Symptoms of Low Iron Levels in Adults: What to Watch For and How to Treat It
- Why Iron Matters: The Role It Plays in Your Body
- Common Early Symptoms of Low Iron in Adults
- Progression of Iron Deficiency
- Who’s Most at Risk for Low Iron?
- How Low Iron Affects Your Brain and Mood
- Physical Signs: Hair, Skin, Nails, and Tongue
- Common Causes of Low Iron in Adults
- How to Test for Iron Deficiency
- What Happens If Iron Deficiency Is Left Untreated?
- Iron Supplements and Treatment Options
- Best Dietary Sources of Iron and Nutrient Pairings
- Why Women Need to Monitor Iron More Closely
- Low Iron and Athletic Performance: What Active Adults Need to Know
- Iron Absorption: What Helps and What Hurts
- Understanding Iron Loss Through Blood Donation or Injury
- How Long Does It Take to Fully Recover from Iron Deficiency?
- FAQ – Symptoms of Low Iron in Adults: 15 Key Questions Answered

Why Iron Matters: The Role It Plays in Your Body
Iron is essential for making hemoglobin — the protein in red blood cells that carries oxygen throughout your body. Without enough iron, your cells literally don’t get the oxygen they need to function properly.
Low iron can affect everything from energy and brain function to immunity and muscle strength. It’s especially important in women, vegetarians, endurance athletes, and people with digestive conditions that impair absorption.
And here’s the kicker: you can have low iron for months — even years — before it shows up clearly in a blood test. That’s why understanding the early signs and staying alert to your body is so important.
Common Early Symptoms of Low Iron in Adults
The earliest signs of low iron are subtle and easy to ignore. Many people chalk them up to stress, aging, or “just being busy.” But in my experience, these signs are often the body’s quiet way of asking for help.
You might notice:
- Feeling unusually tired, even after sleep
- Shortness of breath during normal activities
- Dizziness or lightheadedness when standing up
- Pale or dull skin tone
- Headaches or brain fog
- Cold hands and feet
- Reduced exercise tolerance
- Trouble concentrating or remembering
If you’re experiencing several of these symptoms, especially on a recurring basis, it’s worth looking into — even if your iron is still “in range.” Subclinical deficiencies can still impact how you feel day to day.
Progression of Iron Deficiency
| Stage | Hemoglobin / Ferritin Levels | Common Symptoms | Notes on Diagnosis |
| Normal Iron Storage | Ferritin > 30 ng/mL | None | Stable iron levels |
| Depleted Stores | Ferritin 12–30 ng/mL | Fatigue, exercise intolerance, dull skin | May not show up in hemoglobin yet |
| Functional Deficiency | Ferritin < 12 ng/mL | Fatigue, paleness, headaches | Body lacks iron for red blood cells |
| Iron Deficiency Anemia | Ferritin < 10, low hemoglobin | Shortness of breath, dizziness, chest pain | Visible on full blood count |
| Severe IDA | Hemoglobin < 9 g/dL | Extreme weakness, rapid heartbeat, hair loss | Requires medical treatment |
Catching iron deficiency before it becomes anemia makes treatment faster, safer, and less disruptive to your health. Always ask for ferritin, not just hemoglobin, when testing for iron.
Who’s Most at Risk for Low Iron?
Iron deficiency doesn’t affect everyone equally. Based on what I’ve seen, the risk spikes in certain groups — often without them realizing it.
The most at-risk populations include:
- Women of childbearing age due to menstruation
- Pregnant women, whose blood volume expands significantly
- Vegetarians and vegans, who may lack heme iron (the more easily absorbed form)
- Endurance athletes, especially runners, due to red blood cell damage and iron loss through sweat
- People with GI issues like celiac disease, Crohn’s, or after gastric surgery
- Frequent blood donors
- Older adults, who may have reduced absorption or chronic inflammation
It’s also surprisingly common among teens, due to rapid growth, and among postpartum women, who may not realize they lost significant iron during childbirth.
