Triple-Negative Breast Cancer: What Makes It So Aggressive?
- Foreword
- Part 1: What Is Triple-Negative Breast Cancer?
- Part 2: Why Is Triple-Negative Breast Cancer So Aggressive?
- Part 3: How Triple-Negative Breast Cancer Is Diagnosed
- Part 4: Treatment Options for Triple-Negative Breast Cancer
- Part 5: Prognosis and Survival Rates
- Part 6: FAQs About Triple-Negative Breast Cancer
- Wrapping Up the FAQs
- Part 7: Final Thoughts
Foreword
Receiving a diagnosis of triple-negative breast cancer (TNBC) can feel overwhelming. The term “triple-negative” might sound intimidating, and for many, it brings up questions that might not have easy answers. Why is TNBC so aggressive? Why are there fewer treatment options compared to other types of breast cancer? And most importantly, what does this mean for you, your treatment, and your future?

In this article, we’ll answer those questions and more. Our goal is to equip you with knowledge, not just about what TNBC is, but about why it behaves the way it does. Understanding the science behind this aggressive subtype can empower you to make informed decisions about your treatment options, advocate for yourself, and find hope in the ongoing advances in research and therapy.
Triple-negative breast cancer is defined by its lack of estrogen receptors (ER), progesterone receptors (PR), and HER2 expression — making it resistant to common hormone therapies and HER2-targeted therapies. This makes TNBC particularly challenging, but it also makes it the focus of much exciting new research. While TNBC tends to be more aggressive and harder to treat, advances in immunotherapy, targeted therapy, and chemotherapy are improving the outlook for many patients.
In the following sections, we will explore what makes TNBC so aggressive, how it is diagnosed, what treatment options exist, and what the prognosis looks like for patients diagnosed with TNBC. We’ll also dive into the latest research, including the potential role of insulin resistance and SRC (a protein implicated in tumor growth) in driving TNBC’s aggressive behavior.
By the end of this article, you’ll have a clearer understanding of TNBC — not just as a diagnosis, but as part of a broader journey of treatment, hope, and resilience. Let’s begin with the basics: what exactly is triple-negative breast cancer?
Part 1: What Is Triple-Negative Breast Cancer?
Triple-negative breast cancer (TNBC) is a subtype of breast cancer that lacks three specific markers on its tumor cells: estrogen receptors (ER), progesterone receptors (PR), and human epidermal growth factor receptor 2 (HER2). These receptors are typically targeted in other forms of breast cancer to slow or stop tumor growth. Because TNBC doesn’t express any of these markers, it doesn’t respond to standard hormone therapies or HER2-targeted treatments like trastuzumab (Herceptin), which are used for other types of breast cancer.
This lack of receptors is why it’s called “triple-negative.” It’s a term used to describe a set of breast cancer cells that are biologically different from more common types, and unfortunately, this difference contributes to its more aggressive nature.
The Biology Behind Triple-Negative Breast Cancer
To understand why TNBC is more aggressive, we need to look at what makes it biologically distinct from other breast cancers. In most breast cancers, the tumor cells have estrogen or progesterone receptors, or they overexpress HER2. These receptors can be targeted with specific therapies — hormonal treatments like tamoxifen or HER2-targeted drugslike trastuzumab — which help slow down or stop the growth of the cancer cells.
However, because TNBC does not have these receptors, it doesn’t respond to hormone treatments or HER2 therapies. This leaves chemotherapy as the main treatment option, which works by targeting rapidly dividing cells. But chemotherapy isn’t always a perfect solution, and TNBC can develop resistance, making it harder to treat over time.
Why Is TNBC So Aggressive?
Triple-negative breast cancer is often considered one of the most aggressive forms of breast cancer. But what does that really mean?
- Fast Growth: TNBC tumors tend to grow more quickly than other types of breast cancer. The rapid rate of cell division makes it more likely for the tumor to spread to other parts of the body (metastasize), particularly to organs like the lungs, liver, or brain.
- Higher Likelihood of Recurrence: Compared to other types of breast cancer, TNBC has a higher likelihood of recurrence, particularly in the first few years after treatment. This is because the aggressive nature of the cancer means that some microscopic cancer cells may escape treatment and later cause the cancer to come back.
- Metastasis: TNBC has a higher propensity to spread early. The absence of estrogen, progesterone, and HER2 receptors means that TNBC tumors don’t have the biological “brakes” that other cancers might have, allowing them to metastasize to other parts of the body more easily.
Risk Factors for TNBC
While we still don’t fully understand why some people develop TNBC, several risk factors may increase the likelihood of this type of breast cancer:
- Age: TNBC is more common in younger women, especially those under 40. This makes it more common in women who are premenopausal, though it can occur at any age.
- Family History: Women with a family history of breast cancer, particularly those with mutations in the BRCA1 gene, are at higher risk of developing TNBC. BRCA1 is a tumor suppressor gene, and mutations in this gene are linked to an increased risk of several cancers, including breast cancer. TNBC is more commonly seen in women with BRCA1 mutations compared to other genetic mutations.
- Ethnicity: TNBC is more common in African American women and women of Hispanic descent compared to white women. This difference might be related to genetic factors, though research is still ongoing to better understand the exact causes.
