluations.
Surveillance plans are customized to the type of cancer, treatment modality used, and margin status after excision. Patients are encouraged to report any persistent redness, lumps, asymmetry, or discomfort in the eyelid area, even years after the initial diagnosis. “Is bowel leakage a sign of cancer” – both topics raise the importance of regular monitoring following subtle but clinically significant symptoms.
Integrating Early Detection Strategies into Eye Care
A Call for Collaborative Screening
To improve outcomes, early detection strategies must be integrated into routine ophthalmic care. Eye care providers are uniquely positioned to observe changes in the eyelids and periocular region, often before symptoms develop. Routine dilated eye exams should include a careful external inspection of the eyelids.
Interdisciplinary collaboration between optometrists, ophthalmologists, and dermatologists can help close the gap between early suspicion and confirmed diagnosis. This is especially important in elderly patients, where lesions may progress rapidly or be ignored due to poor vision or reduced self-care capacity.
Training modules for optometry and general practice should include image-based education to recognize red-flag signs of malignancy. With more providers trained to recognize early-stage eyelid cancer, overall detection rates and outcomes can improve significantly.
FAQ
What does early-stage eyelid cancer look like?
It may present as a small, firm bump, discolored patch, ulcer, or scaly area, often resembling benign lesions like a stye or chalazion.
Is eyelid cancer painful?
Most early-stage eyelid cancers are not painful. Pain may develop later if the tumor invades deeper tissues or becomes ulcerated.
How common is eyelid cancer?
Eyelid cancer is relatively rare but increasing in incidence due to better screening and increased sun exposure over decades.
Which type of eyelid cancer is most dangerous?
Sebaceous gland carcinoma and melanoma are the most aggressive, while basal cell carcinoma is the most common and slow-growing.
Can eyelid cancer be treated without surgery?
In select superficial cases, radiation or topical treatments may help, but surgery remains the most reliable and curative option.
Does eyelid cancer cause vision loss?
If untreated, it can invade ocular structures and result in vision impairment, especially when near the tear ducts or orbital rim.
Can children get eyelid cancer?
It is extremely rare in children; the condition primarily affects adults over 50, especially those with cumulative sun damage.
How long does surgery recovery take?
Most patients recover within 2–4 weeks, depending on the extent of reconstruction. Swelling and bruising usually resolve quickly.
Are there warning signs before it becomes serious?
Yes—persistent growth, asymmetry, lash loss, or bleeding are early signs that warrant immediate evaluation.
Is eyelid cancer linked to other cancers?
Not directly, but people with a history of other skin cancers or genetic syndromes may be at higher risk for multiple types.
Can I prevent eyelid cancer?
Wearing sunglasses with UV protection, using sunscreen, and avoiding tanning beds reduce your lifetime risk significantly.
What doctor should I see for a suspicious eyelid lesion?
Start with a dermatologist or ophthalmologist. If cancer is suspected, they will refer you to an oculoplastic or surgical oncologist.
Can makeup or skin products cause eyelid cancer?
There is no proven link. The main risk factors remain UV exposure, age, and genetic predisposition.
What is Mohs surgery and is it used for eyelids?
Yes, Mohs surgery allows precise excision of skin cancers with minimal damage to surrounding tissue—ideal for eyelid tumors.
How often should I get checked after eyelid cancer treatment?
Follow-up every 6–12 months is typical, but high-risk patients may need more frequent monitoring.













