Swollen Lymph Nodes in Leukemia
Swollen Lymph Nodes in Leukemia: Causes, Diagnosis, and When to Worry
- Why Do Lymph Nodes Swell in Leukemia?
- The Underlying Mechanism of Lymph Node Enlargement in Leukemia
- How Common Are Swollen Lymph Nodes in Leukemia Patients?
- What Causes This Symptom in Leukemia Patients?
- When Should You Be Concerned About Lymph Node Swelling?
- How Doctors Diagnose the Cause of Lymph Node Enlargement
- How Lymph Node Swelling Is Treated in Leukemia Patients
- Will Swollen Lymph Nodes Go Away After Treatment?
- What Hematologists and Oncologists Say About This Symptom
- Questions to Ask Your Doctor
- FAQ: Swollen Lymph Nodes in Leukemia
Why Do Lymph Nodes Swell in Leukemia?
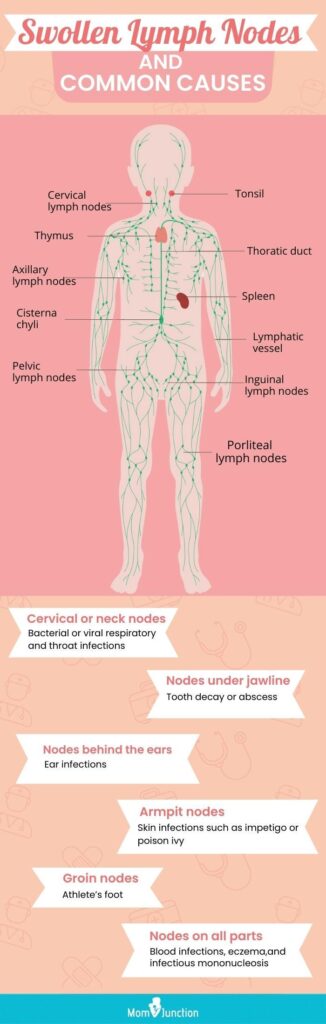
Swollen lymph nodes—also known as lymphadenopathy—are one of the early signs of leukemia, a blood cancer that affects white blood cells. Unlike solid tumors, leukemia spreads through the bloodstream and bone marrow, often disrupting normal immune responses. One of the consequences is abnormal activity or enlargement of lymph nodes.
In leukemia, lymph node swelling doesn’t result from infection, as in most common cases, but from the accumulation of malignant leukocytes (white blood cells). These immature or dysfunctional cells infiltrate lymphatic tissue, causing it to swell and harden. The nodes may be painless, rubbery, and felt most commonly in the neck, armpit, or groin.
Patients with certain types of leukemia—particularly chronic lymphocytic leukemia (CLL) and acute lymphoblastic leukemia (ALL)—often report visible or palpable node enlargement, which may wax and wane depending on disease activity or treatment.
Unlike lymphoma, where the lymph node is the primary site of disease, in leukemia the swelling reflects systemic involvement. Understanding this difference is crucial for both diagnosis and treatment strategy.
The Underlying Mechanism of Lymph Node Enlargement in Leukemia
Leukemia begins in the bone marrow, where it causes an overproduction of abnormal white blood cells. These immature or mutated cells fail to perform normal immune functions and begin to accumulate in various organs, including lymph nodes. Over time, these nodes become reservoirs of leukemic cells.
The immune system may also react by triggering inflammation within the nodes. As the disease progresses, lymphatic channels can become clogged with these abnormal cells, preventing proper drainage and causing further swelling.
In acute leukemias, such as ALL and AML, the onset of lymphadenopathy is rapid and often associated with systemic symptoms like fever and fatigue. In chronic forms like CLL, lymph node swelling can be subtle at first but gradually become more pronounced.
Lymph node involvement may also mimic metastases from other types of cancer, which is why differentiation via laboratory and biopsy testing is essential.
How Common Are Swollen Lymph Nodes in Leukemia Patients?
The frequency of lymph node swelling varies depending on the type and stage of leukemia. In some cases, it is one of the earliest physical signs prompting a medical evaluation. In others, it emerges during progression or relapse.
