Skin Cancer & Cosmetic Dermatology
Skin Cancer & Cosmetic Dermatology: The Full Guide
- Understanding Skin Cancer: Types and Causes
- The Role of Cosmetic Dermatology in Skin Health
- Can Cosmetic Procedures Trigger or Mask Skin Cancer?
- Identifying Cosmetic Concerns After Skin Cancer Treatment
- How Dermatologists Balance Aesthetic Goals with Cancer Safety
- Timing Cosmetic Treatments After Skin Cancer Diagnosis
- Cosmetic Risks for Patients with a History of Melanoma
- The Psychological Impact of Cosmetic Dermatology After Cancer
- Non-Invasive Options for Skin Enhancement After Cancer
- Role of Reconstructive Dermatology in Cancer Recovery
- Navigating Cosmetic Products: What to Avoid After Skin Cancer
- The Role of Annual Cosmetic Check-Ins for Survivors
- Sun Protection as the Foundation of Both Treatment and Aesthetics
- Cosmetic Dermatology for High-Risk Individuals: A Tailored Approach
- Integrating Mental Health into Skin Cancer Cosmetic Recovery
- Future Directions in Skin Cancer and Aesthetic Dermatology
- FAQ: 15 Detailed Questions About Skin Cancer and Cosmetic Dermatology
Understanding Skin Cancer: Types and Causes

Skin cancer occurs when skin cells grow uncontrollably due to DNA damage, often from ultraviolet (UV) exposure. It typically develops in areas with frequent sun exposure but can appear anywhere on the body. The three primary types are:
- Basal cell carcinoma (BCC): The most common, slow-growing, and rarely spreads. It often appears as a pearly bump or flat scar-like lesion.
- Squamous cell carcinoma (SCC): More aggressive, it can metastasize if untreated. It presents as a rough, scaly patch or open sore.
- Melanoma: The deadliest form, melanoma arises from pigment-producing melanocytes and can spread rapidly.
Other rare types include Merkel cell carcinoma and sebaceous gland carcinoma. Factors like tanning beds, fair skin, genetics, and immune suppression increase risk.
The Role of Cosmetic Dermatology in Skin Health
Cosmetic dermatology focuses on enhancing the appearance of the skin while often overlapping with medical care. Many cosmetic procedures—like chemical peels, microneedling, and laser resurfacing—require dermatological oversight to avoid exacerbating or masking underlying skin conditions, including skin cancer.
For instance, aesthetic treatments are often postponed or modified in patients with a history of cancerous lesions to avoid irritation or confusion with recurrent tumors. Dermatologists trained in both aesthetic and medical aspects can distinguish suspicious changes during cosmetic evaluations.
This integrative approach is especially beneficial for long-term skin monitoring. It also supports the removal of benign lesions that resemble cancer, thus reducing anxiety and allowing earlier detection if malignancy does occur.
Can Cosmetic Procedures Trigger or Mask Skin Cancer?
One concern among both patients and physicians is whether cosmetic treatments can hide or worsen existing skin cancer. While procedures like Botox and fillers do not directly cause cancer, certain interventions may interfere with early detection:
| Cosmetic Procedure | Risk of Masking Skin Cancer | Recommended Protocol |
| Chemical peels | Medium | Evaluate lesions beforehand |
| Laser resurfacing | High for pigmented lesions | Avoid areas with changing moles |
| Dermal fillers | Low | Monitor for abnormal swelling |
| Microneedling | Medium | Not recommended on suspect lesions |
Regular full-body skin checks are essential before and after undergoing any aesthetic treatments, particularly if you have a personal or family history of skin cancer.
Identifying Cosmetic Concerns After Skin Cancer Treatment
After surviving skin cancer, patients often face cosmetic concerns such as scarring, pigmentation changes, or uneven skin tone—especially if surgery or radiation was involved. These concerns are not just aesthetic; they impact self-esteem and quality of life.
Common post-cancer cosmetic issues include:
- Hypopigmented scars from excision.
- Hyperpigmentation after radiation.
