Understanding the TCHP Chemotherapy Regimen for HER2-Positive Breast Cancer
- Introduction to TCHP Chemotherapy
- Components of the TCHP Regimen
- Administration Protocol
- Efficacy and Outcomes
- Side Effects and Management Strategies
- Cardiac Monitoring During Treatment
- TCHP vs Other HER2-Positive Regimens
- Neoadjuvant vs Adjuvant Use of TCHP
- Pathological Complete Response and Its Prognostic Value
- Long-Term Follow-Up After TCHP
- Patient Experience During TCHP: Physical and Emotional Journey
- TCHP in Metastatic HER2-Positive Breast Cancer
- Considerations for Older Patients and Those with Comorbidities
- Managing Fertility and Reproductive Health
- Financial Toxicity and Access to TCHP
- Future Directions in HER2-Positive Breast Cancer Treatment
- Survivorship Planning After TCHP
- FAQ
Introduction to TCHP Chemotherapy
The TCHP regimen is a combination chemotherapy protocol specifically designed for patients with HER2-positive breast cancer. HER2-positive refers to breast cancers that overexpress the human epidermal growth factor receptor 2 (HER2), a protein that promotes the growth of cancer cells. Approximately 15-20% of breast cancers are HER2-positive, and they tend to be more aggressive than other types.
TCHP stands for the four drugs used in this regimen: Docetaxel (Taxotere), Carboplatin, Trastuzumab (Herceptin), and Pertuzumab (Perjeta). This combination is utilized in both neoadjuvant (before surgery) and adjuvant (after surgery) settings to reduce tumor size, eliminate residual cancer cells, and improve overall survival rates.
The rationale behind combining these specific drugs lies in their synergistic effects. Docetaxel and Carboplatin are chemotherapeutic agents that disrupt cell division, while Trastuzumab and Pertuzumab are monoclonal antibodies targeting the HER2 receptor, thereby inhibiting cancer cell growth and survival.
Components of the TCHP Regimen
Each drug in the TCHP regimen plays a distinct role in combating HER2-positive breast cancer:
- Docetaxel (Taxotere): A taxane-based chemotherapy that stabilizes microtubules, preventing cell division and leading to cell death.
- Carboplatin: A platinum-based chemotherapeutic agent that causes DNA crosslinking, inhibiting DNA replication and transcription, ultimately inducing apoptosis in cancer cells.
- Trastuzumab (Herceptin): A monoclonal antibody that binds to the HER2 receptor, blocking downstream signaling pathways responsible for cell proliferation and survival. It also mediates antibody-dependent cellular cytotoxicity.
- Pertuzumab (Perjeta): Another monoclonal antibody that binds to a different epitope on the HER2 receptor, preventing dimerization with other HER receptors, thereby inhibiting cell signaling and growth.
The combination of Trastuzumab and Pertuzumab provides a more comprehensive blockade of the HER2 signaling pathway, enhancing the efficacy of the treatment.