How TNBC Is Diagnosed
Like other breast cancers, TNBC is typically diagnosed through a combination of mammography, ultrasound, and biopsy. When a suspicious area is found in a mammogram or ultrasound, a biopsy is performed to confirm the diagnosis and determine whether the cancer is triple-negative. During the biopsy, the tumor cells are tested for the presence of estrogen, progesterone, and HER2 receptors.
In addition to these tests, genetic tests may be performed to assess whether a patient has a mutation in the BRCA1 gene or other genetic markers that might indicate an increased risk for TNBC.
Understanding whether a tumor is triple-negative is vital because it significantly influences the treatment plan. In the next section, we’ll explore why TNBC is so aggressive in more detail, diving into the biological and molecular mechanismsthat contribute to its behavior.
Part 2: Why Is Triple-Negative Breast Cancer So Aggressive?
Triple-negative breast cancer (TNBC) is known for its aggressive nature, and understanding why it behaves this way requires a look at its biological and molecular mechanisms.
TNBC doesn’t behave like other types of breast cancer, mainly because it lacks the estrogen and progesterone receptors (ER and PR) and the HER2 receptor that are typically present in breast cancer cells. This absence means that TNBC doesn’t respond to the standard treatments used for hormone receptor-positive or HER2-positive cancers. Instead, TNBC must rely on other pathways, many of which contribute to its aggressiveness.
1. Lack of Targeted Treatment Options
In most breast cancers, tumors that are hormone receptor-positive (ER or PR) or HER2-positive can be treated with targeted therapies. Hormone receptor-positive cancers can be treated with drugs that block estrogen or progesterone (like tamoxifen or aromatase inhibitors), while HER2-positive cancers can be treated with drugs that target the HER2 protein (like trastuzumab or pertuzumab). These treatments help stop the cancer cells from growing and dividing by blocking the signals that fuel their growth.
However, in TNBC, these targeted therapies aren’t effective because the cancer cells don’t have the receptors that these drugs work on. As a result, the treatment plan is primarily limited to chemotherapy, which aims to kill rapidly dividing cells — a strategy that isn’t as specific or precise as hormone therapy or HER2-targeted therapy.
While chemotherapy is still the most effective treatment for TNBC, it comes with significant risks, including side effects like hair loss, nausea, and increased susceptibility to infections. And because chemotherapy is a blunt tool, it doesn’t always target the cancer cells as efficiently as targeted therapies, which can lead to resistance over time.
2. High Proliferation Rate and Rapid Growth
One of the defining characteristics of TNBC is its high proliferation rate. This means the cancer cells are dividing rapidly. Ki-67, a marker for cell division, is typically higher in TNBC compared to other breast cancer subtypes, signaling that the tumor is growing and multiplying more quickly. The rapid division of cells means that the cancer has a higher chance of metastasizing — or spreading to other parts of the body — particularly to organs like the lungs, liver, or brain.
The increased proliferation also makes the tumor more likely to be resistant to therapies that target slowly dividing cells, such as hormone therapy. Chemotherapy is often the only available option for treatment, but even chemotherapy can have limited effectiveness against tumors that evolve quickly and develop resistance.
3. Genetic Mutations: The Role of p53 and BRCA1
In TNBC, genetic mutations are often at play, which contribute to its aggressive behavior. One of the most commonly found mutations in TNBC is in the p53 gene, which is a tumor suppressor gene. The p53 protein is responsible for preventing cells with damaged DNA from dividing. When p53 is mutated, damaged cells are allowed to continue dividing, often leading to the development of tumors. This mutation is found in many cancers, but it’s especially prevalent in TNBC. Because the p53 mutation allows cells to bypass growth checkpoints, it accelerates the cancer’s ability to spread and resist treatment.
Additionally, TNBC is strongly associated with BRCA1 mutations, which are linked to hereditary breast and ovarian cancers. BRCA1 is another tumor suppressor gene that helps repair damaged DNA. When this gene is mutated, cells accumulate DNA damage, increasing the likelihood of cancer. Patients with BRCA1 mutations are more likely to develop TNBC, and this specific type of cancer is often more aggressive in those with the mutation. PARP inhibitors, which target DNA repair mechanisms, are being researched as potential treatments for TNBC, especially in BRCA1-mutated cases.
4. Overexpression of SRC (Proto-Oncogene)
Another key factor contributing to TNBC’s aggressiveness is the overexpression of SRC, a protein that acts as a tyrosine kinase. SRC plays a pivotal role in cell signaling pathways that regulate cell growth, migration, and survival. In TNBC, SRC is often overexpressed or hyperactivated, which drives the cancer cells to grow uncontrollably and metastasize more easily.
SRC works by interacting with other signaling pathways involved in cell survival and proliferation. It plays a particularly crucial role in promoting tumor invasion and metastasis. Overactivation of SRC enhances the cancer’s ability to invade surrounding tissues, spread to distant organs, and resist apoptosis (programmed cell death). The presence of SRC in TNBC provides a potential target for therapies aimed at inhibiting SRC, though this is still in early stages of research.
5. Insulin and Metabolic Pathways
Recent research has started to explore the connection between insulin resistance and TNBC. Insulin resistance, which is often seen in individuals with diabetes, has been linked to an increased risk of TNBC. Insulin is a growth factor that can stimulate cell division, and high levels of insulin may contribute to the rapid growth of cancer cells, including those in TNBC. Furthermore, insulin resistance can activate other signaling pathways that promote tumor progression and metastasis, making TNBC more difficult to treat.
