Sudden Tiredness Symptoms, Evaluation, and Treatment Options
Sudden Tiredness: Definition and Clinical Context
Definition and Core Features
Fatigue is a broad medical term describing a subjective feeling of tiredness, lack of energy, or reduced capacity for physical or mental activity. It reflects a state in which normal levels of alertness or endurance cannot be sustained. Fatigue may present as a purely physical sensation, cognitive slowing, or both. In clinical settings, it is recognized as a common and often non-specific symptom rather than a disease in itself.
Sudden tiredness refers to the acute onset of this sensation, developing over hours or days rather than persisting for weeks or months. This contrasts with chronic fatigue, which is prolonged and may reflect underlying systemic or psychological disorders. Differentiating between these patterns is clinically important because acute fatigue is more often linked to short-term physiological or environmental factors, whereas chronic forms usually suggest persistent medical or psychological conditions.
- Acute (sudden) fatigue: Develops quickly and often relates to short-term physiological or situational factors.
- Chronic fatigue: Persists for weeks or months and may indicate ongoing medical or psychological illness.
Epidemiology and Clinical Relevance
Fatigue is among the most frequent complaints encountered in primary care, affecting individuals of all ages and backgrounds. Despite its prevalence, only a small proportion of people presenting with tiredness are ultimately diagnosed with serious organic disease. Most cases are attributed to benign or reversible influences such as insufficient sleep, acute stress, or temporary lifestyle disruption.
Psychiatric and functional conditions, including depression, anxiety, and stress-related fatigue, account for a substantial share of clinical presentations. Because fatigue often arises from multiple overlapping causes, clinicians must determine whether it represents a transient imbalance or an early sign of systemic illness. Recognizing the difference between physiological tiredness and sudden-onset pathologic fatigue is essential for accurate diagnosis and management.

Common and Benign Causes of Sudden Tiredness
Lifestyle and Behavioral Factors
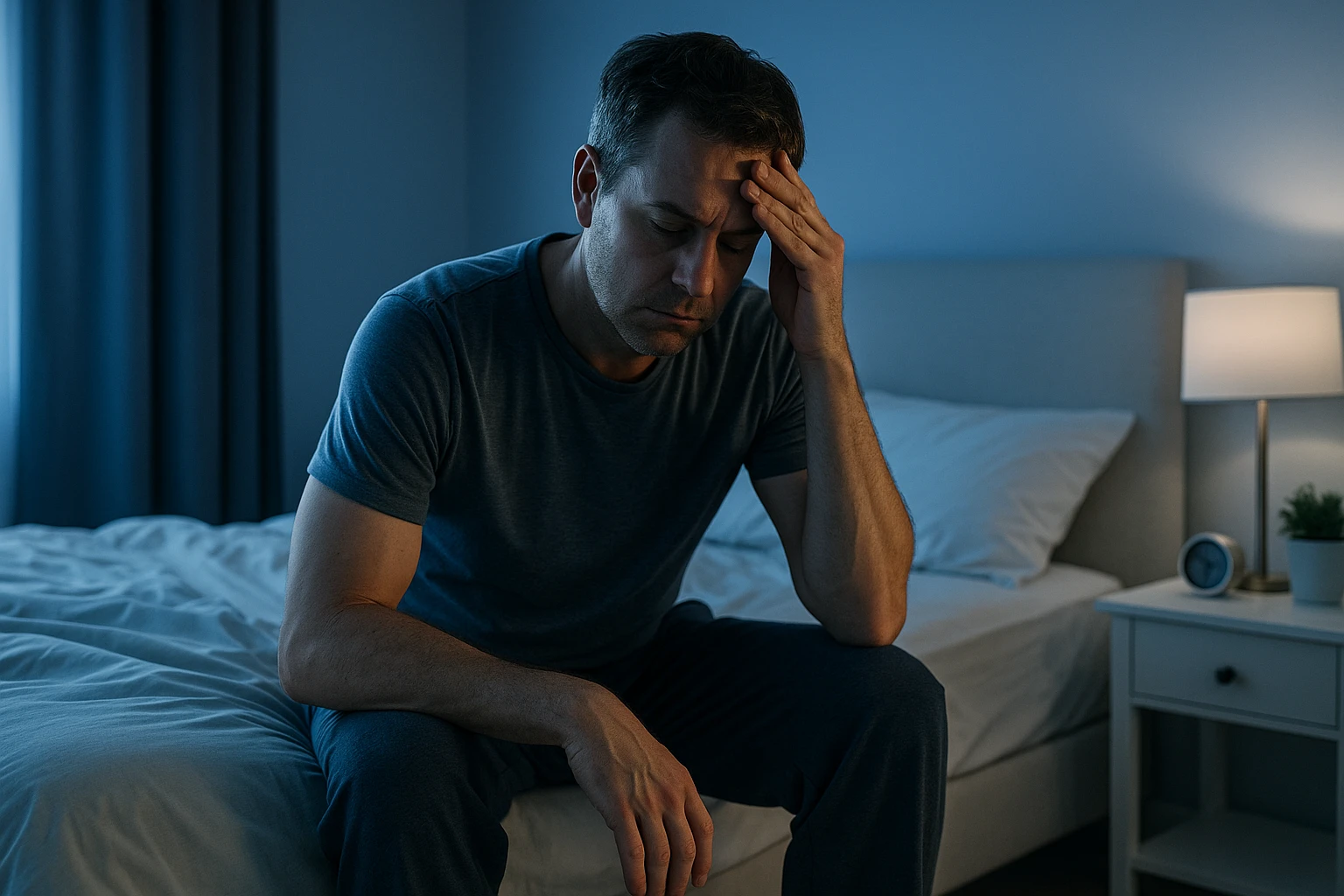
Many episodes of sudden tiredness can be traced to everyday habits and routines that disrupt the body’s natural energy regulation. Insufficient or poor-quality sleep is one of the most frequent contributors, as even a few nights of inadequate rest can impair alertness, concentration, and physical stamina. High workload and prolonged exertion without adequate recovery cause temporary exhaustion that is physiological rather than pathological.