Lymph Node Involvement by Leukemia Type
| Leukemia Subtype | Prevalence of Swollen Nodes |
| Chronic Lymphocytic Leukemia (CLL) | ~80–90% of patients report lymphadenopathy |
| Acute Lymphoblastic Leukemia (ALL) | ~60–70%, especially in children |
| Acute Myeloid Leukemia (AML) | Less common (~20%), usually with advanced disease |
| Chronic Myeloid Leukemia (CML) | Rare, unless blast crisis develops |
In pediatric patients with ALL, enlarged lymph nodes—especially in the cervical area—may be mistaken for reactive nodes due to infection. For this reason, bloodwork and imaging play a central role in distinguishing leukemia from other causes.
Routine blood tests for lymphomas and leukemias, including complete blood count (CBC) with differential and flow cytometry, are often the first step in clarifying the nature of lymph node enlargement.
What Causes This Symptom in Leukemia Patients?
Several biological and treatment-related factors contribute to lymph node swelling in leukemia. These include direct infiltration by cancer cells, immune system overactivation, and even reactions to treatment.
Overview of Causes of Swollen Lymph Nodes in Leukemia
| Cause Type | Mechanism |
| Leukemic Cell Infiltration | Malignant cells invade lymphatic tissue and displace normal immune cells |
| Immune System Response | Cytokine release and inflammation triggered by abnormal white cells |
| Infection (Secondary) | Immunosuppression leads to viral or bacterial infections that inflame nodes |
| Drug-Induced | Some therapies can cause reactive lymphadenopathy or immune reconstitution |
| Tumor Lysis or Remission Flare | Rapid cell breakdown or immune activation during treatment may enlarge nodes temporarily |
Understanding the cause of node swelling helps clinicians decide whether it reflects disease activity, a treatment reaction, or a superimposed infection—each requiring a different management approach.
When Should You Be Concerned About Lymph Node Swelling?
Not all lymph node swelling in leukemia is a sign of immediate danger—but certain characteristics should raise concern. When nodes are rapidly growing, painful, or associated with systemic symptoms such as fever, night sweats, or unexplained weight loss, urgent evaluation is needed.
Swelling in unusual locations—such as deep abdominal or mediastinal nodes—can compress nearby organs and cause breathing difficulty, digestive obstruction, or vascular compromise. These scenarios often signal aggressive disease progression or transformation into a more severe phase.
In patients undergoing treatment, new or worsening lymphadenopathy may represent relapse, drug resistance, or complications like tumor lysis syndrome. Therefore, any significant change in size, consistency, or tenderness of lymph nodes should be promptly reported.
Additionally, if lymph node swelling is accompanied by skin changes, persistent fatigue, or bleeding symptoms, this may suggest a broader shift in the leukemia’s behavior—sometimes mimicking metastases from solid tumors.
How Doctors Diagnose the Cause of Lymph Node Enlargement
The evaluation of swollen lymph nodes in leukemia involves a combination of physical exam, imaging, and laboratory analysis. Since lymphadenopathy can result from disease, treatment, or infection, multiple diagnostic tools are often used together.
Common Diagnostic Methods for Lymphadenopathy in Leukemia
| Method | Diagnostic Purpose |
| Complete Blood Count (CBC) | Assesses white cell abnormalities and anemia |
| Peripheral Blood Smear | Identifies blasts or abnormal lymphocytes |
| Flow Cytometry | Detects cell surface markers to classify leukemia |
| Ultrasound or CT Scan | Evaluates node size, location, and compression of structures |
| Lymph Node Biopsy | Differentiates between leukemic infiltration and other causes |
| Bone Marrow Aspiration | Confirms systemic disease burden |
In some cases, blood tests for lymphomas may be included, especially when the diagnosis is unclear or the presentation mimics lymphoma. Immunophenotyping helps distinguish leukemia subtypes and determines treatment responsiveness.
Doctors also assess the response of swollen lymph nodes over time to therapy—shrinking nodes often indicate effective treatment, while persistent or enlarging nodes may require a change in therapeutic approach.
