Subcutaneous Lumps in Soft Tissue Sarcoma
Subcutaneous Lumps in Soft Tissue Sarcoma: Symptoms, Risks, and Treatments
- Why Do Subcutaneous Lumps Appear in Soft Tissue Sarcoma?
- How Tumors Cause These Lumps: A Look at the Mechanism
- Prevalence of Subcutaneous Lumps in Soft Tissue Sarcoma Patients
- Statistics and Clinical Trends
- Why These Lumps Form During or After Treatment
- Warning Signs That Require Immediate Attention
- Diagnostic Tools for Subcutaneous Lumps
- How to Manage and Relieve Symptoms
- Preventive Strategies and Monitoring
- How Long Do Subcutaneous Lumps Last?
- Expert Perspectives from Oncology Clinics
- FAQ: Questions to Ask Your Oncologist
Why Do Subcutaneous Lumps Appear in Soft Tissue Sarcoma?
Subcutaneous lumps—those firm, sometimes painless masses just beneath the skin—are often the first clue in identifying soft tissue sarcoma. Unlike common benign growths like lipomas or cysts, lumps associated with sarcoma form due to malignant changes in connective tissues such as muscle, fat, or blood vessels. These cancerous growths arise when abnormal cells multiply and form a tumor, which becomes palpable as it presses outward under the skin.