- Insufficient or disrupted sleep
- High workload or prolonged exertion
- Poor nutrition or dehydration
- Physical inactivity or overtraining
Other behavioral influences include inadequate nutrition, dehydration, and inactivity, which limit the body’s ability to maintain energy balance. Conversely, overtraining or excessive exercise without rest may result in fatigue through muscular or metabolic strain. These factors are generally reversible once sleep, nutrition, and workload are corrected.
Psychological and Emotional Factors
Emotional stress and psychological strain are common but often underrecognized causes of sudden tiredness. Acute stress elevates hormones such as cortisol and adrenaline, temporarily increasing alertness, but sustained stress depletes these reserves, leading to a rapid drop in perceived energy. Anxiety can also interfere with concentration and sleep, compounding exhaustion.
Depression is another frequent cause of fatigue seen in clinical practice. It alters neurotransmitter balance and motivation, resulting in reduced physical and mental energy. Because these psychological and psychiatric conditions are common in primary care, they must be considered when evaluating unexplained tiredness even in the absence of a clear medical cause.

Circadian and Occupational Disruption
Irregular sleep-wake schedules can produce transient but significant fatigue. Shift workers often experience sudden tiredness at night due to misalignment between work schedules and the body’s internal circadian rhythm. This mismatch affects hormonal cycles and sleep quality, reducing alertness during waking hours.
- Shift work disrupting normal sleep patterns
- Jet lag from frequent travel across time zones
- Inconsistent daily routines affecting circadian rhythm
Jet lag, frequent travel, and inconsistent routines similarly disrupt synchronization between brain sleep centers and environmental cues like light exposure. These forms of occupational fatigue are generally short-lived but can affect performance and well-being if not managed through adequate rest and gradual adaptation.
Medical Causes and Warning Signs of Sudden Tiredness
Major Medical Causes
While many cases of sudden tiredness are benign, several medical conditions can underlie acute or rapidly developing fatigue. These include disorders that affect oxygen transport, hormone balance, energy metabolism, and the body’s response to illness.
- Anemia: Reduced oxygen delivery to tissues causes weakness and exhaustion.
- Thyroid or adrenal disorders: Endocrine dysfunction impairs metabolic regulation and energy levels.
- Cardiopulmonary diseases: Conditions such as heart failure, arrhythmias, or respiratory compromise decrease oxygenation and circulation.