- Atrophic or raised scars that alter facial contours.
Cosmetic dermatology offers non-invasive solutions like laser resurfacing, filler injections, or pigmentation correction to address these issues. However, all treatments should be tailored to the patient’s cancer history, location of lesions, and skin type.
Survivorship care plans often include dermatological input to address these needs. Ongoing monitoring ensures that new cosmetic symptoms don’t overshadow recurrence signs, as explained in the overview of Skin Cancer Connection.
How Dermatologists Balance Aesthetic Goals with Cancer Safety
Board-certified dermatologists trained in cosmetic and oncologic care follow rigorous protocols to balance aesthetic enhancements with patient safety. Before any cosmetic procedure, especially involving lasers or injectables, dermatologists:
- Conduct full skin evaluations.
- Review personal and family cancer history.
- Avoid active or healing cancer sites.
- Schedule follow-up checks for evolving skin lesions.
If you’ve had prior basal or squamous cell carcinoma, dermatologists will often avoid cosmetic procedures on the same area or delay them until the skin has completely healed and stabilized. They may also recommend less invasive approaches or refer patients for medical clearance.
What sets cosmetic dermatology apart is its medical foundation—it does not just pursue beauty, but integrates risk awareness and safe practice. That’s especially critical for patients with previous malignancies.
Timing Cosmetic Treatments After Skin Cancer Diagnosis
If you’ve been treated for skin cancer, the question often arises: When is it safe to resume cosmetic dermatology? Timing depends on cancer type, treatment method, and location:
| Cancer Type | Time to Wait Before Cosmetic Treatment |
| Basal Cell Carcinoma | 3–6 months (after complete healing) |
| Squamous Cell Carcinoma | 6–12 months (with regular derm follow-up) |
| Melanoma | At least 12–24 months, depending on stage |
Surgical excisions require full wound remodeling before any resurfacing or pigmentation correction. Radiation-treated areas might take longer due to skin sensitivity and increased risk of complications.
In some cases, cosmetic dermatology becomes part of the rehabilitation process—but only when oncologic clearance is obtained, and the patient is emotionally and physically ready.
Cosmetic Risks for Patients with a History of Melanoma
Melanoma is particularly aggressive and prone to recurrence, which adds caution when considering cosmetic procedures. Treatments that involve trauma to the skin, such as deep peels or ablative lasers, may cause inflammation or mask symptoms.
Here are common concerns:
- Delayed detection: Cosmetic procedures may temporarily obscure evolving pigmented lesions.
- Inflammation: Healing responses can resemble malignancy.
- False reassurance: Patients may believe enhanced skin = healthy skin, delaying real evaluation.
As a result, dermatologists often limit elective cosmetic procedures near previous melanoma sites and prioritize surveillance. Treatments like LED therapy or microcurrent facials, which don’t disturb deep skin layers, may be preferred.
This approach ensures that aesthetic goals do not override cancer vigilance, especially in high-risk individuals.
The Psychological Impact of Cosmetic Dermatology After Cancer
Surviving skin cancer changes the relationship many patients have with their appearance. Scars, discoloration, and fear of recurrence can impact mental health. Cosmetic dermatology plays a therapeutic role in restoring confidence—but it must be done thoughtfully.
Patients often report:
- Increased self-esteem after scar improvement.
- Relief from hyperpigmentation or textural irregularities.
- Greater willingness to re-engage socially.
However, unrealistic expectations or aggressive cosmetic agendas can cause more harm than good. That’s why experienced dermatologists balance patient hopes with what is medically responsible.
Aesthetic care after cancer isn’t superficial—it’s part of holistic recovery.
In some patients with prior malignancy, underlying skin inflammation or pigmentation can also resemble signs of dangerous skin cancer. Evaluating such changes requires careful diagnostic distinction.
Non-Invasive Options for Skin Enhancement After Cancer
For patients with a history of skin cancer, non-invasive cosmetic procedures are often the safest route. These methods can address concerns such as redness, texture, fine lines, and discoloration without compromising the skin’s health.
