Shortness of Breath on Exertion: Diagnosis and Treatment Options
Exertional Breathlessness
Feeling short of breath while walking uphill, climbing stairs, or doing light exercise is a common experience. In medical terms, this symptom is called exertional dyspnea-a sensation of difficult or uncomfortable breathing that appears during physical activity. It happens when the body’s demand for oxygen rises faster than the heart and lungs can deliver it. Although many people notice this occasionally, especially when out of shape or recovering from illness, persistent breathlessness on exertion deserves attention.
What it feels like
Exertional breathlessness can feel like tightness in the chest, a struggle to get enough air, or a sense that breathing takes extra effort during movement. Some people describe it as being unable to take a deep breath or needing to stop to catch their breath sooner than others. The sensation may come on gradually or suddenly, depending on how hard the heart and lungs must work.
- Occurs during activities such as light walking, climbing, or household chores.
- May be accompanied by chest tightness, shallow breathing, or fatigue.
- Varies in timing and severity depending on exertion level and health status.
Doctors often ask patients to describe how long the symptom has been present, what brings it on, and how quickly it eases with rest. These details help separate temporary breathlessness caused by exertion or deconditioning from more persistent forms linked to heart or lung conditions.
Why it matters
While shortness of breath on exertion can appear in healthy individuals after intense effort, ongoing or unexplained symptoms may point to medical causes. It frequently occurs in cardiovascular or respiratory diseases such as heart failure, coronary artery disease, chronic lung disease, or anemia.
- Can be an early sign of heart or lung disease.
- Associated with reduced exercise tolerance when chronic.
- May predict long-term health outcomes if left unaddressed.
For that reason, clinicians take it seriously as an early clue to how efficiently the heart and lungs are working together. Recognizing exertional dyspnea early allows timely evaluation and management. Understanding that this symptom is common-and often manageable once its cause is identified-helps patients approach medical assessment with confidence rather than fear.
Inside the Body: How Breathlessness Happens
Shortness of breath during exertion arises when the body’s demand for oxygen and the ability of the lungs, heart, and muscles to supply and use that oxygen fall out of balance. This mismatch between ventilatory demand and capacity creates the sensation known as dyspnea. Understanding how these systems interact helps explain why physical activity can suddenly feel more difficult for some people than others.
The demand-capacity balance
During exercise, muscles require more oxygen to produce energy, which increases both breathing rate and heart rate. The lungs must move greater volumes of air to deliver oxygen, while the heart must circulate it efficiently throughout the body. If either the ventilatory system or circulatory system cannot keep pace with this rising demand, breathing becomes uncomfortable or labored.
- Exercise increases oxygen demand in muscles.
- The lungs and heart must work together to meet this demand.
- When demand exceeds capacity, breathlessness develops.
This imbalance-where the need for ventilation exceeds what the body can provide-is the primary physiological trigger for exertional breathlessness. In healthy individuals, this balance is maintained even under moderate strain. However, when disease or reduced conditioning limits capacity, the body reaches its threshold for oxygen delivery sooner, leading to an earlier onset of dyspnea.
The lung and muscle connection
The lungs and respiratory muscles work together to support ventilation. When ventilatory inefficiency develops-such as when airflow is limited or gas exchange is less effective-the lungs must work harder to deliver oxygen. This increased effort places greater strain on the diaphragm and accessory breathing muscles.
- Ventilatory inefficiency forces the lungs to work harder.
- Diaphragm and accessory muscles experience increased workload.
- Reduced aerobic reserve means smaller tolerance for exertion.
Over time, the added workload can lead to fatigue and the perception that breathing is more difficult than usual. Neural and perceptual factors in the brain further amplify this awareness, turning physiological strain into the recognizable feeling of shortness of breath.