These lumps may go unnoticed at first because they don’t usually cause pain. They can be mistaken for minor injuries or benign nodules until they increase in size or begin to affect surrounding nerves and tissues. In the case of soft tissue sarcoma, subcutaneous lumps are not just symptoms—they are critical diagnostic indicators that should never be overlooked.
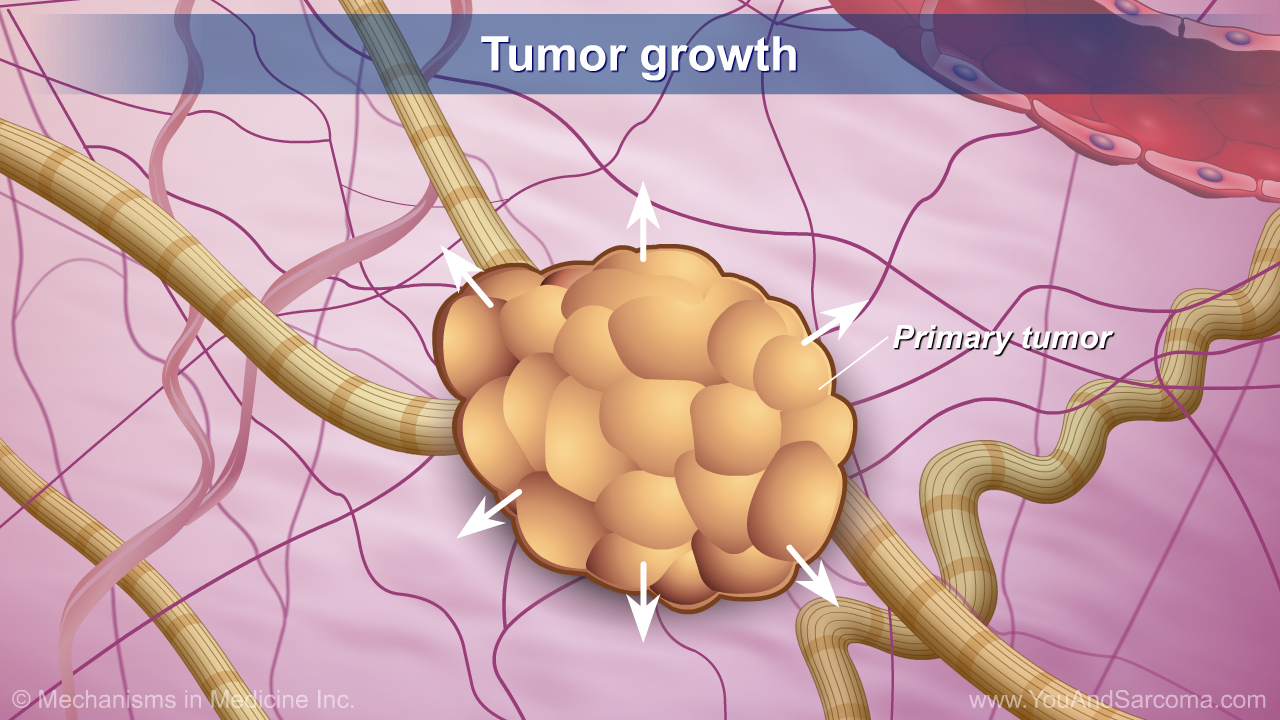
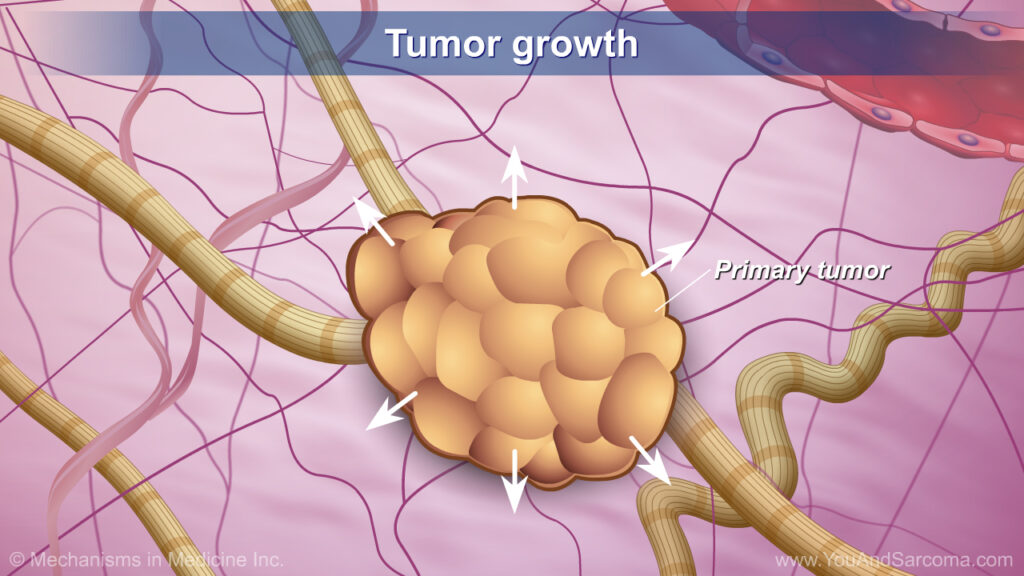
How Tumors Cause These Lumps: A Look at the Mechanism
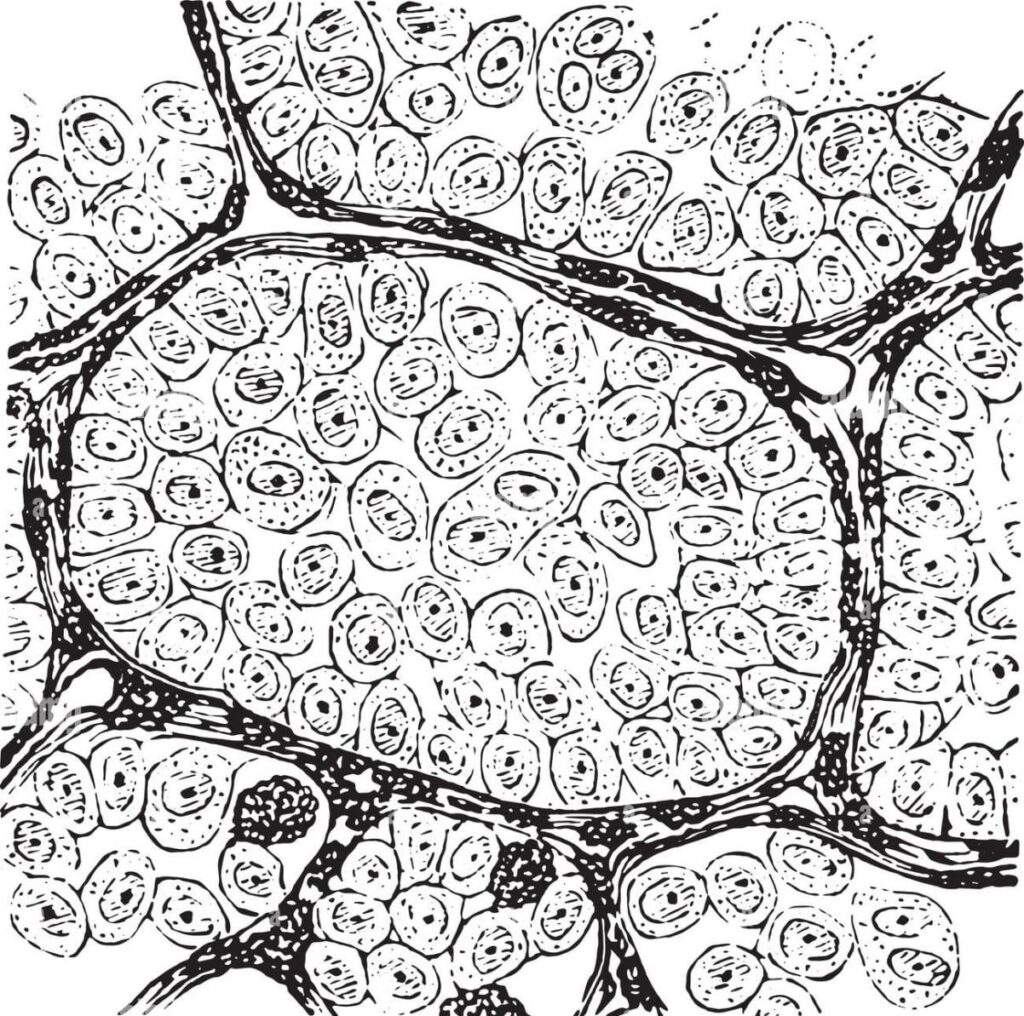
The formation of these lumps stems from genetic mutations that disrupt the normal cycle of cell growth and death. Instead of dying off, mutated cells continue to multiply, forming a solid mass within the soft tissue layer. The lump may appear fixed or mobile, depending on how deep the tumor has spread and whether it’s pressing against muscles or fascia.