Common non-invasive treatments include:
- Intense Pulsed Light (IPL): Helps with pigmentation issues and redness post-surgery or sun damage.
- Microdermabrasion: Light exfoliation to improve texture, suitable even for fragile skin.
- Topical Retinoids and Niacinamide: Proven to improve skin appearance and potentially reduce precancerous lesions.
Niacinamide, in particular, has gained attention for its protective role in skin health. It may not only improve skin tone but also help reduce recurrence of non-melanoma skin cancers. We’ll explore this further in a separate section, especially for patients with basal cell skin cancer or prior sun damage.
When designing a treatment plan, dermatologists often combine non-invasive tools with sun protection counseling and regular check-ups.
Role of Reconstructive Dermatology in Cancer Recovery
Sometimes, the journey through skin cancer involves significant surgical removal, leaving behind scars or tissue loss. Reconstructive dermatology steps in here—not only for appearance but also for function.
Techniques used include:
- Flap Surgery: Skin is moved from an adjacent area to cover a defect.
- Skin Grafting: Skin from another part of the body is transplanted to repair a surgical site.
- Laser Scar Revision: Resurfaces the top layer to smooth out raised scars.
Advanced cosmetic-reconstructive integration can even restore natural contours in areas like the nose, cheek, or eyelid. This can be a transformative experience for patients who struggled with visibility of surgical results.
Dermatologists trained in both oncology and aesthetics are crucial here, offering a balance of safety and skill.
Navigating Cosmetic Products: What to Avoid After Skin Cancer
Skin cancer survivors are often more cautious about the products they apply daily. Some ingredients may irritate sensitive skin, while others are debated for their hormonal or inflammatory effects.
Here’s a simplified table of what to avoid and what to consider:
| Avoid These | Better Alternatives |
| Parabens (possible endocrine links) | Preservative-free products |
| Oxybenzone (in some sunscreens) | Zinc oxide or titanium dioxide SPF |
| Strong fragrances | Hypoallergenic, fragrance-free |
| Harsh retinoids (post-treatment) | Low-dose or encapsulated retinoids |
Products should be reviewed with your dermatologist, especially if you’ve had radiation or chemotherapy to the skin. Additionally, any persistent redness or new texture should not be self-treated—it might mimic early symptoms of squamous cell skin cancer.
The Role of Annual Cosmetic Check-Ins for Survivors
Even if you’re not pursuing active cosmetic treatments, dermatologists recommend yearly aesthetic-focused check-ins for those with a history of skin cancer. These visits go beyond mole mapping:
- Assess skin healing from past surgeries.
- Discuss concerns like dryness, discoloration, and texture.
- Evaluate suitability for gentle cosmetic interventions.
What makes these sessions valuable is that they blend surveillance with rejuvenation. Patients get medical reassurance while also learning how to safely care for their skin’s appearance.
Importantly, these appointments also help spot subtle changes early, especially in cosmetically treated areas. If a rash or lesion evolves post-filler or resurfacing, it could be an early warning sign—particularly in the context of skin cancer connection conditions.