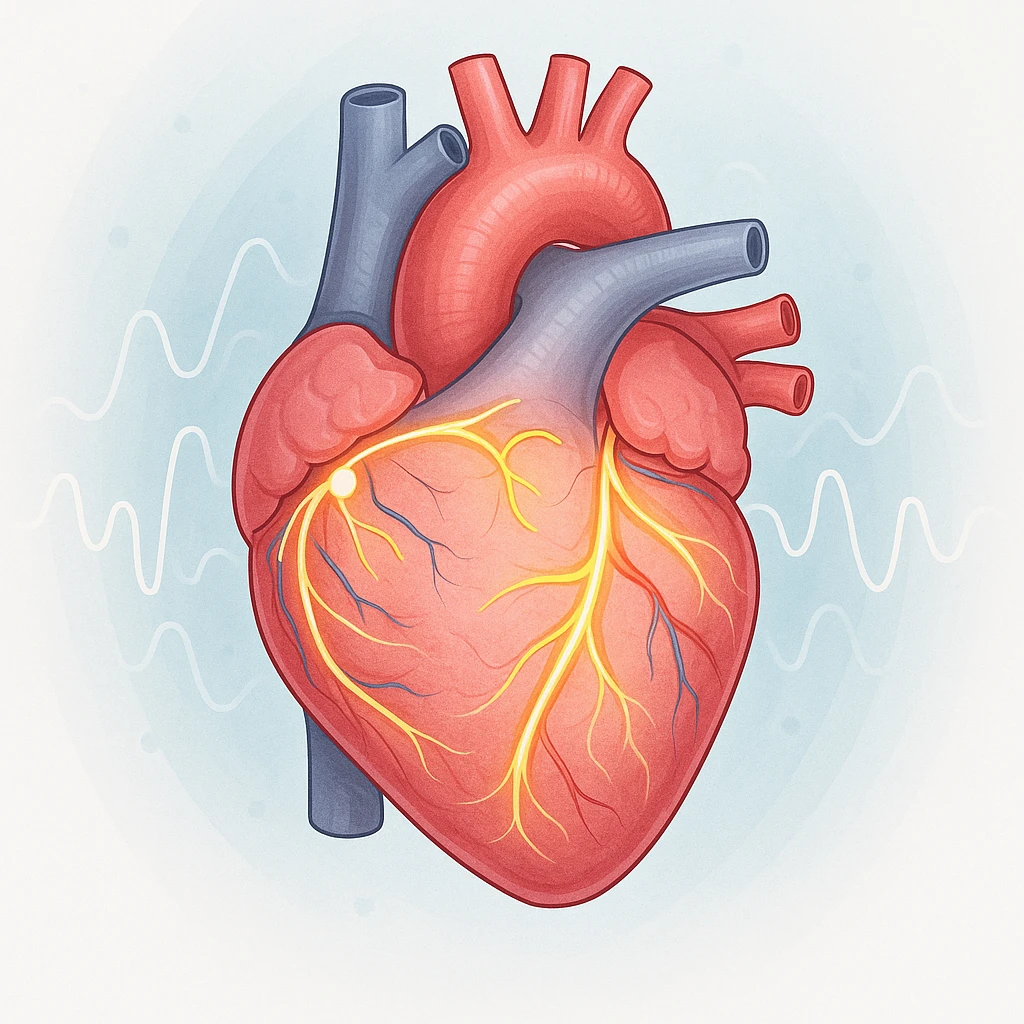
When the heart can’t keep up
The heart’s role is to deliver oxygen-rich blood to working muscles. When cardiac function is impaired-whether from weakened heart muscle, valve problems, or limited blood flow-oxygen delivery to tissues drops. To compensate, the body increases breathing rate in an attempt to bring in more oxygen, even though the underlying issue lies with circulation rather than ventilation.
This mismatch compounds exertional symptoms, making even routine activity feel strenuous. Ultimately, breathlessness during exertion reflects the body’s integrated response to stress on the lungs, heart, and muscles. When any part of this network cannot meet rising oxygen demand, breathing feels harder, signaling that the system is operating near its physiological limit.
Conditions That Commonly Cause Exertional Dyspnea
Shortness of breath during physical activity can stem from a range of heart, lung, and systemic conditions that affect how the body moves and uses oxygen. These problems often limit the efficiency of blood flow or gas exchange, making it harder to meet the body’s increased oxygen demands during exertion. Understanding the main medical causes helps explain why this symptom may persist even when rest feels comfortable.