In addition to insulin, metabolic reprogramming in TNBC is also becoming a focal point of research. Tumor cells often alter their metabolism to fuel their rapid growth, a phenomenon known as the Warburg effect. TNBC cells, like other aggressive cancers, shift their energy production pathways to prioritize survival and proliferation. Understanding how TNBC manipulates its metabolism opens up new therapeutic avenues, such as targeting metabolic pathways to slow tumor growth.
6. The Tumor Microenvironment
Finally, the tumor microenvironment plays a major role in TNBC’s aggressive behavior. Unlike many other breast cancer subtypes, TNBC tends to be poorly differentiated, meaning that it doesn’t resemble normal breast tissue. This lack of differentiation makes it harder for the immune system to recognize and fight the tumor. Moreover, TNBC often recruits immune cells that may help the tumor survive rather than attack it, contributing to the cancer’s ability to grow and spread.
Additionally, the extracellular matrix, the network of proteins surrounding the tumor, often becomes more fibrotic and stiff in TNBC, which allows the cancer cells to invade surrounding tissues more easily. The interaction between cancer cells and their microenvironment not only helps the tumor grow but also increases its ability to evade therapies.
Understanding the Aggression
TNBC’s aggressiveness stems from a combination of genetic mutations, altered signaling pathways, immune evasion, and metabolic reprogramming. These factors work together to create a cancer that grows rapidly, spreads early, and resists many common treatments. However, this complexity also opens up new opportunities for targeted therapies and treatments that aim to disrupt these aggressive behaviors. With continued research and advances in immunotherapy and targeted treatment, the future for TNBC patients is becoming brighter, despite the challenges this cancer subtype presents.
In the next section, we’ll explore how TNBC is diagnosed and what tools doctors use to get a clear picture of the cancer’s extent and characteristics.
Part 3: How Triple-Negative Breast Cancer Is Diagnosed
Diagnosing triple-negative breast cancer (TNBC) involves the same basic steps as diagnosing any other type of breast cancer, but the specifics of TNBC require a more detailed and often more complex evaluation.
Given that TNBC doesn’t have the estrogen receptors (ER), progesterone receptors (PR), or HER2 expression, its diagnosis depends on a careful combination of imaging tests, biopsy procedures, and molecular testing. Understanding how TNBC is diagnosed is important, as it helps doctors determine the best course of treatment and provides patients with insight into what to expect at each stage.
1. Imaging Tests: Mammograms, Ultrasound, and MRI
The diagnostic process for TNBC begins with imaging tests, which are used to detect any abnormal masses in the breast. The mammogram is typically the first line of screening for women who are regularly monitored for breast cancer. If a suspicious mass is seen on the mammogram, doctors will often follow up with an ultrasound, which helps determine whether the mass is solid or fluid-filled, distinguishing a potential tumor from a cyst.
For women who have dense breast tissue or in cases where the mammogram is inconclusive, magnetic resonance imaging (MRI) may be used. MRI provides a more detailed view of breast tissue and is particularly useful in identifying smaller tumors or abnormalities that might be missed on a standard mammogram. However, MRI is more expensive and typically reserved for certain cases, such as women with a higher risk of breast cancer or those with dense breasts.
While these imaging tests are excellent at identifying tumors, they don’t provide the full picture. This is where biopsy and molecular testing come in.
2. Biopsy: The Core of Diagnosis
Once an abnormality is seen on imaging, the next step is usually a biopsy — a procedure where a small sample of tissue is removed from the suspicious area and examined under a microscope. Biopsy is the only way to confirm whether a mass is cancerous and to determine the type of cancer present.
In the case of TNBC, the biopsy is also essential for determining the hormone receptor status (estrogen and progesterone receptors) and the HER2 status. Since TNBC lacks these receptors, it will show negative results for all three markers — ER, PR, and HER2 — confirming that it is triple-negative.
The biopsy may also be followed by additional tests to assess the grade of the tumor, which indicates how aggressive the cancer cells are. Grade 1 tumors tend to be slower growing, while Grade 3 tumors are more aggressive and may require more intensive treatment. High-grade tumors are common in TNBC, contributing to its overall aggressive nature.
3. Molecular and Genetic Testing
In addition to determining the hormone receptor and HER2 status, molecular and genetic testing is an important part of the diagnostic process for TNBC. Understanding the genetic makeup of the tumor can give doctors crucial insights into the cancer’s behavior and help inform treatment decisions.
BRCA1 and BRCA2 Mutations
One of the most significant genetic factors in TNBC is the BRCA1 mutation, which is often linked to hereditary breast cancer. Women who carry a BRCA1 gene mutation have a higher risk of developing TNBC. If a TNBC patient tests positive for a BRCA1 mutation, they may be eligible for treatments like PARP inhibitors, which block a DNA repair pathway that is particularly vulnerable in cancer cells with BRCA1 mutations. Genetic counseling is often recommended for women with a family history of breast cancer or those diagnosed with TNBC at a young age.
Oncotype DX and MammaPrint
For patients diagnosed with TNBC, the use of multigene assays such as Oncotype DX and MammaPrint can be particularly valuable. These tests analyze a tumor’s gene expression to assess the likelihood of recurrence and to help guide decisions about whether chemotherapy will be beneficial. Although these tests are often more commonly used in hormone receptor-positive or HER2-positive cancers, they can still provide valuable information in TNBC cases, especially to determine the aggressiveness of the disease and help decide whether chemotherapy should be administered.