How Lymph Node Swelling Is Treated in Leukemia Patients

The primary approach to treating lymph node enlargement in leukemia is to address the underlying malignancy. Once systemic therapy (chemotherapy, targeted therapy, or immunotherapy) begins, nodes often decrease in size as leukemic cells are cleared.
Treatment Modalities and Their Impact on Lymphadenopathy
| Treatment Type | Role in Managing Swollen Nodes |
| Systemic Chemotherapy | Reduces leukemic burden and shrinks infiltrated nodes |
| Targeted Therapy (e.g., BTK inhibitors) | Used in CLL to reduce node size and disease activity |
| Corticosteroids | Rapid anti-inflammatory effect on swollen lymph tissue |
| Monoclonal Antibodies | Target CD20 or other markers on leukemic cells within nodes |
| Radiation Therapy | Rarely used but may shrink nodes causing critical compression |
| Antibiotics/Antivirals | Treats secondary infections contributing to node swelling |
For patients in remission or on maintenance therapy, any recurrence of lymphadenopathy may lead to re-staging and therapy adjustment. In refractory cases, clinical trials may offer access to novel agents aimed at minimizing residual disease in lymphoid tissue.
Can Lymph Node Swelling Be Prevented or Managed Proactively?
While lymphadenopathy in leukemia cannot always be prevented, proactive monitoring and prompt treatment can minimize its impact and prevent complications. Regular blood tests and physical exams during and after treatment help detect changes early.
Patients at high risk—those with bulky disease at diagnosis, treatment resistance, or genetic mutations—may benefit from more aggressive or tailored treatment plans. Lifestyle factors like maintaining good hygiene, avoiding exposure to infections, and adhering to medication schedules can also reduce reactive node enlargement.
Strategies to Control or Prevent Lymphadenopathy
| Preventive Strategy | Benefit |
| Routine physical and lab monitoring | Early detection of node changes |
| Adherence to treatment protocols | Reduces disease-related lymph node involvement |
| Infection prevention (handwashing, vaccines) | Lowers reactive lymphadenopathy risk |
| Genetic profiling and targeted therapy | Guides more effective node-specific treatment |
| Regular imaging in high-risk cases | Identifies deep node swelling not visible externally |
While not all swelling is avoidable, especially in active cancer phases, these strategies can help manage symptoms and improve quality of life.
Will Swollen Lymph Nodes Go Away After Treatment?
In most cases, lymph node swelling in leukemia improves significantly after initiating effective therapy. As the leukemic burden decreases, the nodes—once packed with malignant cells—tend to shrink or return to normal size.
The timeline of resolution varies depending on the leukemia subtype, initial disease burden, and treatment response. In acute leukemias, lymphadenopathy may resolve within weeks of chemotherapy initiation. In chronic types like CLL, nodes may take longer to regress, especially if bulky at presentation.
However, in some patients, lymph nodes may remain mildly enlarged despite good control of leukemia. This could be due to residual fibrosis or reactive changes rather than active disease. Persistent or recurrent swelling may also indicate relapse, transformation to aggressive disease, or the emergence of drug resistance.
Prognosis of Lymph Node Resolution
| Clinical Scenario | Likelihood of Resolution |
| Acute leukemia with early chemotherapy | High resolution in weeks |
| Chronic leukemia under targeted therapy | Gradual reduction over months |
| Refractory or relapsed disease | Swelling may persist or worsen |
| Residual node enlargement without blasts | May remain stable and benign |
Regular follow-up and response monitoring help distinguish between persistent benign changes and signs of renewed cancer activity.
What Hematologists and Oncologists Say About This Symptom
Leukemia experts emphasize that while lymph node swelling can be alarming for patients, it is a common and manageable manifestation of the disease. Oncologists frequently reassure families that node enlargement often correlates with disease activity and responds well to systemic treatment.
Specialists caution, however, that not all swelling is due to leukemia itself. Infections, autoimmune flares, or drug reactions may also cause node enlargement. Thus, evaluating context, history, and lab findings is key to appropriate management.
Hematologists also highlight the importance of patient self-monitoring. Noticing changes in lymph node size, location, or tenderness can help detect relapse early. Particularly in CLL, where progression can be slow, this vigilance plays a critical role in timely intervention.