Heart-related causes
When the heart’s pumping or blood flow is impaired, oxygen delivery to muscles decreases. Heart failure-where the heart muscle weakens and struggles to move blood forward-can cause breathlessness during even mild exertion. Coronary artery disease, which narrows the vessels supplying the heart itself, can similarly limit oxygen availability. As the heart works harder to keep up, pressure can build in the lungs, leading to a sense of heaviness or tightness during activity.
- Heart failure reduces the heart’s ability to pump blood efficiently.
- Coronary artery disease limits blood and oxygen flow to the heart muscle.
- Fluid buildup in the lungs increases pressure and discomfort during exertion.
Lung-related causes
The lungs are responsible for transferring oxygen into the bloodstream and removing carbon dioxide. Chronic obstructive pulmonary disease (COPD) makes this process less efficient by narrowing airways and trapping air, forcing people to work harder to breathe. Interstitial lung diseases, which stiffen the lung tissue, reduce the lungs’ ability to expand and exchange gases. In both cases, the lungs cannot meet the increased ventilatory demands of physical activity, producing the sensation of exertional breathlessness.
- COPD causes airway narrowing and air trapping, making breathing less efficient.
- Interstitial lung disease reduces lung flexibility and gas exchange capacity.
- Both conditions increase breathing effort during activity.
Other contributing factors
Beyond the heart and lungs, systemic conditions like anemia-where blood carries less oxygen-can also cause exertional dyspnea. Even without structural disease, the reduced oxygen-carrying capacity forces the body to increase breathing and heart rate during exertion. Additionally, some individuals experience overlapping heart and lung problems, creating a combined burden that keeps symptoms present despite targeted treatment. This overlap can make breathlessness more persistent and challenging to manage.
- Anemia decreases the blood’s oxygen-carrying ability.
- Combined heart and lung disease can amplify symptoms even with treatment.
- Overlapping conditions make exertional breathlessness harder to resolve.
When to see a doctor
It’s important to seek medical evaluation if breathlessness is new, worsening, or occurs with chest pain, dizziness, or swelling. Early assessment helps identify whether the cause lies in the heart, lungs, or another system, allowing treatment to begin before symptoms become more limiting.
How Doctors Find the Cause
If you’re experiencing shortness of breath during exertion, it’s important to work with your doctor to identify the underlying cause. The process typically begins with a thorough evaluation, starting with your medical history, a physical exam, and a series of initial tests to rule out common causes. If these tests don’t provide clear answers, additional, more specialized testing may be needed. Understanding how doctors approach this evaluation can help you feel confident in the process and the care you’ll receive.
Initial clinical evaluation
During your first visit, your doctor will gather information about your symptoms, medical history, and lifestyle. A physical exam will help identify any obvious signs of illness. Common initial tests include:
- Chest X-ray to check for lung issues, such as fluid or lung disease.
- ECG (electrocardiogram) to assess heart rhythm and check for underlying heart conditions.
- Spirometry to measure lung function and detect conditions like asthma or COPD.
These tests help your doctor determine if there are clear signs of heart or lung issues that may be contributing to your breathlessness. The goal of this first step is to identify major causes and start to narrow down the possibilities.
Specialized testing
If the initial evaluation doesn’t pinpoint the cause, your doctor may order more specialized tests to look deeper into the heart and lungs. These tests include:
- Echocardiography to check the structure and function of the heart.
- Cardiac stress testing to assess how well your heart performs under physical exertion.
- CT chest imaging to get a detailed view of the lungs and check for diseases like pulmonary fibrosis.
These tests provide more detailed images and data to help doctors understand how your heart and lungs are functioning under stress, helping to clarify whether the problem lies with the heart, lungs, or both.
Exercise assessment
In cases where it’s still unclear whether heart or lung issues are causing exertional dyspnea, exercise testing can be helpful. This test involves monitoring your heart rate, oxygen levels, and breathing while you exercise on a treadmill or stationary bike. By observing how your body responds to physical exertion, your doctor can better understand whether your symptoms are related to the heart or lungs.
