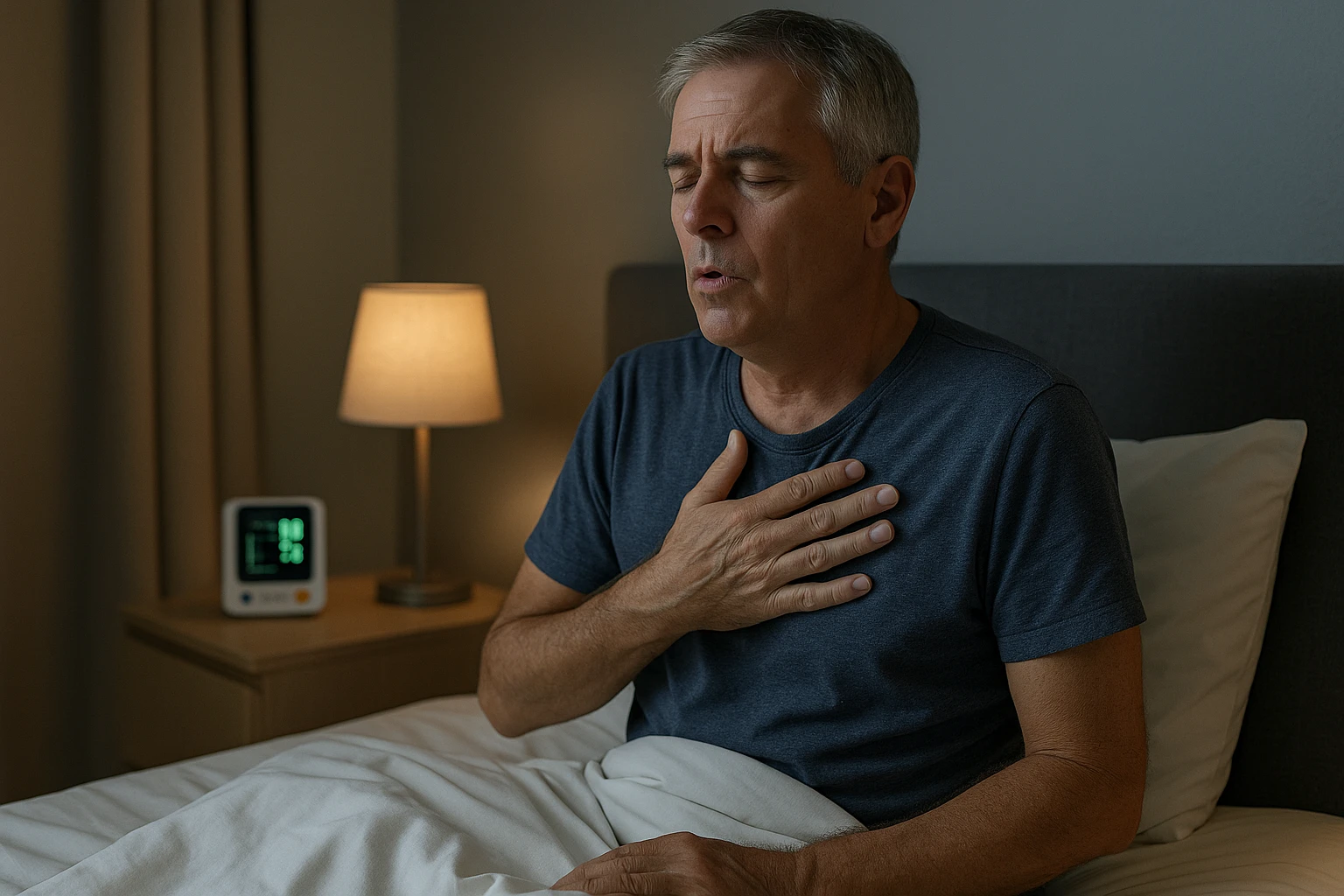
Shortness of Breath While Sleeping: Why It Happens and Relief Options
Shortness of Breath at Night
Shortness of breath at night can be unsettling and may indicate an underlying health condition. Many people describe waking up gasping for air or feeling unable to take a full breath while lying down. Although occasional breathlessness may seem harmless, persistent symptoms at night often point to heart or lung problems. Recognizing these patterns is the first step toward understanding their cause and seeking appropriate medical care.