If swollen nodes press on nerves or organs, oncologists may use temporary interventions like corticosteroids or low-dose radiation to relieve symptoms, while continuing systemic therapy.
Questions to Ask Your Doctor
Clear communication with your healthcare team is essential in understanding and managing swollen lymph nodes during leukemia. Below are questions to guide meaningful discussion with your oncologist or hematologist:
| Patient Questions | Why It Matters |
| Are my swollen lymph nodes caused by leukemia or another issue? | Helps determine treatment path |
| How can you tell if the swelling is dangerous? | Clarifies risk of complications |
| Should I have a biopsy or scan to investigate further? | Explores diagnostic clarity |
| Will treatment make the nodes go away completely? | Sets realistic expectations |
| How long will it take for the swelling to resolve? | Helps with monitoring and patience |
| Are swollen lymph nodes a sign that my disease is progressing? | Evaluates relapse or resistance |
| What labs should I follow to track this symptom? | Ensures proper surveillance |
| Can the swelling be painful or cause other symptoms? | Anticipates related issues |
| Should I avoid touching or pressing on the nodes? | Prevents irritation or inflammation |
| Can these nodes become infected? | Flags secondary risks |
| What if the swelling returns after remission? | Plans for long-term management |
| Do swollen nodes affect my prognosis? | Addresses patient fears |
| Are there supportive treatments to help with this? | Explores symptom relief options |
| Is this a common symptom in my type of leukemia? | Provides reassurance or alerts |
| Should I get a second opinion if swelling persists? | Encourages informed decision-making |
FAQ: Swollen Lymph Nodes in Leukemia
1. Is it normal to have swollen lymph nodes if I have leukemia?
Yes. It’s one of the most common physical signs, especially in chronic lymphocytic and acute lymphoblastic leukemia.
2. Are swollen lymph nodes painful in leukemia?
Usually, they are painless. If they become painful, it may indicate rapid growth, infection, or compression of nearby tissues.
3. Can lymph nodes stay enlarged even after leukemia is treated?
Yes, some nodes remain slightly enlarged due to scarring or fibrosis, even when the cancer is in remission.
4. How are swollen lymph nodes different in leukemia vs. lymphoma?
In leukemia, node swelling reflects systemic blood cancer, while in lymphoma, the node itself is the primary tumor site.
5. Do blood tests show why my lymph nodes are swollen?
Often, yes. CBC, flow cytometry, and other blood tests for lymphomas help identify abnormal cells linked to the swelling.
6. What imaging is used to examine swollen lymph nodes?
Ultrasound, CT scans, and PET scans are commonly used to evaluate size, location, and possible complications.
7. Should I be concerned about one-sided or asymmetric swelling?
Possibly. Asymmetry or rapid enlargement should be evaluated to rule out localized complications or transformation.
8. Can infections cause lymph nodes to swell even with leukemia?
Yes. Leukemia patients are immunocompromised and prone to infections that can inflame lymph nodes independently.
9. What’s the role of lymph node biopsy in leukemia?
It helps confirm or rule out other causes of swelling, such as lymphoma or metastases from another cancer.
10. Is it safe to delay treatment if only lymph node swelling is present?
Not recommended. Swollen nodes can be a warning sign of active or worsening disease and should be addressed promptly.
11. Can exercise or massage reduce lymph node swelling?
No. This can actually cause discomfort or injury. Medical treatment is required to reduce size.
12. What if the swelling affects my breathing or swallowing?
This is a medical emergency, often due to large mediastinal or cervical nodes compressing vital structures.
13. Do steroids help with swollen lymph nodes in leukemia?
Yes. Steroids are sometimes used to shrink lymphatic tissue quickly, especially in emergencies.
14. Is lymph node swelling more common in children or adults with leukemia?
It’s common in both, but certain subtypes like ALL in children show more prominent node involvement.
15. How often should I monitor lymph node size during leukemia?
At every check-up, and more frequently if there are symptoms like pain, fever, or fatigue. Report any rapid changes to your doctor.