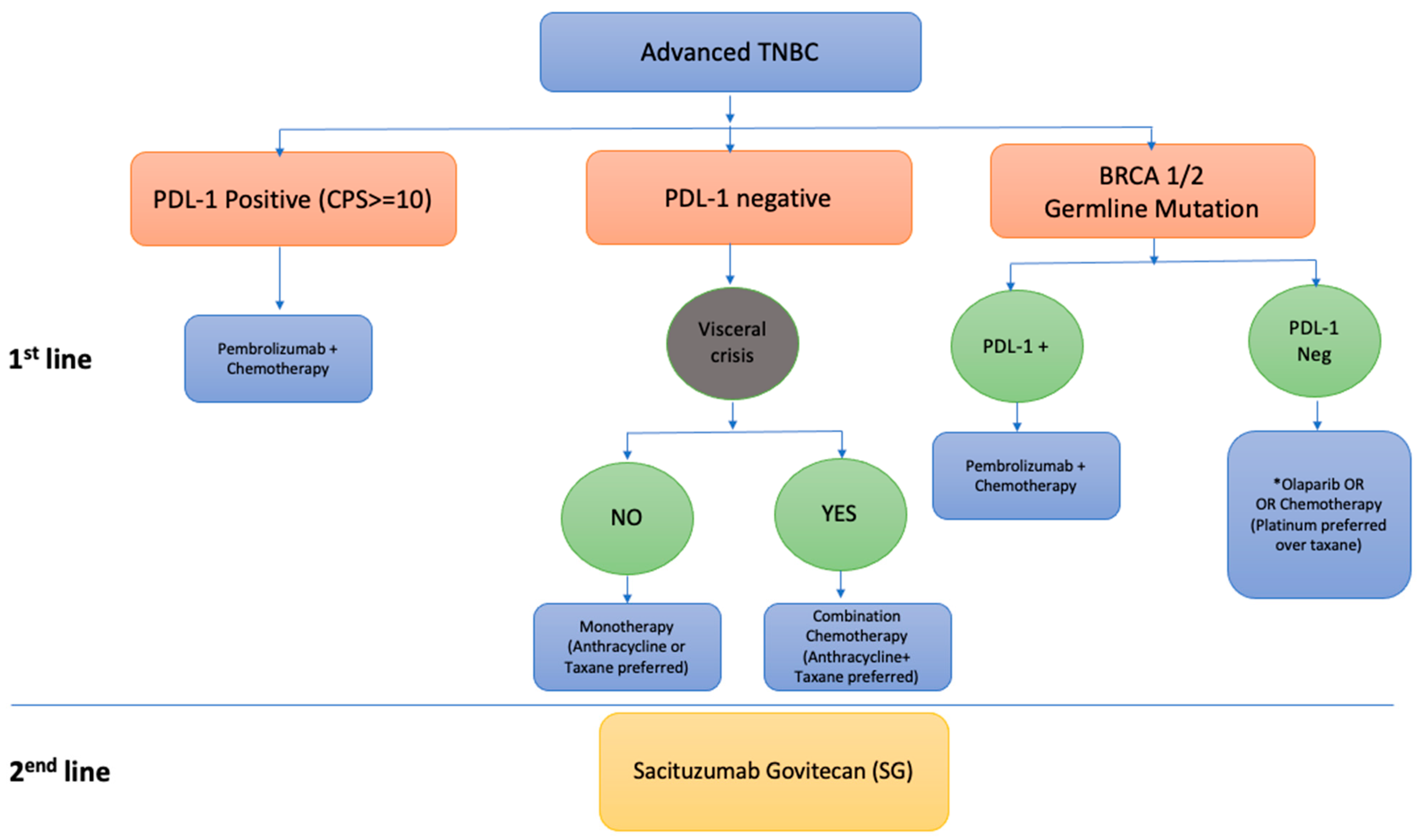
PD-L1 Testing
Immunotherapy has shown promise in treating TNBC, especially in cases where the cancer cells express programmed death-ligand 1 (PD-L1). PD-L1 is a protein that helps cancer cells evade detection by the immune system. By testing for PD-L1, doctors can determine if immunotherapy drugs like pembrolizumab (Keytruda) or atezolizumab (Tecentriq), which block the PD-1/PD-L1 pathway, might be effective for a given patient.
4. Staging: Understanding the Extent of the Cancer
Once TNBC is diagnosed, doctors must determine its stage — or how far the cancer has spread. This staging process involves additional imaging tests, such as CT scans, bone scans, or PET scans, which can help assess whether the cancer has spread to distant organs, such as the lungs, liver, or bones.
Staging is crucial for understanding the extent of disease and for determining an appropriate treatment plan. In Stage 0 or Stage I, the tumor is confined to the breast or lymph nodes and is more likely to be treated effectively with surgery and chemotherapy. In more advanced stages (Stage II, III, or IV), the cancer may have spread to other parts of the body, which may require a combination of chemotherapy, surgery, radiation, and possibly immunotherapy or targeted therapies.
The Road to Diagnosis
The diagnosis of triple-negative breast cancer is a detailed process that begins with imaging and culminates in a biopsy and molecular testing. While TNBC’s lack of receptors makes it more difficult to treat, it also opens the door for new research and targeted therapies that are improving outcomes for patients. Understanding the diagnostic process gives patients insight into how their doctors are evaluating the cancer and making treatment decisions.