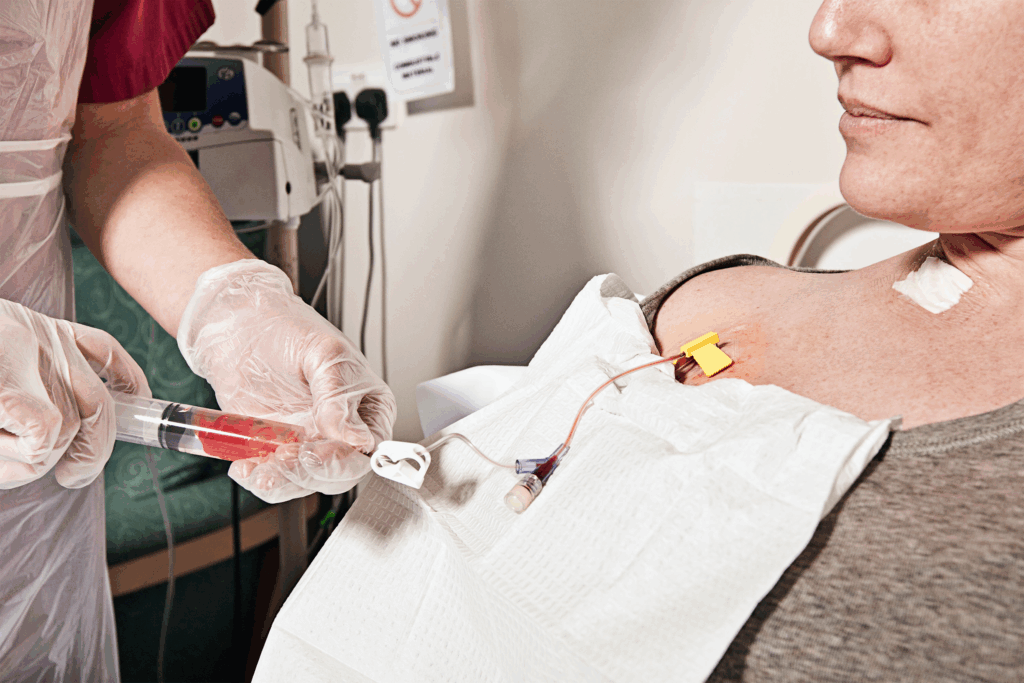
Administration Protocol
The TCHP regimen is typically administered in cycles, with each cycle lasting 21 days. Patients usually undergo six cycles, totaling approximately 18 weeks of treatment. The administration schedule is as follows:
- Day 1 of Each Cycle:
- Docetaxel: Administered intravenously over 60 minutes.
- Carboplatin: Administered intravenously over 30 minutes.
- Trastuzumab: Initial dose administered intravenously over 90 minutes; subsequent doses over 30 minutes if well-tolerated.
- Pertuzumab: Initial dose administered intravenously over 60 minutes; subsequent doses over 30-60 minutes.
Following the completion of the six cycles, Trastuzumab and Pertuzumab may be continued every three weeks to complete a total of one year of HER2-targeted therapy. This maintenance phase is crucial for sustaining the therapeutic effects and reducing the risk of recurrence.
Efficacy and Outcomes
Clinical trials and real-world studies have demonstrated the efficacy of the TCHP regimen in treating HER2-positive breast cancer. The combination of chemotherapy with dual HER2 blockade has been shown to increase the rate of pathological complete response (pCR), which is associated with improved long-term outcomes.
For instance, the TRYPHAENA trial reported high pCR rates with the TCHP regimen, indicating its effectiveness in eradicating cancer cells before surgery. Additionally, the regimen has been associated with improved event-free survival and overall survival rates compared to chemotherapy alone or single-agent HER2-targeted therapy.
It’s important to note that individual responses to treatment can vary based on factors such as tumor biology, patient health status, and adherence to the treatment protocol. Regular monitoring and follow-up are essential to assess treatment response and manage any adverse effects.
Side Effects and Management Strategies
The TCHP regimen, while highly effective, is associated with a range of side effects that vary in severity from patient to patient. Common side effects include fatigue, nausea, diarrhea, hair loss, and neutropenia. Many of these effects are predictable and can be managed with preemptive and supportive care.
Neutropenia, or low white blood cell count, is one of the most frequent and serious side effects. To reduce infection risk, patients may receive growth factor support such as filgrastim or pegfilgrastim. Nausea and vomiting are managed with antiemetic drugs like ondansetron or dexamethasone, administered before and after infusion.
Peripheral neuropathy is another concern, particularly due to docetaxel. It presents as tingling or numbness in the hands and feet and may necessitate dose modification. Diarrhea, more commonly associated with pertuzumab, can be managed with loperamide and dietary adjustments. Early and honest communication between patients and providers is essential for tailoring side effect management.