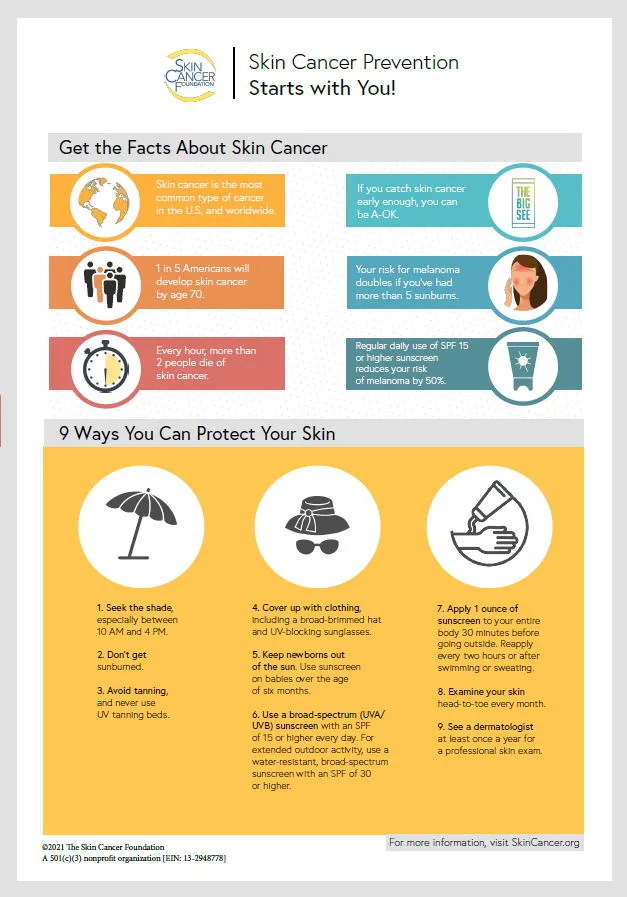
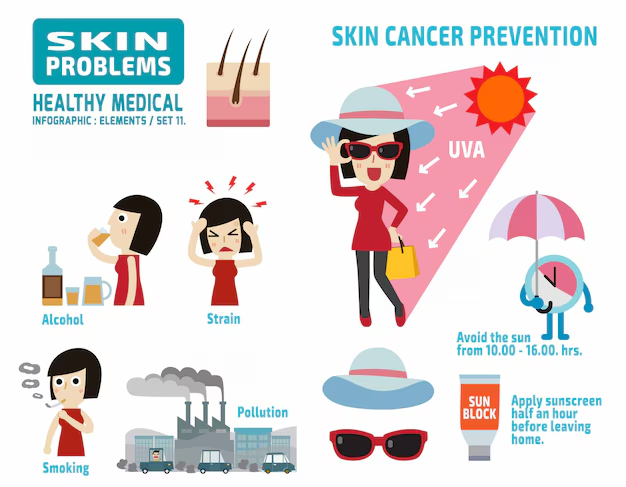
Sun Protection as the Foundation of Both Treatment and Aesthetics
UV exposure is the top preventable risk factor for most skin cancers—and it’s also the biggest accelerator of skin aging. That’s why in cosmetic dermatology, sun protection is more than a recommendation; it’s a cornerstone.
Dermatologists emphasize:
- Daily use of broad-spectrum SPF 30+.
- Preference for physical blockers like zinc oxide, especially in sensitive or previously treated skin.
- Protective clothing and wide-brimmed hats as adjuncts.
- Caution with post-procedure exposure: for instance, laser-treated areas should be kept entirely sun-free for weeks.
One of the key messages to skin cancer survivors is that investing in good sun protection equals investing in long-term cosmetic outcomes. Post-repair pigmentation, vascular changes, and fine lines are far less likely to return in patients who follow proper UV defense protocols.
Cosmetic Dermatology for High-Risk Individuals: A Tailored Approach
Not all cosmetic options are safe for everyone. Individuals with a strong personal or family history of melanoma or non-melanoma skin cancers need customized plans.
In such patients, dermatologists may:
- Avoid deep ablative lasers that increase inflammation.
- Opt for topical brighteners instead of chemical peels.
- Carefully time interventions around cancer check-ups.
- Prefer dermatologist-prescribed products over med-spa offerings.
Patients with genetic predispositions or those who have undergone radiation therapy may also present with fragile skin that reacts unpredictably to standard procedures. In these cases, cautious stepwise treatments are preferred.
This individualized strategy protects both skin health and long-term cosmetic integrity—especially important when managing skin without a rash concerns that may signal underlying damage.
Integrating Mental Health into Skin Cancer Cosmetic Recovery
The psychological aspect of skin cancer, especially when disfigurement or facial involvement occurs, cannot be overstated. Cosmetic recovery isn’t just about surface changes—it’s part of emotional healing.
Key elements of support:
- Offering visual rehabilitation plans, so patients feel involved in their recovery journey.
- Encouraging dermatologic visits as self-care, not vanity.