Why this symptom matters
When breathing becomes difficult at night, it can reflect more than fatigue or poor sleep. The body’s normal breathing pattern changes during rest, and lying flat can make it harder for the lungs to expand fully. In people with heart or lung disorders, this position increases pressure in the chest and makes breathing feel labored. Because of this, nighttime breathlessness often signals that the heart or lungs are under strain and may need medical attention.
- Heart or lung strain can cause nighttime breathlessness.
- Lying flat increases chest pressure, making breathing more difficult.
- Tracking the timing and position of symptoms helps identify underlying causes.
Identifying the pattern and timing of these symptoms helps doctors determine whether the cause is cardiac, respiratory, or another condition affecting breathing.
Recognizing orthopnea and paroxysmal nocturnal dyspnea (PND)
Doctors use specific terms to describe different types of shortness of breath at night. Orthopnea refers to difficulty breathing when lying flat that improves quickly after sitting or standing up. People who experience orthopnea may notice they sleep better with extra pillows or in a reclined position. This happens because sitting upright reduces pressure on the lungs and allows air to move more freely.
Paroxysmal nocturnal dyspnea (PND) describes sudden episodes of breathlessness that occur during sleep, often a few hours after lying down. The sensation may be intense enough to awaken someone from sleep, leaving them short of breath until they sit up. PND can be distressing, but recognizing it as a known medical symptom helps individuals understand that it signals disrupted fluid balance or airflow, often related to heart or lung conditions.
| Feature | Orthopnea | Paroxysmal Nocturnal Dyspnea (PND) |
|---|---|---|
| Timing | Occurs immediately when lying flat | Occurs a few hours after falling asleep |
| Relief | Improves quickly when sitting or standing up | Improves gradually after sitting up or standing |
| Common causes | Often linked to heart or lung strain | Commonly associated with heart failure |
What Happens in the Body During Nighttime Breathlessness
Shortness of breath at night often stems from internal changes that occur when a person lies down. Understanding these shifts helps explain why breathing feels easier in certain positions and more difficult in others, especially for those with heart or lung conditions.
Fluid and pressure shifts
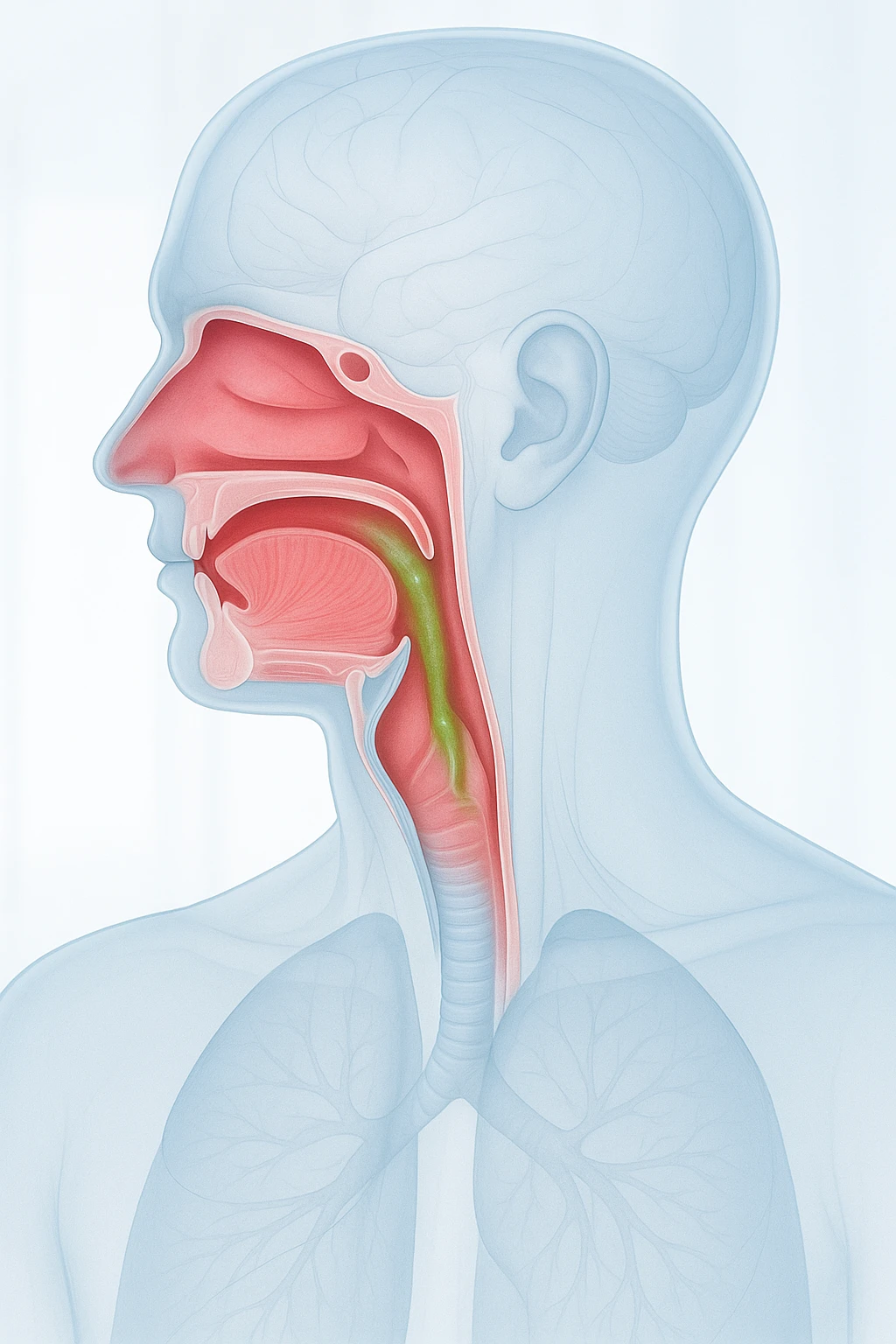