Cardiac Monitoring During Treatment
Because Trastuzumab and Pertuzumab target HER2, which is also expressed in cardiac tissue, there is a known risk of cardiotoxicity. Cardiac dysfunction, including reduced left ventricular ejection fraction (LVEF) or congestive heart failure, may occur, especially when these drugs are used in combination or following anthracycline therapy.
Baseline cardiac evaluation using echocardiography or MUGA scans is performed before starting treatment. LVEF is reassessed every three months during the course of HER2-targeted therapy to monitor cardiac function. If a significant decline in LVEF is detected, HER2 therapy may be temporarily withheld or permanently discontinued depending on the severity and reversibility of the dysfunction.
Patients with preexisting cardiac conditions are monitored more closely, and in some cases, cardioprotective medications such as beta-blockers or ACE inhibitors may be considered. Cardiologic consultation is recommended when LVEF drops below safe thresholds. Ongoing research aims to refine risk prediction and prevention strategies for this critical side effect.
TCHP vs Other HER2-Positive Regimens
The TCHP regimen is often compared with other common HER2-positive treatment protocols, such as AC-TH (Adriamycin, Cyclophosphamide followed by Taxol and Herceptin) and THP (Taxol, Herceptin, Pertuzumab). While each regimen has its own merits, TCHP is distinguished by the absence of anthracyclines and the inclusion of dual HER2 blockade, which offers a potent anti-cancer strategy with reduced risk of cardiotoxicity associated with anthracyclines.
Here is a comparative overview:
| Regimen | HER2 Blockade | Chemotherapy Backbone | Cardiotoxicity Risk | Typical Use Case |
| TCHP | Trastuzumab + Pertuzumab | Docetaxel + Carboplatin | Moderate | High-risk HER2+, neoadjuvant/adjuvant |
| AC-TH | Trastuzumab | Doxorubicin + Cyclophosphamide, followed by Paclitaxel | High | Some HER2+ cases, higher recurrence risk |
| THP | Trastuzumab + Pertuzumab | Paclitaxel only | Low | Lower-risk HER2+, older or cardiac patients |
The decision between regimens depends on tumor stage, cardiac profile, and patient tolerance. Many oncologists favor TCHP in younger or high-risk patients where aggressive upfront control is necessary.
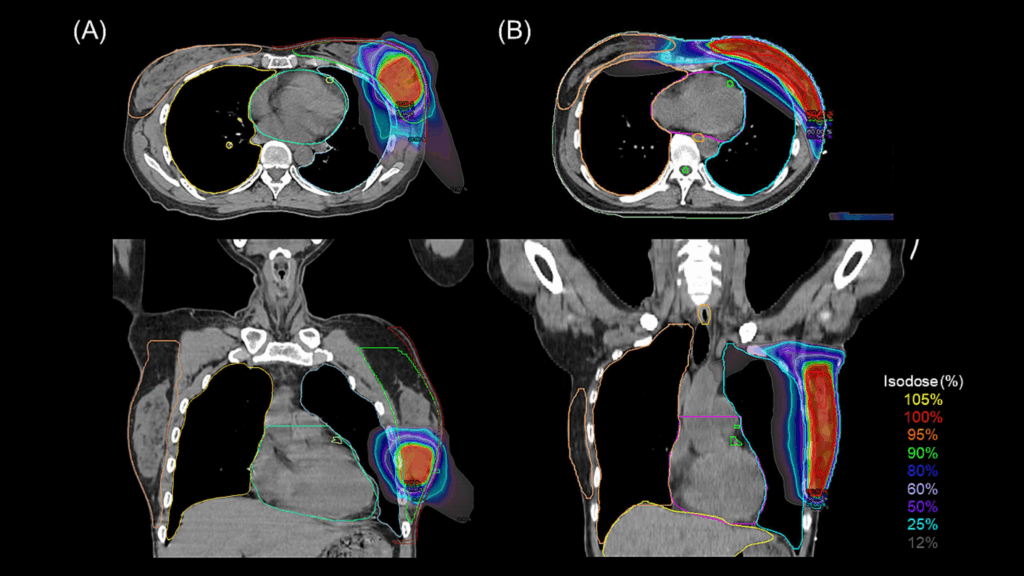
Neoadjuvant vs Adjuvant Use of TCHP
TCHP can be employed both as a neoadjuvant therapy (before surgery) and adjuvant therapy (after surgery), with strategic advantages in each setting. In the neoadjuvant setting, TCHP is used to shrink tumors, making breast-conserving surgery more feasible and allowing real-time assessment of the tumor’s responsiveness to treatment.