Sarcoma lumps typically feel firmer than benign growths because they consist of densely packed abnormal cells. As the tumor grows, it may encroach on adjacent structures, leading to swelling, inflammation, or pressure on nerves. This biological behavior makes early imaging and biopsy essential for differentiating sarcomas from less dangerous conditions.
Prevalence of Subcutaneous Lumps in Soft Tissue Sarcoma Patients
Although soft tissue sarcomas are uncommon—accounting for less than 1% of adult cancers—most cases manifest with a visible or palpable lump. Clinical studies indicate that around 75% to 80% of patients initially seek medical attention due to noticing a lump, often without other accompanying symptoms.
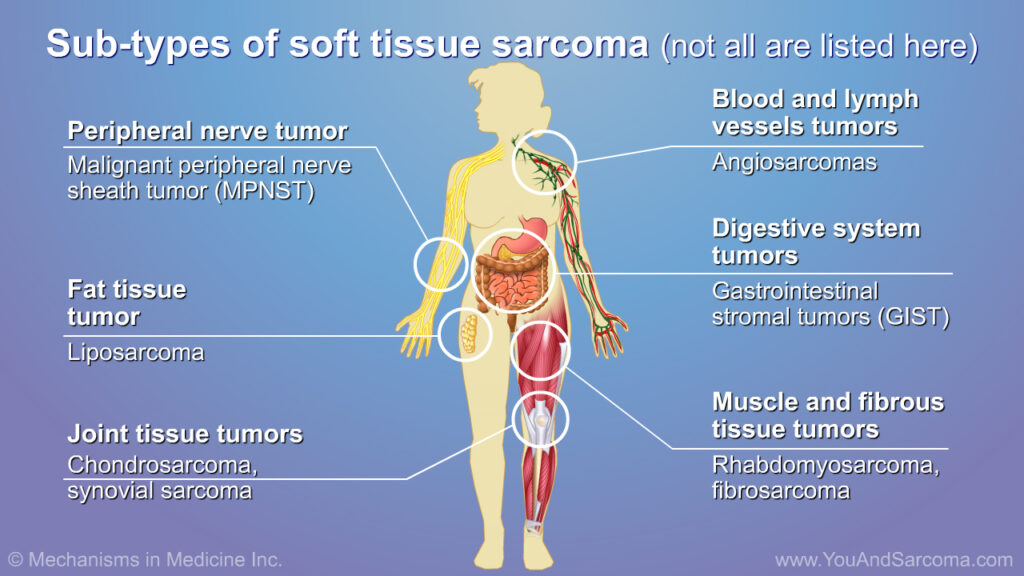
The location and depth of the lump often depend on the tumor subtype. For example, liposarcomas and fibrosarcomas frequently develop in the thigh or upper arm, making detection easier. In contrast, retroperitoneal sarcomas may remain undetected until they grow large enough to cause internal symptoms.