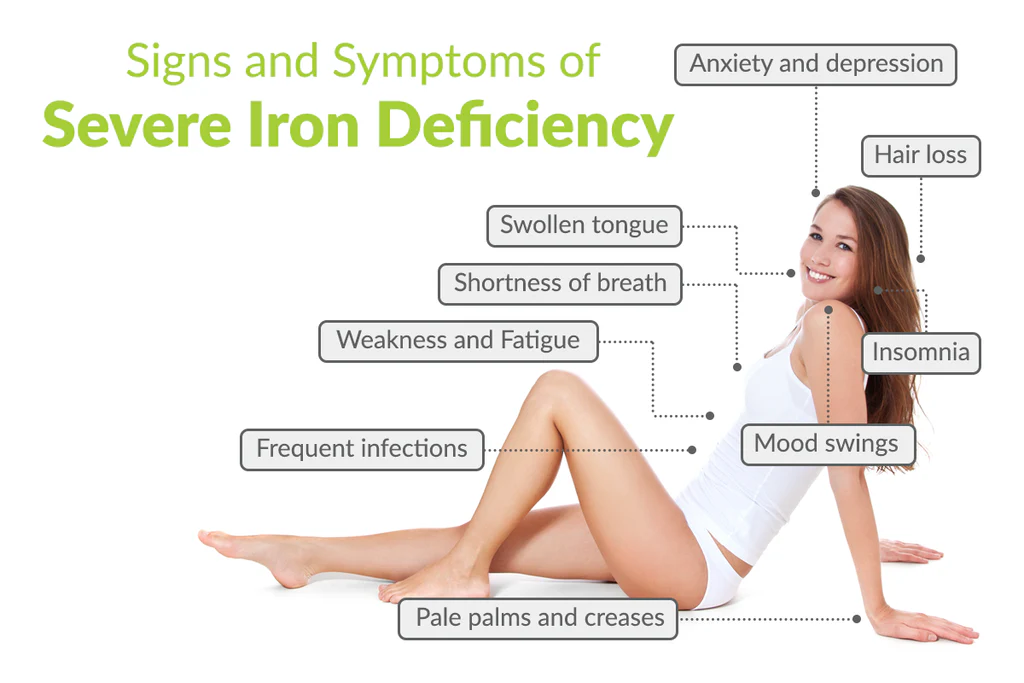
How Low Iron Affects Your Brain and Mood
If you’ve ever felt like your brain is in a fog, your memory is slipping, or your mood is dipping for no clear reason — iron may be part of the puzzle. I’ve seen these symptoms firsthand, and they often improve dramatically once iron is corrected.
Iron helps your brain process oxygen and produce key neurotransmitters like dopamine and serotonin. When iron is low, these systems start to struggle. The result?
- Difficulty focusing or retaining information
- Irritability or emotional sensitivity
- Mild depression or anxiety
- Restlessness or fatigue that feels mental, not physical
Some of my clients said they just “didn’t feel like themselves” — until they addressed iron levels. What makes it tricky is that these changes often happen gradually. You don’t notice them until they start affecting daily life.
Physical Signs: Hair, Skin, Nails, and Tongue
Iron deficiency often shows up on the surface before it’s ever caught in bloodwork. As someone who’s coached women through health resets, I always ask about these visual signs — because they’re early warning flags.
Hair loss is a big one. You may notice excessive shedding in the shower or a thinning ponytail. Hair can also become dry, brittle, or stop growing.
Skin may appear pale, sallow, or unusually dry — especially around the mouth or eyes. Some people develop a yellowish or “washed out” look, even if they feel okay otherwise.
Nails become thin, ridged, or spoon-shaped, and some people develop vertical lines or brittleness that doesn’t respond to topical treatments.
An unusual but very specific sign is the tongue becoming smooth, pale, or sore — sometimes with tiny cracks or sensitivity to acidic foods. If you notice these changes, it’s time to look deeper.
Common Causes of Low Iron in Adults
Understanding the root cause is the first step toward fixing low iron. From what I’ve seen, it’s rarely “just a diet problem.” Often, it’s a mix of absorption issues, lifestyle habits, or hidden blood loss.
Some of the most common culprits include:
- Heavy menstrual periods, especially with clots or prolonged flow
- Digestive disorders (like IBS, celiac, Crohn’s, or ulcers)
- Poor dietary intake, especially if relying on plant-based sources only
- Regular NSAID use (ibuprofen, aspirin), which can cause hidden GI bleeding
- Pregnancy or breastfeeding, due to increased demand
- Blood donation, especially if frequent
- Low stomach acid, which impairs iron absorption — common with age or antacid use
I’ve also seen iron depletion linked to intense physical training, frequent long-distance running, or crash dieting — all of which increase metabolic demand while reducing reserves.
How to Test for Iron Deficiency
Getting tested is straightforward — but most people don’t get the right tests. I always recommend a full iron panel, not just hemoglobin, especially if you have fatigue with normal blood counts.