In the next section, we’ll explore how TNBC is treated, what options are available, and how patients can manage the unique challenges of this aggressive breast cancer subtype.
Part 4: Treatment Options for Triple-Negative Breast Cancer
Triple-negative breast cancer (TNBC) is notorious for being harder to treat than other breast cancer subtypes. Because TNBC lacks the estrogen receptors (ER), progesterone receptors (PR), and HER2 expression, it doesn’t respond to hormonal therapies or HER2-targeted treatments. This leaves chemotherapy as the cornerstone of treatment. However, the approach to managing TNBC has evolved significantly in recent years, with new treatments like immunotherapy, targeted therapies, and clinical trials offering hope for better outcomes.

In this section, we’ll discuss the current treatment options for TNBC, focusing on chemotherapy, the promising role of immunotherapy, and the emerging therapies that are offering patients more targeted approaches.
1. Chemotherapy: The Mainstay of Treatment
Chemotherapy has traditionally been the primary treatment for triple-negative breast cancer, particularly because TNBC tends to be highly proliferative (cells are dividing rapidly). Chemotherapy works by targeting these rapidly dividing cells, attempting to slow their growth or kill them outright. However, while chemotherapy is often effective, it’s a blunt instrument that affects both cancerous and healthy cells, leading to common side effects like hair loss, fatigue, and nausea.
For early-stage TNBC (Stage I and II), chemotherapy is typically given adjuvantly (after surgery) to reduce the risk of recurrence. For more advanced stages, chemotherapy may be used both as a neoadjuvant (before surgery) and adjuvanttreatment to shrink tumors and target any cancer cells that may have spread to other parts of the body.
Common chemotherapy drugs used for TNBC include:
- Doxorubicin (Adriamycin)
- Cyclophosphamide (Cytoxan)
- Paclitaxel (Taxol)
- Carboplatin
These drugs can be combined in various regimens, with the goal of attacking cancer cells through different mechanisms. While chemotherapy remains effective for many patients with TNBC, the major challenge is chemoresistance. Over time, cancer cells can develop resistance to chemotherapy, causing treatment to lose its effectiveness. This is one of the reasons why recurrence rates for TNBC tend to be higher, especially in the first few years after initial treatment.
2. Immunotherapy: A Promising New Approach
In recent years, immunotherapy has emerged as a groundbreaking treatment option for triple-negative breast cancer, particularly for those patients whose tumors express high levels of PD-L1 (a protein that helps the tumor evade the immune system).
Immunotherapy works by boosting the body’s immune system to recognize and attack cancer cells. One of the most significant advancements in TNBC treatment has been the approval of PD-1/PD-L1 inhibitors, which block the PD-L1 protein on tumor cells, allowing the immune system to better target and destroy them.
- Pembrolizumab (Keytruda) is a PD-1 inhibitor that has shown significant promise in treating TNBC, particularly for patients with PD-L1-positive tumors. Pembrolizumab has been shown to increase overall survival in patients with advanced or metastatic TNBC.
- Atezolizumab (Tecentriq) is another PD-L1 inhibitor that has shown positive results, especially when combined with chemotherapy. This combination has been approved for use in metastatic TNBC and has demonstrated the ability to extend survival and improve response rates in patients with advanced TNBC.
Immunotherapy is particularly beneficial for patients with metastatic TNBC or for those whose tumors have progressed after traditional chemotherapy. It’s also being explored in clinical trials for early-stage TNBC, with the hope of improving treatment outcomes and reducing recurrence rates.
3. Targeted Therapy: Future Directions
While TNBC doesn’t have the typical receptors that other therapies target, targeted therapies are beginning to play an important role in treatment. Targeted therapies work by focusing on specific molecules or pathways that are involved in cancer growth.
For example:
- PARP inhibitors: Drugs like olaparib (Lynparza) are being studied as targeted therapies for TNBC, particularly in patients with a BRCA1 or BRCA2 mutation. These drugs work by blocking the repair of DNA damage in cancer cells, leading to cell death. Because BRCA1 and BRCA2 are involved in DNA repair, cancers with mutations in these genes are particularly vulnerable to PARP inhibition.
- Antibody-drug conjugates (ADCs): This newer class of drugs involves antibodies that target specific proteins on the cancer cells, delivering a cytotoxic drug directly to the tumor. The goal is to limit the damage to healthy cells while effectively killing the cancer cells. Research into ADCs for TNBC is ongoing, with promising results in clinical trials.
- Src inhibitors: As we discussed in Part 2, SRC is often overexpressed in TNBC and contributes to cancer cell growth and metastasis. Inhibiting SRC may block the signals that allow the cancer to grow and spread. While still in clinical trial stages, SRC inhibitors represent an exciting potential treatment for TNBC.
4. Clinical Trials: A Path to Better Treatments
Since TNBC is so difficult to treat, clinical trials are a crucial avenue for finding better treatments and ultimately a cure. Clinical trials often give patients access to the latest therapies, including immunotherapy, targeted therapies, and novel chemotherapy regimens that aren’t yet widely available.
Participating in a clinical trial can be a way to receive cutting-edge treatment while contributing to the broader research community’s understanding of TNBC. Patients interested in clinical trials should consult with their oncologist to determine if they are eligible and to understand the potential risks and benefits.