- Infections and inflammation: Acute or chronic infections, autoimmune disease, and systemic inflammation can trigger fatigue.
- Metabolic disorders: Diabetes or electrolyte imbalances disrupt cellular energy production.
Although these causes are medically significant, most cases of fatigue in primary care arise from less serious mechanisms.
Medication-Related Fatigue
Certain prescription and over-the-counter medications can cause or worsen tiredness. Sedatives, antihypertensives, antidepressants, and some antihistamines reduce alertness or induce drowsiness. Chemotherapy agents, corticosteroids, and other systemic treatments may also produce fatigue as a side effect through metabolic or inflammatory pathways.
Identifying recent medication changes is an essential step in evaluating sudden-onset fatigue. In many cases, symptoms improve when the causative drug is adjusted or discontinued under medical supervision.
Red Flags: When to Seek Immediate Care
Although serious underlying illness is relatively rare among patients presenting with fatigue, certain associated symptoms require prompt attention. Red-flag indicators include:
- Unintentional weight loss
- Persistent or unexplained fever
- Night sweats
- Enlarged lymph nodes or abdominal organs
- Chest pain, shortness of breath, palpitations, or fainting
These signs may indicate infection, malignancy, or cardiopulmonary disease requiring urgent assessment. Recognizing these patterns early enables timely intervention and helps prevent complications.
When to See a Doctor: Sudden fatigue accompanied by chest pain, difficulty breathing, neurological symptoms, or unexplained fever should prompt immediate medical review.

Evaluation and Diagnosis of Sudden Tiredness
History and Clinical Assessment
The evaluation of sudden tiredness begins with a detailed medical history. Clinicians assess onset, duration, and fatigue pattern-determining whether it appeared abruptly or developed progressively. Questions about sleep quality, daily routines, recent stressors, and activity changes help distinguish physiological tiredness from illness-related fatigue. Reviewing medications, alcohol or caffeine intake, and psychosocial context provides insight into reversible factors.
- Onset, duration, and progression of fatigue
- Sleep habits and quality
- Workload, activity levels, and stress exposure
- Medication or substance use
- Psychological and social context
During physical examination, clinicians look for objective signs of systemic, endocrine, cardiopulmonary, neurologic, or psychiatric disease. Observations may include pallor suggesting anemia, thyroid enlargement, irregular heart rhythm, or respiratory abnormalities. Mental status, mood, and affect are assessed to identify emotional or psychiatric factors. This systematic approach ensures that serious or multisystem causes are not missed while avoiding unnecessary testing.
Laboratory and Imaging Evaluation
Initial testing is guided by clinical findings rather than broad screening. Common baseline studies include:
- Complete blood count (CBC) – evaluates anemia or infection
- Inflammatory markers – identifies possible systemic illness
- Metabolic profile – reviews renal and electrolyte balance
- Thyroid function tests – detects hormonal imbalance
Imaging or advanced diagnostics are reserved for cases with red-flag symptoms or abnormal findings suggesting specific disease, such as cardiopulmonary pathology or malignancy. Unfocused imaging and extensive test panels are discouraged as they increase cost and may produce incidental findings that complicate diagnosis.
Referral and Escalation
When initial evaluation does not identify a cause, or if concerning features are present, referral to a specialist is appropriate. Patients with endocrine abnormalities may be referred to endocrinology, those with cardiac or respiratory findings to cardiology or pulmonology, and individuals with persistent unexplained fatigue to internal medicine or psychiatry for further evaluation. Prompt referral helps ensure serious conditions are addressed efficiently while avoiding unnecessary interventions.

Management, Prognosis, and Knowledge Gaps in Sudden Tiredness
Targeted Management
The management of sudden tiredness centers on identifying and addressing its underlying cause. When a specific medical condition is present, treatment should target that disorder, such as correcting anemia, managing thyroid disease, treating infection, or adjusting medications that contribute to fatigue. For many patients, however, tiredness arises from modifiable lifestyle factors including inadequate sleep, poor diet, or psychological stress. In these situations, interventions that restore energy balance-such as improving sleep hygiene, increasing physical activity, and reducing stress-are often effective.