Statistics and Clinical Trends
| Factor | Observation |
| Common location | Thigh, upper arm, shoulder, trunk |
| Presenting with lump | 75–80% of diagnosed patients |
| Average time to seek care | 3–6 months after initial noticing |
| Age trend | More common in 40–60-year-olds |
| Associated subtypes | Liposarcoma, synovial sarcoma, leiomyosarcoma |
These statistics reveal a pattern: the earlier a lump is detected and investigated, the better the prognosis. However, lack of pain or slow growth often delays diagnosis.
Why These Lumps Form During or After Treatment
Even after the removal of a primary tumor, subcutaneous lumps may still develop. These can be due to several causes:
- Local recurrence: Cancer cells that weren’t fully removed may regrow at the original site.
- Radiation-induced fibrosis: Dense scar-like tissue may form in response to radiotherapy, mimicking a tumor.
- Surgical complications: Fluid buildup (seromas) or bleeding (hematomas) can feel like lumps.
- Metastatic spread: In aggressive cases, new malignant lumps may form elsewhere in the soft tissue.
This underscores the importance of post-treatment monitoring and distinguishing between scar tissue and tumor recurrence through imaging and biopsy.
Warning Signs That Require Immediate Attention
Recognizing red flags early can make a significant difference. These symptoms warrant urgent evaluation:
- A lump growing more than 1 cm in a month
- Increased firmness, irregular surface, or adherence to deeper tissues
- Redness, heat, or skin ulceration over the lump
- Numbness or tingling in the nearby area
- New pain or sudden loss of limb function
If any of these appear, patients should consult their oncologist immediately to rule out recurrence or secondary malignancies.
Diagnostic Tools for Subcutaneous Lumps
Proper diagnosis is achieved through a combination of clinical and imaging techniques, followed by pathological confirmation. Below is a summary of standard tools:
| Diagnostic Step | Purpose |
| Physical Exam | Checks size, texture, and mobility |
| Ultrasound | Quick assessment of superficial tissue structure |
| MRI | High-resolution scan for deep or complex lesions |
| Core Needle Biopsy | Extracts tissue for definitive pathological review |
| PET/CT Scan | Evaluates for metastasis and treatment planning |
MRI remains the preferred method for imaging due to its detailed view of soft tissues. However, only a biopsy can confirm malignancy.
How to Manage and Relieve Symptoms
Management strategies for subcutaneous sarcoma lumps depend on stage, size, and location. The cornerstone of treatment remains surgical removal with clean margins.
- Surgery: Wide excision is performed to ensure complete tumor removal.
- Radiotherapy: Used pre- or post-surgery to lower recurrence risk.
- Chemotherapy: Beneficial in high-grade or metastatic sarcomas.
- Rehabilitation: Involves physical therapy to restore limb function.
- Palliative care: Provides symptom relief in advanced stages.
Coordination among oncologists, radiologists, and surgeons ensures a comprehensive approach to care.
Preventive Strategies and Monitoring
While it’s difficult to prevent soft tissue sarcomas entirely, recurrence can often be caught early through vigilant monitoring. Prevention tips include:
- Attending all scheduled follow-up appointments
- Conducting monthly self-exams to detect new lumps
- Maintaining a healthy lifestyle to support immune response
- Reporting unusual symptoms promptly
Routine MRI or ultrasound follow-ups are commonly scheduled every 3–6 months for at least two years post-treatment.
How Long Do Subcutaneous Lumps Last?