Here’s what to ask your doctor for:
- Ferritin: the best marker of iron storage
- Serum iron
- Total Iron Binding Capacity (TIBC)
- Transferrin saturation
- Hemoglobin and hematocrit: assess anemia
- Reticulocyte count (sometimes) to measure red cell production
Ferritin is particularly important. Levels below 30 ng/mL may signal depleted stores — even if hemoglobin looks normal. Inflammation can mask the problem, so labs should be interpreted with symptoms in mind.
Also, always try to get tested fasting, in the morning, and ideally before taking any iron supplements that could skew results.
What Happens If Iron Deficiency Is Left Untreated?
I’ve worked with clients who ignored their symptoms for months — sometimes years — thinking their fatigue or weakness was “just life.” But left unaddressed, iron deficiency can spiral into serious health consequences.
Here’s what can happen over time:
- Full-blown iron deficiency anemia, with severe exhaustion and shortness of breath
- Cognitive dysfunction, including memory loss and reduced focus
- Reduced immunity, leading to frequent infections or slow wound healing
- Increased risk of complications during pregnancy, including low birth weight or preterm delivery
- Heart strain, including irregular heartbeat or even heart failure in older adults
What makes this condition tricky is how quietly it progresses. You may adapt to lower energy levels without realizing how far you’ve slipped — until treatment brings you back to what “normal” really feels like.
Iron Supplements and Treatment Options
Once diagnosed, iron deficiency can often be reversed — but it takes consistency and the right approach. I’ve guided many clients through this process, and a few key lessons always come up.
First, your doctor will likely recommend an oral iron supplement, such as:
- Ferrous sulfate
- Ferrous gluconate
- Ferrous fumarate
These are typically taken on an empty stomach with vitamin C (like orange juice) to boost absorption. But they can cause constipation, nausea, or stomach upset, so many people give up early.
In that case, alternatives include:
- Lower-dose iron taken twice a day
- Iron bisglycinate (a gentler form)
- Liquid iron, for sensitive digestion
- IV iron infusions, for severe cases or when oral options fail
Always recheck iron levels after 6–8 weeks to track progress — especially ferritin, which rises slowly over time.
Best Dietary Sources of Iron and Nutrient Pairings
Even with supplements, what you eat matters. I always encourage clients to include iron-rich foods daily, especially during recovery.
Top iron-rich foods include:
- Red meat (especially beef and lamb)
- Chicken thighs and liver
- Seafood, especially oysters, clams, sardines
- Legumes: lentils, chickpeas, white beans
- Tofu and tempeh
- Leafy greens (spinach, chard, kale)
Pair iron-rich meals with vitamin C sources like bell peppers, citrus fruits, or tomatoes to enhance absorption.
Avoid pairing iron-heavy meals with calcium, coffee, or tea, which inhibit absorption. For example, don’t drink milk or tea with a spinach salad if you’re relying on that iron.
Why Women Need to Monitor Iron More Closely
In my experience, women — especially menstruating, pregnant, or postpartum — need to be extra vigilant about iron. Monthly blood loss, pregnancy demands, and hormonal shifts make deficiency more likely.
Key times to test or supplement include:
- Heavy periods (lasting over 7 days or with clots)
- Pregnancy (especially second and third trimester)
- Postpartum recovery — up to 6 months after birth
- Perimenopause, if cycles become erratic and heavy
- Vegetarian or vegan diets
I often recommend that women keep track of symptoms monthly, especially fatigue, mood, and hair changes. A small drop in iron can throw off your energy and emotional balance long before labs detect anemia.
Low Iron and Athletic Performance: What Active Adults Need to Know
Over the years, I’ve worked with many athletes and active adults who were shocked to learn that their fatigue, poor recovery, or drop in endurance was due to iron deficiency. It’s especially common in female runners, cyclists, and anyone training intensely.
Here’s what I often see:
- Decreased VO2 max (your body’s ability to use oxygen efficiently)
- Slower recovery between workouts
- More frequent muscle soreness
- Increased injuries due to fatigue and poor tissue repair
Why does this happen? Exercise increases red blood cell turnover and iron loss through sweat and gastrointestinal microbleeding. Combine that with high physical demand and you’ve got a recipe for depletion — even with a good diet.
Iron Absorption: What Helps and What Hurts
Many of my clients didn’t realize how many everyday habits affect iron absorption. Even if you’re eating or supplementing correctly, poor absorption can undo all your efforts.