When the body is in a lying or supine position, gravity no longer keeps fluid distributed evenly in the lower limbs. Venous blood returns more freely to the chest, increasing pressure within the pulmonary circulation. The small blood vessels in the lungs fill more fully, raising pulmonary pressure and reducing the lungs’ ability to expand-a condition called reduced lung compliance. This change can make each breath feel more effortful, particularly for people whose hearts already struggle to pump blood efficiently.
- Lying flat increases venous return to the chest.
- Pulmonary pressures rise as lung vessels fill with blood.
- Lung compliance decreases, making breathing more difficult.
- Pulmonary congestion occurs as fluid leaks into lung tissue.
As pressure rises, small amounts of fluid may move from blood vessels into lung tissue-a process called pulmonary congestion. This narrows the air spaces and heightens breathlessness. For individuals with heart failure, these effects are more pronounced because the weakened heart cannot effectively handle the increased blood returning from the body.
Why it worsens during sleep
During sleep, the body’s natural rhythms further influence breathing. Muscle relaxation and a slower breathing rate make it harder to compensate for rising lung pressure. Meanwhile, fluid redistribution continues, adding to chest congestion. This combination of physiological factors can trigger tightness or air hunger that awakens a person after a few hours of rest.
This interaction between posture, circulation, and lung mechanics explains why nighttime breathlessness is closely tied to conditions that affect heart function and fluid balance.
Causes and Risk Factors for Shortness of Breath at Night
Shortness of breath that occurs at night can result from several medical conditions, most of which affect the heart, lungs, or breathing patterns during sleep. Understanding these causes helps clarify why symptoms occur and who may be at higher risk.
Heart-related causes
Heart failure is one of the most common causes of shortness of breath at night. When the heart’s pumping ability is reduced, blood returning to the heart can back up into the lungs. Lying flat increases venous return from the lower body, which raises pulmonary pressure and can lead to fluid seeping into lung tissue, known as pulmonary congestion. This buildup makes it harder for the lungs to expand and for oxygen to move into the bloodstream.
- Heart failure causes fluid buildup in the lungs when lying flat.
