Shoulder Pain from Bone Metastases
Shoulder Pain from Bone Metastases: Causes, Diagnosis, and Relief
- Why Shoulder Pain Can Develop in Cancer Patients with Bone Metastases
- How Bone Metastases Cause Pain in the Shoulder Region
- How Common Is Shoulder Pain from Bone Metastases?
- What Causes Shoulder Pain in Cancer Patients with Bone Metastases?
- When to Be Concerned About Shoulder Pain
- How Shoulder Pain from Bone Metastases Is Diagnosed
- Treatment and Symptom Relief Options
- Can This Type of Pain Be Prevented?
- Does the Pain Go Away — And When?
- Clinical Perspectives: What Oncologists Say About This Pain
- Questions to Ask Your Doctor
- FAQ: Shoulder Pain from Bone Metastases
Why Shoulder Pain Can Develop in Cancer Patients with Bone Metastases
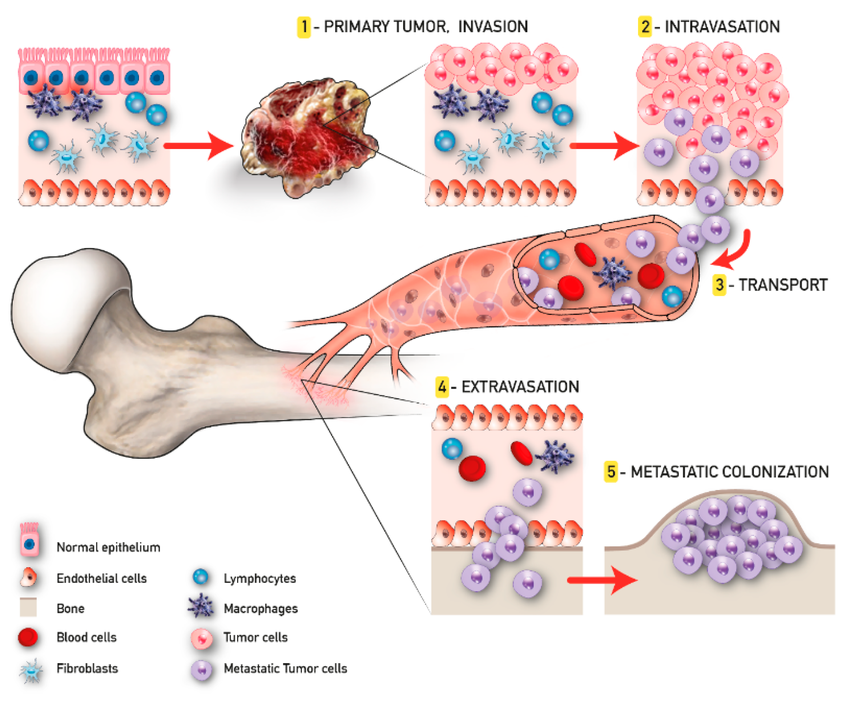
Shoulder pain in individuals diagnosed with cancer is more than just a musculoskeletal discomfort—it may be a manifestation of metastatic spread, particularly to the bones. When cancer cells from a primary tumor migrate to the bones (a process known as metastases), they can settle in areas like the humerus or scapula, which make up the shoulder joint. This often results in a deep, aching pain that may worsen at night or with movement.
In women with breast cancer, this type of pain can sometimes be mistaken for rotator cuff injuries or arthritis, delaying the appropriate oncologic intervention. The pain may feel dull and constant or sharp during motion, depending on the location and aggressiveness of the lesion.
In some cases, shoulder pain can also be the first sign of distant cancer spread, especially in patients who previously had successful treatment. Because of its non-specific nature, early evaluation by a specialist is essential.
How Bone Metastases Cause Pain in the Shoulder Region
The shoulder is a complex joint made of bones, muscles, and tendons, but when cancer spreads to the skeletal system, it alters the bone structure itself. Bone metastases typically weaken the affected bone through a process called osteolysis, in which cancer cells stimulate bone resorption. This structural degradation irritates local nerves, stretches the periosteum (bone lining), and sometimes even leads to fractures.
In the shoulder, metastatic lesions may form in the proximal humerus (upper arm bone), clavicle, or scapula. These bones are richly innervated, so even small lesions can trigger intense, unrelenting pain. Moreover, tumor-related inflammation and compression of adjacent soft tissues—muscles, nerves, and bursae—contribute to both pain and limited range of motion.
The involvement of nearby neurovascular structures may also lead to secondary symptoms such as tingling or numbness in the arm, mimicking neurological conditions. For many patients, understanding that bone cancer isn’t limited to primary tumors—but often represents metastatic disease—is key to addressing this pain comprehensively.