Triple-negative breast cancer is aggressive, but the treatment landscape is evolving. While chemotherapy remains the cornerstone of treatment, immunotherapy and targeted therapies are beginning to offer new hope for patients. Research into the genetic and molecular underpinnings of TNBC continues, and with each new discovery, more treatment options are becoming available.
Although TNBC remains one of the more challenging types of breast cancer to treat, personalized treatment — based on genetic testing, tumor profiling, and immunotherapy responses — is offering patients more options than ever before. The future for TNBC treatment is moving in a hopeful direction, and clinical trials, research, and new therapies are at the forefront of improving survival and quality of life for those diagnosed with this challenging cancer.
In the next section, we’ll explore the prognosis for patients with TNBC, including survival rates and the factors that influence long-term outcomes.
Part 5: Prognosis and Survival Rates
One of the most difficult aspects of a triple-negative breast cancer (TNBC) diagnosis is the uncertainty about what comes next. Unlike hormone receptor-positive or HER2-positive breast cancers, TNBC often has a more aggressive course and a higher risk of recurrence. Understanding the prognosis — how the cancer is likely to behave — is crucial in helping patients and their healthcare teams make decisions about treatment and long-term management.
While statistics provide a broad sense of survival and recurrence rates, it’s important to remember that each patient’s situation is unique. Prognosis depends on a number of factors, including the tumor’s characteristics, the stage of the cancer, how well the cancer responds to initial treatments, and the patient’s overall health.
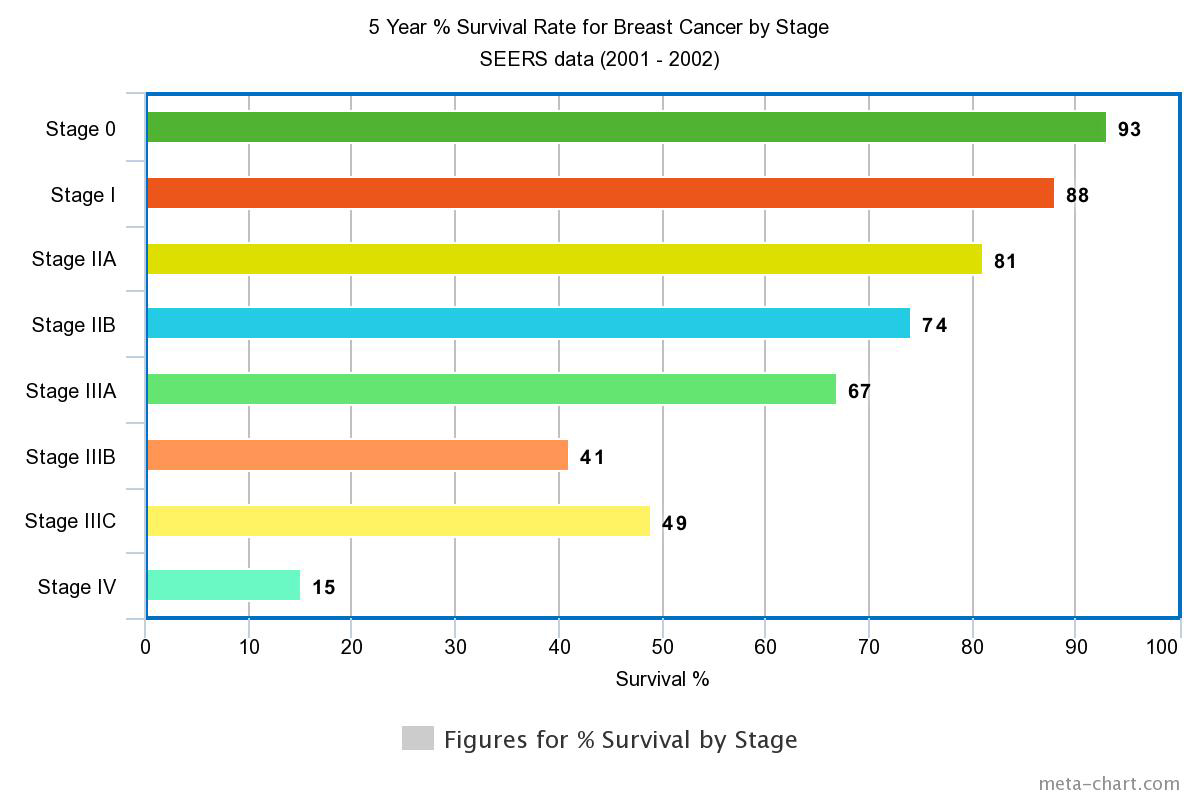
1. Survival Rates for Triple-Negative Breast Cancer
Survival rates for TNBC tend to be lower than for other subtypes of breast cancer. This is largely due to its aggressive nature, tendency to spread quickly, and resistance to standard therapies like hormone therapy and HER2-targeted treatments. However, survival rates have been improving with advancements in treatment, including the use of immunotherapy, targeted therapies, and more personalized treatment approaches.
Early-Stage TNBC
For early-stage TNBC (Stage 1 or Stage 2), the 5-year survival rate can be relatively favorable, but it’s still lower compared to other types of breast cancer. The 5-year survival rate for Stage 1 TNBC is generally around 70% to 90%, depending on the specific tumor characteristics, like grade, size, and response to chemotherapy. However, TNBC’s risk of recurrence is higher in the first few years after treatment, making follow-up care critical.