Achieving a pathological complete response (pCR) in the neoadjuvant phase is a strong predictor of improved survival, particularly in HER2-positive disease. For patients who do not achieve pCR, post-surgical treatment may be intensified or extended, such as incorporating T-DM1 (ado-trastuzumab emtansine).
In the adjuvant setting, TCHP is used to eliminate microscopic residual disease and reduce the likelihood of recurrence. While the therapeutic intent remains the same, the benefit of using TCHP before surgery lies in early tumor shrinkage, biomarker reevaluation, and potentially guiding more personalized post-operative therapy.
Pathological Complete Response and Its Prognostic Value
A key objective of using the TCHP regimen in the neoadjuvant setting is achieving a pathological complete response (pCR), defined as the absence of invasive cancer in the breast and lymph nodes at the time of surgery. pCR is not only a marker of treatment success but also a strong prognostic indicator in HER2-positive breast cancer.
Patients who achieve pCR after TCHP therapy typically have significantly improved event-free survival (EFS) and overall survival (OS) compared to those with residual disease. Clinical trials like NeoSphere and TRYPHAENA have shown pCR rates exceeding 50% in patients receiving TCHP, particularly in those with hormone receptor-negative tumors.
The ability to assess response before surgery allows oncologists to tailor adjuvant therapy more precisely. For example, patients who do not reach pCR may receive T-DM1 instead of continuing trastuzumab, a strategy supported by the KATHERINE trial. Thus, pCR not only reflects biological sensitivity but also guides downstream treatment decisions.
Long-Term Follow-Up After TCHP
After completion of the TCHP regimen, long-term follow-up is critical to monitor for recurrence, manage late side effects, and support survivorship. Most patients continue with HER2-targeted therapy until they complete a full year of trastuzumab-based treatment. Regular clinical evaluations, imaging as indicated, and blood work are part of ongoing care.
Cardiac function remains a major area of focus during follow-up, especially for patients who experienced transient drops in ejection fraction. Echocardiograms or MUGA scans are often continued every 6 to 12 months for the first two years post-treatment.
Other aspects of follow-up include bone health assessments (due to chemotherapy-induced menopause), fertility counseling, and screening for secondary malignancies. Survivorship care plans are typically developed by the oncology team and include guidance on diet, exercise, emotional support, and return-to-work planning. The goal is holistic recovery, not just disease control.
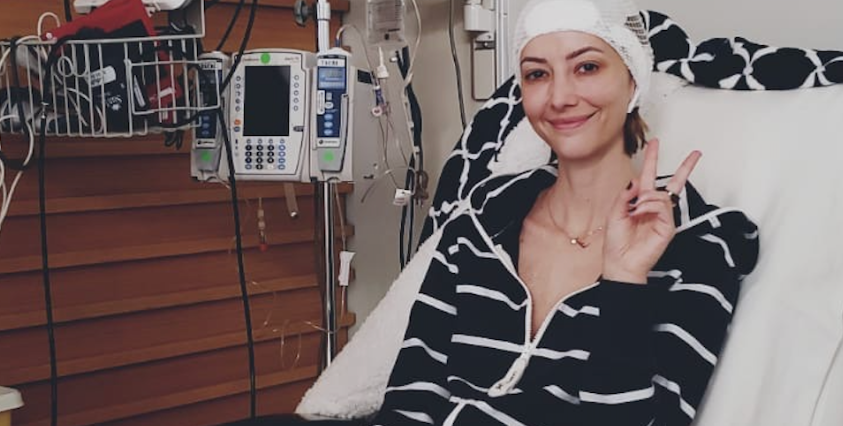
Patient Experience During TCHP: Physical and Emotional Journey
Going through the TCHP regimen is physically and emotionally taxing for most patients. The physical side effects, such as fatigue, hair loss, gastrointestinal issues, and altered taste, can be overwhelming. Many patients also experience anxiety, depression, and fear, especially around infusion days or when awaiting scan results.