The duration of a lump depends on its cause. Benign post-treatment lumps may resolve in weeks to months. In malignant cases, removal is necessary. Prognosis factors are summarized below:
| Prognostic Variable | Influence on Outcome |
| Tumor grade | Higher grade = greater recurrence risk |
| Surgical margin status | Clear margins improve survival |
| Response to therapy | Better response leads to longer remission |
| Stage at diagnosis | Early-stage detection improves outlook |
In patients who receive timely, aggressive treatment, the lump often resolves completely. However, lifelong monitoring is usually required.
Expert Perspectives from Oncology Clinics
Experts consistently emphasize that not all lumps are harmless, even if painless or slow-growing. Oncologists warn against waiting for discomfort before seeking care. Early evaluation through imaging and biopsy can dramatically improve outcomes.
Dr. Amina K., a surgical oncologist, states: “Don’t let absence of pain fool you. Any persistent or growing lump deserves thorough investigation. If it’s malignant, time matters.”
Doctors also remind patients that recurrence is possible, and even post-treatment lumps must be evaluated. This approach minimizes the risk of overlooking Angiosarcoma of the Breast, Axillary Lump, or other rare presentations.
FAQ: Questions to Ask Your Oncologist
1. How can I tell if a lump is cancerous or benign?
Your doctor will use imaging and biopsy to confirm this. Visual appearance alone is not reliable.
2. Can a soft tissue sarcoma lump be mistaken for a cyst?
Yes, especially in early stages. That’s why imaging and biopsy are essential.
3. Should every new lump be checked immediately?
If it’s persistent, growing, or firm—yes. Early detection matters.
4. Will the lump go away after surgery or treatment?
In many cases, yes, but monitoring is essential.
5. Is there a link between subcutaneous lumps and recurrence?
Yes. Recurrence often appears as a new lump at or near the surgical site.
6. Can exercise or massage help reduce lumps?
No, and in some cases, it may worsen the situation.
7. Does chemotherapy shrink these lumps?
In certain types, chemotherapy can help—but surgery is often still needed.
8. What’s the risk of metastasis if I ignore a lump?
It increases significantly. Delayed treatment can allow spread.
9. Can subcutaneous lumps be painful?
Sometimes—especially if nerves or vessels are involved.
10. Should I get a second opinion if told it’s benign?
Yes, especially if it’s growing. False negatives can occur.
11. How do I track changes in a lump over time?
Photograph and measure it weekly, and share with your oncologist.
12. Could this be a sign of another cancer?
Possibly. It may be related to Angiosarcoma of the Breast or even Axillary Lump in some rare cross-metastases.
13. Are there any early signs I missed?
Many patients overlook small or painless lumps—until they grow.
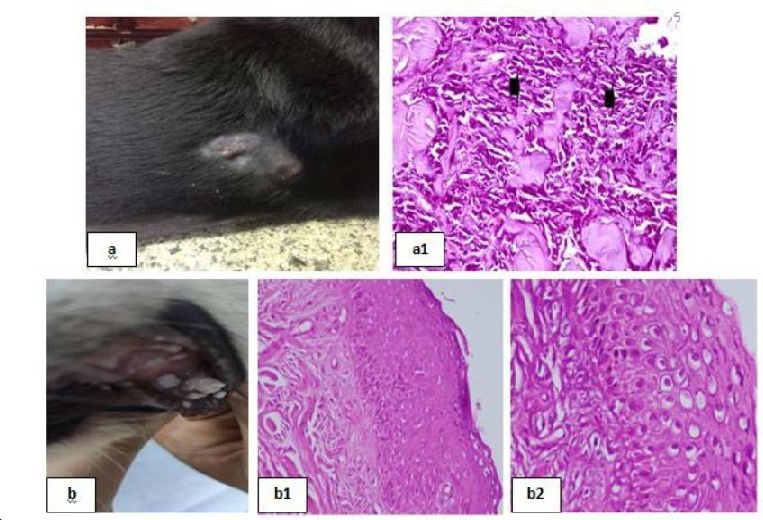
14. Can pets develop similar symptoms?
Interestingly, veterinary oncology tracks similar signs. See Lump on Toe in pets as a comparative study.
15. What should I do if the lump returns after treatment?
Return to your oncologist immediately. It may signal recurrence or metastasis.