How Common Is Shoulder Pain from Bone Metastases?
Shoulder pain due to bone metastases is not uncommon, especially in patients with advanced-stage cancers. Breast, lung, prostate, kidney, and thyroid cancers are among the most likely to spread to the bones. Within this subset, the shoulder area—though not as commonly affected as the spine or pelvis—still represents a notable percentage.
Frequency of Bone Metastases Involving the Shoulder in Selected Cancers
| Cancer Type | Bone Metastases Incidence | Shoulder Involvement (Approx.) |
| Breast Cancer | Up to 70% in stage IV | ~10–15% |
| Lung Cancer | ~30–40% | ~5–10% |
| Prostate Cancer | Over 85% in advanced stage | ~7–12% |
| Renal Cell Carcinoma | ~35% | ~5% |
| Thyroid Cancer | ~60% | ~5–8% |
These numbers reflect clinical trends, but real-world presentation varies by tumor biology, treatment status, and genetic factors. The longer a person lives with metastatic disease, the higher the cumulative risk for painful skeletal involvement.
What Causes Shoulder Pain in Cancer Patients with Bone Metastases?
Pain in the shoulder linked to metastatic disease arises from several overlapping causes—some related directly to the tumor and others to the consequences of treatment or systemic dysfunction.
Major Contributing Factors
| Cause Type | Examples and Mechanism |
| Oncologic | Tumor invasion into bone, soft tissue compression, periosteal stretching |
| Therapy-Induced | Radiation-induced tissue fibrosis, chemotherapy-induced neuropathy |
| Metabolic | Cancer-related hypercalcemia leading to bone fragility |
| Mechanical | Pathological fractures, joint instability due to lytic lesions |
| Inflammatory | Tumor cytokines triggering local inflammation in joint capsule |
Importantly, metastatic shoulder pain may be compounded by muscle atrophy and joint disuse. For patients undergoing immunotherapy or targeted therapy, atypical inflammation can also mimic arthritis or bursitis, complicating the clinical picture.
In all scenarios, precise diagnosis helps to tailor pain management strategies and prevent complications such as fracture or nerve entrapment.
When to Be Concerned About Shoulder Pain
Not all shoulder pain in cancer patients is immediately alarming, but there are specific red flags that should prompt urgent medical attention. Pain that is constant, worsens at night, and doesn’t respond to over-the-counter medications may indicate metastatic involvement. This is especially true if the pain is localized to the upper arm or shoulder blade and accompanied by swelling or reduced mobility.
Other warning signs include visible deformity, sudden loss of strength, or a cracking sensation—possible signs of an impending or actual pathological fracture. If neurological symptoms appear—like numbness, tingling, or shooting pain into the fingers—this may suggest compression of the brachial plexus or spinal involvement.
Patients who already have known bone metastases should alert their oncologist to any new or changing shoulder pain. Likewise, individuals in remission who experience persistent shoulder discomfort should be evaluated for recurrence or progression.
In any case, unexplained shoulder pain in someone with a history of cancer should never be ignored. Early intervention can prevent severe complications and improve quality of life.
How Shoulder Pain from Bone Metastases Is Diagnosed

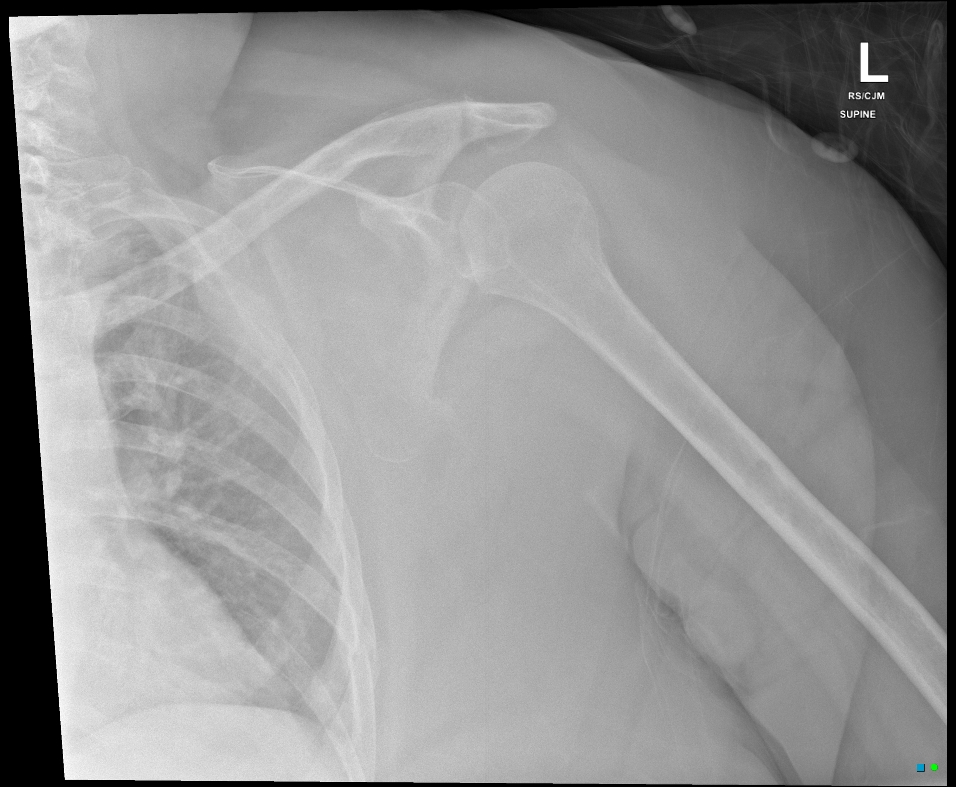
Diagnosis begins with a thorough clinical history and physical examination. Oncologists look for pain patterns, range of motion limitations, and signs of localized tenderness or swelling. The next step typically involves imaging studies, which help confirm whether the pain is due to bone cancer metastasis or another cause.