- Pulmonary congestion reduces lung expansion and oxygen exchange.
- Orthopnea and PND are characteristic nighttime symptoms of heart failure.
Lung and airway conditions
Respiratory conditions such as COPD and asthma can worsen at night. These diseases cause inflammation and narrowing of the airways, which may intensify during rest. For some individuals, changes in body position or nighttime temperature can cause additional airway constriction. Because the lungs are already under strain, even minor fluctuations in airway resistance or oxygen levels can cause noticeable breathlessness.
- COPD and asthma cause airway inflammation and narrowing.
- Symptoms may worsen due to position or temperature changes.
- COPD rarely produces sudden awakenings, distinguishing it from PND.
Other contributing factors
Not all nighttime breathlessness is due to heart or lung disease. Sleep apnea, where breathing repeatedly stops and starts during sleep, can cause oxygen drops that awaken a person gasping for air. Anxiety or panic episodes may also create sensations of tightness or air hunger. In some people, excess body weight or reflux increases pressure on the diaphragm when lying flat, worsening breathing difficulty.
- Sleep apnea causes breathing pauses and oxygen drops during sleep.
- Anxiety and panic can cause chest tightness or air hunger.
- Obesity or reflux increases pressure on the diaphragm when lying down.
Red flags
- Sudden awakening gasping for air
- Chest discomfort or tightness
- Severe shortness of breath that does not improve when sitting up
Seek immediate medical attention if you experience any of these warning signs, as they may indicate an urgent cardiac or respiratory condition requiring prompt evaluation.
How Doctors Diagnose Shortness of Breath at Night
When shortness of breath at night occurs, doctors use a structured approach to determine the cause. Diagnosis begins with a detailed conversation about symptoms and continues through physical examination and targeted tests.
Clinical evaluation
The diagnostic process starts with a comprehensive medical history. Healthcare providers ask when symptoms appear-whether immediately after lying down, during sleep, or in the early morning-and how body position affects breathing. These details help determine whether the issue may be orthopnea, paroxysmal nocturnal dyspnea, or another form of nighttime breathlessness. The doctor may also ask about associated signs such as leg swelling, cough, or wheezing, which help differentiate cardiac from respiratory causes.
- Symptom timing and body position are key diagnostic clues.
- Doctors assess related signs such as leg swelling, cough, or wheezing.
- Breathing effort and posture are observed during examination.
Diagnostic testing
After the initial evaluation, diagnostic tests are chosen to clarify the underlying condition. Common investigations include a chest X-ray to detect lung congestion or structural changes, an electrocardiogram (ECG) to assess heart rhythm, and an echocardiogram to evaluate heart function and fluid buildup. Pulse oximetry measures blood oxygen levels, while spirometry tests airflow and lung capacity.
| Test | Purpose |
|---|---|
| Chest X-ray | Detects fluid or congestion in the lungs |
| Electrocardiogram (ECG) | Assesses heart rhythm and electrical activity |
| Echocardiogram | Evaluates heart structure and pumping function |
| Pulse oximetry | Measures oxygen saturation in the blood |
| Spirometry | Tests airflow and lung capacity |
| Sleep study (polysomnography) | Detects sleep apnea or low oxygen during sleep |
If sleep-related breathing problems are suspected, a sleep study may be recommended to identify sleep apnea or nighttime oxygen desaturation. These tests, combined with clinical history and examination, allow healthcare providers to pinpoint the cause of nocturnal breathlessness and develop effective treatment plans.
Questions to ask your clinician
- What possible causes could explain my nighttime shortness of breath?
- Which tests will help determine whether it’s heart or lung related?
- How can I prepare for diagnostic tests like an echocardiogram or sleep study?
- Are there any warning signs that mean I should seek urgent care?
These questions can help you better understand your condition and take an active role in your diagnostic process.
Treatment and Living Well with Shortness of Breath at Night
Managing shortness of breath at night begins with understanding and addressing its underlying cause. While this symptom can be distressing, most cases improve significantly once heart, lung, or sleep-related conditions are properly treated. Ongoing care-supported by lifestyle changes and regular follow-up-helps maintain comfort and reduce the risk of recurrence.