Support systems are crucial. Oncology nurses, support groups, therapists, and patient navigators play a major role in helping patients adapt. Some find strength in mindfulness practices, gentle physical activity, or journaling their experience. It is not uncommon for patients to describe the treatment period as one of the most challenging yet transformative experiences of their lives.
Clear communication with the medical team and family helps reduce the sense of isolation and helplessness. While TCHP is an aggressive regimen, understanding what to expect and having a proactive support system in place often makes the journey more manageable and empowering.
TCHP in Metastatic HER2-Positive Breast Cancer
Although TCHP is primarily used in early-stage and locally advanced HER2-positive breast cancer, it may also play a role in selected cases of metastatic disease, especially when a strong initial response is needed. The regimen is considered when there is a significant tumor burden, rapid progression, or visceral crisis.
In metastatic settings, HER2-targeted therapies such as trastuzumab deruxtecan (Enhertu) or tucatinib-based combinations are more commonly used due to better tolerability in long-term treatment. However, TCHP may be used as a first-line intensive induction therapy to quickly control aggressive disease, followed by transition to maintenance regimens.
This approach requires careful evaluation of the patient’s functional status, organ reserve, and treatment goals. Quality of life considerations remain paramount, and treatment plans are adapted dynamically as disease behavior and patient needs evolve.
Considerations for Older Patients and Those with Comorbidities
Administering the TCHP regimen to elderly patients or those with underlying health conditions poses distinct challenges. Aging impacts drug metabolism, increases the risk of organ toxicity, and reduces physiological resilience. Before beginning therapy, comprehensive geriatric assessments are essential to evaluate functional status, comorbidities, cognitive function, nutritional state, and psychosocial factors. This allows oncologists to distinguish between fit and frail patients and to adjust the intensity of treatment accordingly.
Patients with cardiovascular disease, renal insufficiency, liver impairment, or diabetes require particular caution. HER2-targeted therapies like trastuzumab and pertuzumab can exacerbate cardiac issues, while chemotherapy agents may interact with existing medications. In such cases, dose modifications, extended infusion times, or alternative regimens like THP may be preferred to reduce toxicity.
Regular monitoring throughout treatment — including lab work, cardiac imaging, and symptom tracking — ensures early detection of complications. Multidisciplinary care teams that include cardiologists, geriatricians, pharmacists, and dietitians can greatly improve the safety and efficacy of TCHP in complex patients. The overall goal remains the same: to balance oncologic control with preservation of independence, function, and dignity.
Managing Fertility and Reproductive Health
Fertility preservation is a major concern for younger women undergoing TCHP chemotherapy, as the regimen carries a high risk of ovarian toxicity. Chemotherapy can impair ovarian reserve, disrupt hormonal cycles, and even lead to premature menopause. For patients wishing to preserve future reproductive potential, fertility counseling should be initiated as soon as possible after diagnosis and before the first cycle of treatment.
Cryopreservation of embryos or unfertilized eggs is the most established method. These procedures require 10–14 days of ovarian stimulation and retrieval, which is usually feasible without delaying treatment. Some patients may also consider ovarian tissue preservation, though this is less common. Concurrent use of GnRH agonists like goserelin may offer partial protection to the ovaries by inducing temporary suppression during chemotherapy, although it is not a guarantee of fertility preservation.