Common Diagnostic Tools for Shoulder Metastases
| Diagnostic Tool | Purpose |
| X-ray | Initial assessment of bone structure, fractures, lytic lesions |
| MRI | Detailed view of bone marrow, soft tissues, nerve involvement |
| CT Scan | Precise anatomical mapping, often for surgical planning |
| PET-CT | Detects metabolically active tumors across the body |
| Bone Scan | Highlights areas of increased bone turnover from metastases |
| Biopsy | Confirms cancer type if diagnosis is unclear or new |
In some cases, blood tests are also used to detect tumor markers or elevated calcium levels, which may indicate extensive bone involvement.
A key part of diagnosis is distinguishing metastatic pain from degenerative or inflammatory shoulder conditions, which are common in the general population. Cancer-related pain often has a different character—more constant, less responsive to rest, and more likely to disrupt sleep.
Treatment and Symptom Relief Options
Relieving shoulder pain from bone metastases involves a multi-modal strategy tailored to the individual’s cancer status, location of the lesions, and pain severity. The goal is not only to control the pain but also to stabilize the affected bone and improve function.
Key Approaches to Management
| Treatment Type | Examples and Details |
| Pharmacologic | Opioids, NSAIDs, corticosteroids, bone-modifying agents (bisphosphonates or denosumab) |
| Radiation Therapy | Localized radiation to reduce tumor size and inflammation |
| Surgery | Stabilization with rods or plates if fracture risk is high |
| Physiotherapy | Gentle exercises to preserve mobility and reduce stiffness |
| Systemic Therapy | Chemotherapy, hormonal therapy, immunotherapy to control underlying disease |
| Specialist Referral | Pain management teams, orthopedic oncology, palliative care |
The use of bisphosphonates or denosumab is particularly helpful in reducing bone resorption and minimizing fracture risk. Pain often improves within weeks after targeted radiation, though full relief can take longer.
Physiotherapists play a crucial role in regaining shoulder movement after bone stabilization or radiation. However, rehabilitation must be carefully paced to avoid exacerbating pain or causing structural damage.
Can This Type of Pain Be Prevented?
Preventing shoulder pain caused by bone metastases is not always possible, but proactive monitoring and preventive strategies can reduce its impact. Early detection of skeletal involvement allows for timely intervention before the pain becomes debilitating.
Patients with cancers known to spread to bone—especially metastases from breast, prostate, or lung—may be prescribed bone-strengthening agents early in their treatment course. These drugs help reduce the likelihood of skeletal-related events such as fractures and severe pain.
Maintaining physical activity within comfort limits also helps preserve joint function and muscular support around the shoulder. Good nutrition, calcium and vitamin D supplementation, and routine bone scans for high-risk patients all contribute to proactive care.
Importantly, adherence to cancer treatment protocols, including systemic therapies and regular imaging, remains the most effective prevention against bone-related complications.
Does the Pain Go Away — And When?

The course of shoulder pain caused by bone metastases depends largely on the underlying cancer type, treatment response, and whether the skeletal lesion has caused structural damage. For some patients, especially those with responsive tumors and effective systemic therapy, the pain may lessen significantly or resolve altogether after treatment.
Radiation therapy often leads to measurable pain relief within two to four weeks. If bisphosphonates or denosumab are used consistently, they may help reduce future flare-ups. However, in cases where bone destruction is advanced or structural integrity is compromised, the pain may persist or recur intermittently.