Things that help:
- Taking iron with vitamin C (orange juice, lemon water, bell pepper)
- Having iron on an empty stomach (if tolerated)
- Separating iron from calcium, tea, coffee, or dairy
Things that reduce absorption:
- High-calcium meals or supplements (especially dairy-heavy breakfasts)
- Tannins in black tea or red wine
- Antacids and PPIs (reduce stomach acid, which is needed to absorb iron)
On my recommendation, small habit changes — like shifting iron intake to mid-morning or before bed — can make a huge difference in lab results over time.
Understanding Iron Loss Through Blood Donation or Injury
Blood donation is a generous act — but it’s also a surprisingly common trigger for iron depletion. I’ve worked with frequent donors (especially women) who developed symptoms simply from giving blood too often without recovery time.
Each unit of donated blood removes 200–250 mg of iron, which may take weeks or months to replenish.
Other causes of sudden or chronic iron loss include:
- Nosebleeds
- Hemorrhoids or rectal bleeding
- Stomach ulcers
- Surgical recovery
If you give blood more than twice per year, it’s wise to test your ferritin regularly and take low-dose iron as maintenance.
How Long Does It Take to Fully Recover from Iron Deficiency?
This is one of the most common questions I get — and the answer depends on severity, absorption, and consistency.
Mild cases (low ferritin, normal hemoglobin) often improve within 4–6 weeks of supplementation. You may feel better in a few days, but full replenishment of iron stores takes time.
Moderate to severe cases can take 2–4 months, or longer if absorption is impaired. In some cases, IV iron offers a faster solution — but even then, symptoms may take weeks to resolve fully.
In my experience, the key to recovery is not just restoring numbers — it’s maintaining healthy levels long-term, especially if your body tends to drop quickly.
FAQ – Symptoms of Low Iron in Adults: 15 Key Questions Answered
Can low iron make you tired even if you’re sleeping enough?
Yes — in my experience, this is one of the most common early signs. I’ve seen people sleep 9 hours and still feel like they’ve been hit by a truck. If rest doesn’t restore your energy, iron might be the missing link.
Is dizziness always a sign of anemia?
Not always, but I’ve noticed that people with low ferritin often get lightheaded, especially when standing quickly. It’s a signal your oxygen delivery system isn’t working at full capacity.
How fast can low iron develop?
It depends on the cause. After surgery, childbirth, or heavy bleeding, levels can drop in days. In other cases, like poor diet, it creeps in slowly over months. I’ve seen both — and both matter.
Can low iron affect your mental focus?
Definitely. On my clients, brain fog is often one of the earliest complaints. Poor concentration, word recall issues, or memory slips can all be tied to oxygen-starved brain tissue.
Why do nails change with iron deficiency?
Iron helps maintain healthy skin and nails. When levels fall, the body prioritizes oxygen over nail growth, leading to brittleness or ridges. I’ve spotted this often in subtle form.
Does low iron cause cold hands and feet?
Yes. Reduced oxygen delivery and slower circulation are to blame. If you’re always bundled up while others feel fine, it might not be “just you” — I always suggest checking iron.
Can you still be iron deficient if your hemoglobin is normal?
Absolutely. I’ve seen this in dozens of cases. Ferritin — your iron storage marker — can be low even when hemoglobin is still within range. Always test both.
Is it safe to take iron supplements on your own?
I usually suggest checking levels first. Over-supplementing can cause issues like constipation or even iron overload. That said, low-dose iron paired with vitamin C is often safe short term.
What foods help raise iron levels naturally?
Red meat, chicken, lentils, leafy greens, and shellfish are my go-to recommendations. Combine them with vitamin C-rich produce to boost absorption.
Can low iron cause anxiety or mood swings?
Yes — and I’ve seen mood stabilize dramatically with proper iron levels. Iron plays a role in neurotransmitter production, which affects both energy and emotion.
How often should you test iron levels?
If you’ve had deficiency before, I usually recommend testing every 6–12 months — more frequently if you’re pregnant, breastfeeding, or menstruating heavily.
Does cooking in a cast iron pan help?
It can! I’ve measured increased iron content in meals made this way. While it won’t replace supplements, it’s a helpful habit to add iron to your diet passively.
Are vegetarians more likely to have low iron?
Yes, especially without careful planning. Plant-based iron (non-heme) is harder to absorb. I’ve helped many vegetarians manage this by optimizing their food pairings and timing.
Is it possible to have too much iron?
Yes — especially if supplementing without bloodwork. Conditions like hemochromatosis cause iron overload, which can damage organs. Always test first if you’re unsure.
What’s the fastest way to raise iron levels?
In my experience, a combo of iron-rich foods + daily supplements (taken correctly) works fastest. For severe cases, IV iron can raise levels within days under medical supervision.