- Recognizing that restored appearance can reduce cancer-related PTSD.
Cosmetic interventions post-cancer can significantly boost quality of life, reduce anxiety, and improve social engagement. Dermatologists increasingly collaborate with mental health professionals to ensure recovery is both physical and emotional.
Future Directions in Skin Cancer and Aesthetic Dermatology
Research is advancing in merging oncology with aesthetics. Promising areas include:
- Smart topical treatments that both improve appearance and prevent actinic keratosis.
- Bioengineered skin grafts that closely mimic native texture and tone.
- AI-guided dermoscopy that blends cosmetic planning with cancer detection.
Clinical trials are also exploring how certain cosmetic agents might slow or reverse precancerous skin changes. This means the boundary between cancer prevention and aesthetic improvement is narrowing, offering new hope.
The evolution of this field continues to be driven by the need to heal holistically—where patients don’t have to choose between health and appearance but can pursue both safely.
FAQ: 15 Detailed Questions About Skin Cancer and Cosmetic Dermatology
1. Can I get Botox if I’ve had skin cancer on my face?
Yes, but only after clearance from your dermatologist. Botox is non-invasive and generally safe when injected away from previous cancer sites. It should not be done over active lesions or in areas with healing grafts.
2. Do cosmetic lasers increase my risk of skin cancer recurrence?
Most modern lasers are considered safe if used correctly. However, aggressive ablative lasers may not be suitable for skin that has undergone radiation or surgery. Always consult a board-certified dermatologist.
3. Is niacinamide really effective in preventing skin cancer recurrence?
Clinical studies support its role, especially in reducing the occurrence of actinic keratosis and basal cell carcinoma. It’s not a treatment, but a preventative tool when taken under guidance.
4. Can cosmetic tattoos hide skin cancer signs?
Yes, and that’s risky. Tattoo ink can obscure early signs of skin cancer or cause inflammation. Cosmetic tattooing should be avoided over areas of prior cancer or scars.
5. Are hyaluronic acid fillers safe after cancer surgery?
In most cases, yes—especially when injected by a dermatologist. Fillers are temporary and biocompatible, but must not be placed into or near scar tissue that’s still healing.
6. Can skincare products cause skin cancer?
There’s no conclusive evidence linking topical products to cancer. However, some ingredients (like coal tar or formaldehyde) have raised concerns. Always choose products rated safe by dermatologists.
7. What cosmetic procedures help with post-surgical scars?
Microneedling, silicone gel sheeting, fractional lasers, and vascular lasers are common. Each works differently depending on scar type and skin tone.
8. Should I avoid sunscreen if I had a reaction during cancer treatment?
No. You should switch to mineral sunscreens (zinc or titanium-based) that are less likely to irritate sensitive skin. SPF is essential even during treatment.
9. How soon after skin cancer surgery can I consider cosmetic treatments?
Typically after 3 to 6 months, once the area is fully healed and no recurrence is noted. However, timing is individualized.
10. Can cosmetic procedures trigger cancer growth?
There is no evidence that cosmetic treatments cause cancer to return. Still, inflammation and trauma should be minimized in previously treated areas.
11. Is laser hair removal safe for skin cancer survivors?
Yes, but avoid treating over or near previous cancer sites. Areas with suspicious moles should never be lasered.
12. Can I use retinol products after skin cancer?
Low-dose retinol may be safe, but only under professional supervision. Retinoids can be irritating and should be introduced gradually.
13. Do vitamin C serums help prevent skin cancer?
Vitamin C offers antioxidant protection and may reduce damage from free radicals. It’s supportive, but not a substitute for sunscreen or regular screening.
14. Is cosmetic surgery allowed after Mohs surgery?
Yes, many patients undergo aesthetic refinements. The timing and approach depend on scar healing, cancer clearance, and patient goals.
15. Should cosmetic treatments be stopped during skin cancer treatment?
In most cases, yes. Focus on healing and medical therapy first. Once stable, you can resume aesthetic care under dermatologist guidance.