In patients with long-standing or progressive disease, shoulder pain may become a chronic symptom requiring ongoing management. Yet, in others, especially those diagnosed and treated early, it can be a temporary issue.
Ultimately, whether shoulder pain disappears or persists varies: for some, it resolves post-treatment; for others, it’s a life-long symptom managed through supportive care.
Clinical Perspectives: What Oncologists Say About This Pain
According to practicing oncologists and orthopedic cancer specialists, shoulder pain from bone metastases is a serious but manageable issue when addressed promptly. They emphasize the importance of patient-reported symptoms, which often precede imaging confirmation of bone spread.
Clinicians point out that patients frequently mistake metastatic shoulder pain for overuse injuries or arthritis. Because of this, many are diagnosed late—after the lesion has progressed significantly. Timely imaging and detailed history-taking are therefore essential components of care.
Doctors also stress the value of integrated treatment: combining systemic cancer control, local therapies (like radiation), and supportive measures like physiotherapy. Palliative care teams can offer targeted pain relief strategies, even for patients with advanced, non-curable disease.
Ultimately, the medical consensus is clear: shoulder pain in cancer patients should never be dismissed—it is often a window into deeper skeletal complications that can and should be addressed early.
Questions to Ask Your Doctor
| Suggested Questions for Your Doctor | Purpose |
| What is causing my shoulder pain — could it be bone metastases? | Clarify the source of your symptoms |
| Which imaging tests will best confirm the diagnosis? | Understand diagnostic steps |
| Is there a fracture risk? Should I limit movement? | Prevent injury from weakened bone |
| Could this pain be from treatment side effects? | Differentiate between causes |
| What are my treatment options for the pain? | Explore relief strategies |
| Will radiation or surgery help in my case? | Assess suitability of local treatments |
| Should I take bone-strengthening medications? | Prevent future deterioration |
| Can physical therapy help or make it worse? | Clarify rehab safety |
| How soon can I expect relief? | Set realistic expectations |
| Is this pain likely to return or worsen? | Plan for the long term |
| Are there signs I should watch for urgently? | Recognize complications early |
| Can I still exercise or lift with this arm? | Get safe activity guidelines |
| How will this pain affect my cancer treatment? | Ensure holistic management |
| Should I see a pain specialist or palliative care? | Consider referrals |
| What can I do at home to help with this pain? | Encourage self-care and monitoring |
These questions empower both patients and caregivers to advocate for appropriate, timely interventions.
FAQ: Shoulder Pain from Bone Metastases
1. Can shoulder pain be the first sign of cancer?
Yes, in some cases, persistent unexplained shoulder pain may be the first clue to metastatic spread, especially from breast, lung, or prostate cancer.
2. Is this type of pain always linked to advanced cancer?
Not necessarily. Bone metastases may occur even when the primary cancer is still under control, especially in cancers prone to skeletal spread.
3. What does the pain usually feel like?
The pain is typically deep, aching, constant, and may worsen at night or with arm movement.
4. Will imaging always show bone metastases right away?
Not always. Early lesions may not appear on plain X-rays. MRI, PET-CT, or bone scans offer higher sensitivity.
5. How soon does radiation reduce pain?
Patients often begin to feel relief within 2–4 weeks after radiation therapy to the shoulder.
6. Is surgery common for shoulder bone metastases?
Surgery is usually reserved for cases with high fracture risk or when the pain is unmanageable by other means.
7. Can physical therapy help?
Yes, when guided by a specialist. It helps restore mobility and prevent stiffness but must be gentle to avoid fracture.
8. Are opioids always needed for this pain?
Not always. Pain levels vary, and some patients respond well to NSAIDs or bone-targeting drugs.
9. How do bisphosphonates work in this case?
They slow down bone resorption and reduce skeletal pain and fracture risk in metastatic disease.
10. Will this pain ever fully go away?
It can, especially if treatment is effective and bone stability is restored. In some, it remains chronic but manageable.
11. Does pain mean my cancer is worsening?
Not always. It could be from past damage or treatment side effects. Still, worsening pain should always be reported.
12. Can shoulder pain come from chemotherapy?
Yes, especially if it causes nerve inflammation or indirectly weakens bones.
13. Is this pain dangerous?
It can indicate underlying bone weakening or a fracture risk, so it should be taken seriously.
14. Should I stop using my arm altogether?
No, but you should limit high-impact activities and follow your doctor’s guidelines to avoid injury.
15. Is palliative care only for terminal cases?
No. Palliative care supports quality of life at any stage, including managing pain from bone cancer.