After completing treatment, hormone testing (e.g., AMH, FSH, estradiol) and consultation with a reproductive endocrinologist help assess post-treatment fertility status. Discussions about pregnancy timing, contraceptive needs, and menopause symptoms are also important, as many patients resume regular cycles without full fertility. This topic remains deeply personal and emotionally charged, and oncologists must address it with empathy and medical clarity.
Financial Toxicity and Access to TCHP
The TCHP regimen includes some of the most expensive cancer therapies available, particularly the biologics trastuzumab and pertuzumab. Even for insured patients, out-of-pocket costs can be overwhelming due to deductibles, co-pays, and associated medical expenses such as lab tests, imaging, medications for side effects, and transportation. For uninsured or underinsured individuals, access may be limited, creating health disparities that affect treatment outcomes.
Financial toxicity refers not only to the financial burden itself but also to the emotional and psychological stress it imposes on patients and their families. It may lead to skipped appointments, reduced adherence to medication schedules, or delayed follow-up care. To mitigate this, oncology centers typically provide access to financial counselors who can help identify co-pay assistance programs, pharmaceutical grants, nonprofit support, and sliding-scale services.
Open communication between healthcare providers and patients is critical. Oncologists should initiate conversations about cost early in the treatment planning process and remain responsive to changes in the patient’s financial situation. Advocacy for equitable cancer care also continues at the systemic level, aiming to reduce economic barriers and ensure that all eligible patients receive the full benefit of regimens like TCHP.
Future Directions in HER2-Positive Breast Cancer Treatment
While TCHP remains a cornerstone in the treatment of HER2-positive breast cancer, ongoing research is rapidly evolving the landscape. Scientists are working on refining patient stratification to better determine who truly needs intensive chemotherapy and who might benefit from de-escalated therapy with fewer side effects. Biomarkers such as PIK3CA mutations, tumor-infiltrating lymphocytes, and circulating tumor DNA are being explored to personalize therapy and predict response.
Emerging agents like trastuzumab deruxtecan (Enhertu) and tucatinib are demonstrating strong efficacy in metastatic settings and are being tested in earlier stages. Bispecific antibodies, antibody-drug conjugates, and immune checkpoint inhibitors are also under investigation, aiming to improve outcomes through more targeted and immune-based strategies.
Additionally, there’s increasing interest in integrating digital health tools, such as wearable trackers and AI-powered monitoring systems, to enhance real-time treatment management and predict toxicity risks. As treatment becomes more individualized and data-driven, the future holds promise for optimizing outcomes while reducing unnecessary toxicity — reshaping how HER2-positive breast cancer is managed across all stages.
Survivorship Planning After TCHP
Completing the TCHP regimen is a major achievement, but the journey doesn’t end with the last infusion. Survivorship care is a vital phase that addresses not only ongoing surveillance for recurrence but also the physical, emotional, and social impacts of cancer treatment. Patients transitioning into survivorship may face lingering side effects such as fatigue, lymphedema, neuropathy, or cognitive changes (“chemo brain”).
Survivorship planning begins with a personalized follow-up schedule — typically including regular oncology visits, periodic imaging or lab work, and cardiac evaluations due to the long-term risks associated with HER2-targeted therapy. Patients are counseled on symptom monitoring and when to report concerning signs, such as new lumps or persistent pain.
Psychosocial support is integrated into survivorship, helping individuals cope with body image concerns, relationship changes, anxiety about recurrence, and reintegration into work or school. Healthy lifestyle counseling — focusing on diet, physical activity, sleep, and stress management — is also emphasized, as it may contribute to long-term well-being and reduced cancer risk.
Most importantly, survivorship represents a shift in focus: from treating cancer to rebuilding life. For many, it’s a period of reflection, adaptation, and renewed goals. With appropriate guidance and a strong support system, survivors can regain control and move forward with strength and confidence.