For Stage 2 TNBC, the survival rate can range from 50% to 70%, again depending on how the tumor responds to chemotherapy and how much the cancer has spread to nearby lymph nodes or tissues. This range reflects the variability of response to treatment and the level of aggressiveness in individual tumors.
Advanced-Stage TNBC
In Stage 3 or Stage 4 TNBC, the survival rate drops significantly, especially for metastatic TNBC, which has spread to distant organs like the lungs, liver, or brain. The 5-year survival rate for metastatic TNBC is typically 12% to 25%, although this varies based on factors like the specific sites of metastasis, overall health, and how well the cancer responds to therapies like chemotherapy and immunotherapy.
Metastatic TNBC remains difficult to treat, but advances in immunotherapy and clinical trials are improving the outlook for some patients. Clinical trials are essential for patients with advanced TNBC because they provide access to new therapies that might offer longer survival times or improved quality of life.
2. Factors Influencing Prognosis in TNBC
Several factors influence how well a person will respond to treatment and their overall prognosis with TNBC. These include:
Tumor Size and Stage
The size of the tumor and the extent of spread (whether cancer has spread to nearby lymph nodes or other organs) play a significant role in survival. Smaller tumors that are caught early generally have a better prognosis than larger tumors or those that have spread to lymph nodes or distant organs.
Tumor Grade
Tumor grade refers to how abnormal the cancer cells look under the microscope. TNBC is often high-grade, meaning the cancer cells appear more irregular and divide more rapidly. High-grade tumors are more likely to grow and spread quickly, which typically correlates with a poorer prognosis. Conversely, lower-grade tumors tend to be less aggressive and may respond better to treatment.
Response to Treatment
How well a TNBC tumor responds to chemotherapy or immunotherapy is a key factor in prognosis. Some tumors shrink significantly with chemotherapy and remain in remission for years, while others can develop resistance to treatment and recur. The emergence of immunotherapies has brought hope to many patients with metastatic TNBC, but the overall response to these treatments still varies widely.
Genetic Factors and Mutations
Certain genetic mutations, like BRCA1 or BRCA2, can influence the prognosis for TNBC. Patients with TNBC who carry BRCA1 mutations tend to have more aggressive disease, but they may also respond well to PARP inhibitors, which are a newer class of drugs that target DNA repair in tumor cells. These treatments are still being tested in clinical trials, but they represent a growing area of hope for patients with genetic mutations linked to TNBC.
Patients with BRCA2 mutations may also have a higher risk of developing TNBC and may benefit from treatment strategies that target DNA repair pathways, including chemotherapy and PARP inhibitors.
Age and Overall Health
Younger patients, especially those under 40, are more likely to develop TNBC, but their prognosis can vary based on overall health and how well they tolerate treatments. Older patients may face more challenges with aggressive treatments like chemotherapy and may have a higher risk of complications from treatment. Pre-existing health conditions like heart disease or diabetes can also complicate treatment decisions and impact overall prognosis.
3. Advancements in Treatment and Prognosis
Thanks to advances in treatment, the prognosis for TNBC is improving, especially for patients diagnosed in the early stages. Immunotherapy, targeted therapies, and the development of personalized medicine are beginning to make a tangible impact on survival rates and quality of life. New treatments, including PARP inhibitors and immune checkpoint inhibitors, have extended survival for some patients with metastatic TNBC, even in cases where chemotherapy has failed.
Additionally, clinical trials are a key part of improving outcomes for TNBC patients. By participating in clinical trials, patients can gain access to cutting-edge treatments that might otherwise be unavailable. These trials are essential for finding better therapies and ultimately improving the prognosis for people with TNBC.
4. Survivorship and Quality of Life
While survival rates are a crucial part of prognosis, the quality of life is equally important. Many patients with TNBC face long-term side effects from chemotherapy, such as fatigue, neuropathy, and cognitive issues, which can impact their daily lives. As treatments improve, supportive care — including physical therapy, psychological counseling, and nutritional support — has become an essential part of TNBC management, helping patients live better lives during and after treatment.
The prognosis for triple-negative breast cancer can be daunting, but it’s important to remember that survival rates are improving thanks to new treatments, better understanding of the disease, and ongoing research. Advances in immunotherapy, targeted therapies, and genetic testing are beginning to give hope to patients diagnosed with this aggressive subtype of breast cancer. While TNBC remains one of the more difficult types of breast cancer to treat, patients today have more options than ever before, and survival rates are steadily improving.
As we continue to learn more about TNBC, especially through clinical trials and research, the future holds promise for better treatments, better outcomes, and ultimately, a brighter outlook for those diagnosed with TNBC.
In the next section, we’ll answer some of the frequently asked questions that patients and families often have about TNBC, offering further clarity on living with and managing this challenging cancer.
Part 6: FAQs About Triple-Negative Breast Cancer
Triple-negative breast cancer (TNBC) can be difficult to understand, and many patients and their families have questions about what it means, how it’s treated, and what they can expect moving forward. Here, we’ll address some of the most common questions people ask about TNBC, offering clear and actionable information.
Why is triple-negative breast cancer more likely to recur?