- Correcting anemia, thyroid imbalance, or infection
- Reviewing and adjusting medications contributing to fatigue
- Improving sleep hygiene and daily rest patterns
- Increasing physical activity gradually
- Managing stress through behavioral or relaxation techniques
For non-serious or transient causes, clinicians emphasize optimizing lifestyle behaviors, reviewing current medications for potential sedative effects, and establishing healthy daily routines. Addressing contributing factors early helps prevent chronic fatigue patterns and improves overall well-being without the need for extensive intervention.
Follow-up and Long-Term Outcomes
Follow-up and reassessment are essential components of managing unexplained or persistent fatigue. A period of observation allows clinicians to monitor for evolving conditions that may not have been evident during the initial evaluation. Repeat assessments should focus on new or worsening symptoms to ensure timely detection of any underlying disease. In most cases related to lifestyle imbalance or minor illness, symptoms gradually resolve with rest and behavioral adjustment.
Patients who present without red-flag features and who have normal results on targeted investigations generally have a low short-term risk of serious illness. This favorable outlook highlights the value of reassurance and supportive management, avoiding unnecessary testing while maintaining vigilance for clinical change over time.
Special Populations and Evidence Gaps
Research on sudden tiredness remains limited across specific populations. Factors such as sex-related hormonal variation, pregnancy-associated fatigue, and age-related decline in energy metabolism are not yet fully understood. Similarly, occupational influences-including shift work and circadian rhythm disruption-require further investigation to improve prevention strategies. Continued research is also needed to refine diagnostic criteria for acute fatigue and assess the cost-effectiveness of targeted diagnostic testing in diverse clinical contexts.
| Population | Key Consideration |
|---|---|
| Women | Hormonal variation and reproductive health influence fatigue patterns. |
| Pregnant individuals | Physiologic fatigue resulting from metabolic and circulatory changes. |
| Older adults | Reduced energy metabolism and comorbidity burden affect endurance. |
| Shift workers | Circadian rhythm disruption impacts sleep quality and daytime alertness. |
Recognizing these evidence gaps is vital to improving patient outcomes. Future studies that integrate biological, psychological, and social determinants of fatigue will enhance clinicians’ ability to distinguish benign from clinically significant tiredness with greater accuracy.

Frequently Asked Questions About Sudden Tiredness
- Why can tiredness appear suddenly even when you’ve slept well?
- Sudden tiredness can develop from short-term physiological changes, such as dehydration, low blood sugar, stress, or a mild viral illness, even without poor sleep.
- Is sudden tiredness always a sign of illness?
- Not always. Most cases stem from reversible factors like stress, poor nutrition, or disrupted sleep, but persistent or severe fatigue should be medically evaluated.
- How can stress or emotions cause sudden fatigue?
- Stress triggers hormonal changes that initially heighten alertness but later lead to energy depletion. Anxiety or emotional strain also disrupts sleep and focus, increasing fatigue.
- Which medical problems are most often linked with sudden tiredness?
- Conditions such as anemia, thyroid imbalance, heart or lung disease, and infections can cause acute fatigue by affecting oxygen, hormones, or metabolism.
- When should sudden tiredness be considered a red flag?
- If it occurs with chest pain, shortness of breath, fainting, fever, or unexplained weight loss, it may signal an urgent medical condition needing prompt care.
- Can medications make you feel suddenly exhausted?
- Yes. Sedatives, antidepressants, antihistamines, and certain blood pressure drugs can lower alertness or cause drowsiness, particularly soon after changes in dosage.
- How do doctors diagnose the cause of sudden tiredness?
- Clinicians begin with a detailed history and examination, then order targeted tests such as blood counts or thyroid panels based on clinical findings.
- Does sudden tiredness go away on its own?
- In many people, fatigue from mild illness, travel, or sleep disruption improves with rest, hydration, and restoring healthy daily routines.
- Are lifestyle habits important in preventing sudden fatigue?
- Yes. Regular sleep, balanced nutrition, hydration, and stress management help stabilize energy levels and reduce episodes of sudden tiredness.
- Who is more prone to sudden tiredness?
- Shift workers, pregnant individuals, older adults, and those with hormonal changes may experience fatigue more frequently due to circadian, metabolic, or physiological factors.