Medical management
Doctors focus first on treating the root condition responsible for nighttime breathlessness. For individuals with heart failure, optimizing therapy helps reduce fluid buildup in the lungs and ease pressure in the chest. Those with chronic obstructive pulmonary disease (COPD) or asthma may benefit from medications that open the airways and improve airflow. If sleep apnea is identified, continuous positive airway pressure (CPAP) or other breathing aids may be used to keep airways open during sleep. Each treatment plan is tailored to the specific cause, with the goal of restoring normal breathing patterns and improving sleep quality.
- Heart failure: therapy to reduce lung fluid and pressure
- COPD or asthma: medications to open airways and ease breathing
- Sleep apnea: CPAP or other devices to maintain airway patency
Because severe or sudden shortness of breath at night may signal an urgent problem-such as worsening heart failure or respiratory distress-immediate medical evaluation is essential. Early intervention not only relieves symptoms but also helps prevent complications that could become life-threatening.
Lifestyle and prevention
Simple adjustments can often make breathing easier at night. Elevating the head and upper body with extra pillows or an adjustable bed can help reduce pressure on the lungs and improve airflow. Maintaining a healthy weight lowers strain on both the heart and respiratory system, while avoiding heavy meals and alcohol before bedtime may lessen discomfort. For individuals sensitive to allergens or temperature changes, keeping the sleeping environment clean and well-ventilated can also reduce nighttime symptoms.
- Sleep with the head elevated to improve breathing comfort.
- Maintain a healthy weight to ease heart and lung strain.
- Avoid large meals and alcohol close to bedtime.
- Keep bedroom air clean and well-ventilated.
These measures work best when combined with consistent medical management. By minimizing fluid retention, improving oxygen delivery, and supporting restful sleep, lifestyle habits play a vital role in long-term relief.
Monitoring and follow-up
Effective control of nocturnal dyspnea relies on continued monitoring and communication with healthcare providers. Patients are encouraged to track when symptoms occur, note their severity, and share any changes during medical visits. Regular follow-up appointments allow doctors to adjust medications, review test results, and ensure that treatment remains effective as conditions evolve.
With a proactive approach-combining professional care, home adjustments, and awareness of warning signs-most people can achieve significant improvement and regain confidence in their nighttime breathing.
Frequently Asked Questions About Shortness of Breath at Night
- Why does shortness of breath happen more often at night?
- When lying flat, fluid and blood shift toward the chest, raising pressure in the lungs. This can make breathing harder, especially for people with heart or lung disease.
- Is nighttime breathlessness always a sign of heart failure?
- No. While heart failure is a common cause, other factors such as COPD, asthma, sleep apnea, or reflux can also make breathing difficult during sleep.
- How is orthopnea different from paroxysmal nocturnal dyspnea?
- Orthopnea occurs immediately after lying down and improves when sitting up. Paroxysmal nocturnal dyspnea develops later during sleep and may awaken a person gasping for air.
- Can sleep apnea cause shortness of breath at night?
- Yes. Sleep apnea causes repeated pauses in breathing during sleep, leading to drops in oxygen levels that may trigger sudden awakenings with shortness of breath.
- When should I seek urgent medical care for nighttime breathlessness?
- If shortness of breath is sudden, severe, or accompanied by chest pain or dizziness, seek medical attention immediately as it could indicate a serious heart or lung condition.
- What tests might doctors order to find the cause?
- Doctors often use chest X-rays, ECGs, echocardiograms, spirometry, or sleep studies to identify whether heart, lung, or sleep-related problems are responsible.
- Can lifestyle changes help reduce nighttime shortness of breath?
- Yes. Sleeping with your head elevated, maintaining a healthy weight, and avoiding alcohol or large meals before bed can make breathing easier at night.
- Is shortness of breath at night related to anxiety?
- In some cases, anxiety or panic episodes can cause chest tightness and rapid breathing at night. However, medical causes should be ruled out first.
- How can monitoring symptoms help my doctor?
- Keeping track of when shortness of breath occurs, how severe it feels, and what positions worsen it helps doctors identify underlying conditions and adjust treatment effectively.