TNBC is more aggressive than other types of breast cancer, which makes it more likely to recur. Tumors grow quickly and are more likely to spread to other organs (metastasize). Because TNBC doesn’t respond to hormone therapy or HER2-targeted treatments, it lacks the additional support that other types of breast cancer have. As a result, the risk of recurrence is higher in the first few years following treatment, especially if the cancer was not completely eradicated by chemotherapy.
Can lifestyle changes help reduce the risk of TNBC?
While there is no surefire way to prevent TNBC, some lifestyle changes may help lower the risk of developing breast cancer in general. These include:
- Maintaining a healthy weight: Obesity, particularly after menopause, is linked to an increased risk of breast cancer.
- Regular exercise: Physical activity has been shown to reduce breast cancer risk, likely by balancing hormones and improving immune function.
- Limiting alcohol consumption: Studies show a link between alcohol use and an increased risk of breast cancer.
- Dietary changes: A diet rich in fruits, vegetables, and whole grains, with limited processed foods and red meats, may be beneficial for overall health and cancer prevention.
Though these changes won’t guarantee prevention, they can contribute to overall well-being and may lower the risk of developing not just breast cancer, but many other types of cancer.
What are the genetic factors involved in TNBC?
Genetic mutations play a significant role in the development of TNBC. The BRCA1 gene mutation is particularly associated with TNBC. Women with this mutation have a significantly higher risk of developing TNBC. Other genetic mutations, like those in the BRCA2 gene, can also increase the risk. Testing for these mutations, especially in patients with a family history of breast cancer, can help guide treatment decisions. For example, PARP inhibitors, which are targeted therapies that block a DNA repair mechanism, have shown promise in treating TNBC, particularly in patients with BRCA1 or BRCA2 mutations.
Is TNBC more common in younger women?
Yes, TNBC tends to be more common in younger women, particularly those under 40. It is also more frequently diagnosed in African American and Hispanic women. While TNBC can occur at any age, it is particularly aggressive in younger women and tends to present with high-grade tumors that grow and spread quickly. The reasons behind these demographic disparities are still being researched, but they likely involve a combination of genetic, environmental, and hormonal factors.
How does insulin resistance play a role in TNBC?
Emerging research suggests that insulin resistance — a condition where the body’s cells don’t respond properly to insulin — may play a role in the development of TNBC. Insulin is a growth factor that helps cells divide, and high insulin levels may contribute to the rapid growth of TNBC cells. Insulin resistance is often seen in individuals with type 2 diabetes and obesity, both of which have been linked to an increased risk of TNBC. Studies are ongoing to explore how controlling insulin levels and improving insulin sensitivity might become part of the treatment strategy for TNBC.
Can triple-negative breast cancer be cured?
While TNBC is aggressive and more difficult to treat than other types of breast cancer, it is still treatable. In early-stage TNBC, where the cancer hasn’t spread beyond the breast or nearby lymph nodes, treatment with chemotherapy, surgery, and possibly radiation can be highly effective. The prognosis is more challenging for advanced-stage or metastatic TNBC, but new treatments like immunotherapy, PARP inhibitors, and targeted therapies are showing promise in improving survival rates. Cure is not always possible for metastatic TNBC, but ongoing advancements in treatments offer new hope, and many patients live for extended periods with the disease under control.
The questions around triple-negative breast cancer are numerous, and understandably so. The lack of targeted treatments, combined with the aggressive nature of the disease, makes TNBC a particularly challenging diagnosis. However, the key takeaway is that research is rapidly advancing, and treatment options are expanding. Immunotherapy, targeted therapies, and clinical trials are changing the landscape for TNBC patients, offering hope where there was once limited choice. Always discuss your treatment options with your oncologist, and don’t hesitate to ask about new therapies and clinical trial opportunities that might be available to you.
Part 7: Final Thoughts
Triple-negative breast cancer (TNBC) can be one of the most challenging types of breast cancer to face. Its aggressive nature, lack of targeted treatment options, and higher risk of recurrence make it a daunting diagnosis for many. But while TNBC is a more difficult subtype to treat, it’s important to understand that the landscape of treatment is changing — and rapidly.
Advances in immunotherapy, targeted therapies, and personalized treatment have begun to offer new hope for patients with TNBC. Treatments that were once considered experimental are now becoming part of standard care, and clinical trials are constantly pushing the boundaries of what’s possible. The increasing focus on genetic testing and tumor profiling means that doctors can now tailor treatments to the unique characteristics of each patient’s cancer, improving outcomes and survival rates.
While TNBC remains more likely to recur than other types of breast cancer, early detection, effective chemotherapy, and emerging therapies have greatly improved the prognosis for many patients. The key to managing TNBC is a comprehensive approach that includes chemotherapy, targeted therapy, and, where appropriate, immunotherapy. And with ongoing research, new and even more effective treatments are on the horizon.
As a patient, it’s important to remember that while TNBC is aggressive, it doesn’t define you or your journey. It’s a part of your story, but it’s not the whole story. With the right treatment, support, and continued research, many people with TNBC go on to live long, fulfilling lives. The future of TNBC care is brighter than ever, and patients today have more options than ever before.
If you’re facing a TNBC diagnosis, take one step at a time. Work closely with your healthcare team, stay informed about the latest treatment options, and don’t hesitate to ask about clinical trials or new therapies. You’re not alone in this, and advancements in breast cancer treatment continue to offer more hope with each passing year.