FAQ
What does TCHP stand for in breast cancer treatment?
TCHP refers to a chemotherapy regimen that includes four drugs: Docetaxel (T), Carboplatin (C), Trastuzumab (H), and Pertuzumab (P). This combination is used primarily to treat HER2-positive breast cancer and is effective due to its ability to target both rapidly dividing cells and the HER2 receptor.
Who is a candidate for TCHP therapy?
TCHP is commonly prescribed for patients with early-stage, locally advanced, or high-risk HER2-positive breast cancer. Oncologists may recommend it in either the neoadjuvant (before surgery) or adjuvant (after surgery) setting, depending on tumor size, lymph node involvement, and patient health status.
How is TCHP administered?
TCHP is given as an intravenous infusion every 21 days for a total of six cycles. Each session includes all four drugs, and patients are usually monitored closely during and after infusion. Trastuzumab and Pertuzumab are often continued every three weeks after chemotherapy to complete one year of HER2-targeted therapy.
What are the most common side effects of TCHP?
Side effects include fatigue, nausea, diarrhea, hair loss, low white blood cell counts (neutropenia), and peripheral neuropathy. These side effects vary in intensity and duration, but most can be managed with supportive medications and lifestyle adjustments.
How effective is the TCHP regimen?
TCHP is considered one of the most effective regimens for HER2-positive breast cancer. It achieves high rates of pathological complete response (pCR), which is strongly associated with better long-term survival outcomes, especially in hormone receptor-negative tumors.
What is pathological complete response (pCR)?
PCR means that no invasive cancer cells are found in the breast or lymph nodes after neoadjuvant therapy. Achieving pCR after TCHP is a favorable sign and often correlates with lower risk of recurrence and better survival statistics.
Is TCHP safe for patients with heart problems?
Because Trastuzumab and Pertuzumab can affect heart function, patients undergo cardiac monitoring before and during treatment. Those with pre-existing heart conditions may require alternative regimens or more frequent cardiac evaluations to minimize risk.
Can TCHP be used in metastatic breast cancer?
Yes, although it is more commonly used for early-stage disease, TCHP may be employed in selected metastatic cases where rapid tumor control is needed. In such cases, it is usually followed by maintenance therapy with targeted agents.
Are there alternatives to TCHP for HER2-positive breast cancer?
Yes. Alternatives include THP (Taxol + Herceptin + Perjeta) for patients with cardiac risks or AC-TH (anthracycline-based) regimens. Treatment choice depends on disease stage, patient comorbidities, and risk profile.
How long does the entire TCHP treatment last?
The chemotherapy portion typically lasts 18 weeks (six cycles). After that, HER2-targeted therapies like trastuzumab and pertuzumab may continue every 3 weeks for a total of 12 months from the start of treatment.
Will I lose my hair with TCHP?
Yes, hair loss is a common and expected side effect due to the inclusion of docetaxel, which affects rapidly dividing cells, including hair follicles. Hair usually begins to regrow a few weeks after chemotherapy ends.
Can TCHP affect fertility?
Yes, chemotherapy agents in TCHP can cause temporary or permanent ovarian suppression, especially in younger women. Fertility preservation options like egg freezing should be discussed with a reproductive specialist before starting treatment.
How is fatigue managed during TCHP?
Fatigue is one of the most common side effects. Management includes adequate rest, light physical activity (like walking), hydration, proper nutrition, and sometimes medications to treat underlying anemia or inflammation.
What support services are recommended during treatment?
Patients are encouraged to use oncology social work, support groups, nutrition counseling, and psychological services. Navigators or care coordinators can also help with logistics, medication access, and emotional support.
What happens after completing TCHP?
Patients transition to the survivorship phase, which includes regular follow-up visits, imaging if needed, cardiac monitoring, and addressing any lingering side effects. Lifestyle and wellness planning are also introduced to support long-term health.