Exercise testing can distinguish between cardiac and pulmonary limitations, providing valuable insight for diagnosis. It also helps guide treatment plans tailored to your specific condition.
Managing Breathlessness and Regaining Stamina
While treating the underlying cause of exertional dyspnea is essential, managing shortness of breath on exertion also involves strategies to improve endurance and overall well-being. For many individuals, addressing the root cause of the symptom-whether related to heart, lung, or systemic issues-helps reduce its intensity. However, for those with persistent symptoms, rehabilitation and other techniques can help restore stamina and improve quality of life. These treatments aim to enhance lung and heart function, reduce symptoms, and increase physical activity tolerance.
Optimizing Medical Care
The first step in managing exertional dyspnea is addressing the underlying medical condition. For example, heart failure treatment may include medications to improve heart function, while COPD management may focus on medications to open airways. Managing anemia or controlling chronic diseases like diabetes can also significantly reduce symptoms. By optimizing the function of the heart, lungs, or other affected systems, many patients experience a decrease in shortness of breath and an improvement in overall health.
- Medications to improve heart function in heart failure.
- Airway-opening medications for COPD.
- Control of chronic diseases like diabetes or anemia to reduce symptoms.
Rehabilitation and Breathing Retraining
Rehabilitation programs, including pulmonary or cardiac rehab, are often key components in managing exertional breathlessness. These programs involve exercise training tailored to the individual’s physical capabilities and breathing exercises designed to improve lung capacity and efficiency. Breathing retraining techniques, such as diaphragmatic breathing, teach patients how to use their respiratory muscles more effectively, reducing the feeling of breathlessness during exertion.
Regular participation in these programs can help increase endurance, reduce fatigue, and improve the quality of life, even for those who continue to experience residual symptoms despite medical treatment.
Living with Residual Symptoms
Even with treatment, some individuals may continue to experience persistent breathlessness. In these cases, multidisciplinary rehabilitation strategies are often beneficial. These strategies may include working with physical therapists, respiratory therapists, and other healthcare providers who specialize in symptom management. Regular physical activity, pacing techniques, and lifestyle adjustments can all play a role in improving stamina and reducing the impact of residual dyspnea on daily activities.
- Physical therapy to improve stamina.
- Breathing exercises to reduce fatigue.
- Lifestyle adjustments to better manage symptoms.
Recognizing the signs of improvement-such as being able to perform tasks with less shortness of breath or exercising for longer periods-can help motivate patients and reassure them that progress is being made. It’s important for individuals to continue managing their health actively, working with healthcare providers to adjust treatment plans as necessary.
- Shortness of breath on exertion (exertional dyspnea) is difficulty breathing during physical activity.
- This symptom is common in cardiovascular and respiratory diseases and may predict long-term health risks.
- Dyspnea occurs when the body’s demand for oxygen exceeds its ventilatory capacity.
- Contributing factors include ventilatory inefficiency, diaphragm dysfunction, and reduced aerobic reserve.
- Heart failure, coronary artery disease, COPD, interstitial lung disease, and anemia are frequent causes of exertional dyspnea.
- Heart-lung disease overlap can lead to persistent breathlessness despite treatment.
- Initial evaluation involves a detailed history, physical exam, chest X-ray, ECG, and spirometry.
- Persistent dyspnea may improve with multidisciplinary rehabilitation and symptom management.
- Improving ventilatory efficiency and aerobic conditioning can improve prognosis and quality of life.
- What is exertional dyspnea?
- Exertional dyspnea refers to shortness of breath that occurs during physical activity when the body’s demand for oxygen exceeds its capacity to deliver it.
- What causes shortness of breath on exertion?
- Conditions like heart failure, COPD, coronary artery disease, and anemia can lead to exertional dyspnea by impairing the body’s ability to supply oxygen efficiently during activity.
- How does the body react during exertion?
- During exertion, muscles need more oxygen, which causes the heart and lungs to work harder. If they can’t keep up, shortness of breath results.
- Why do some people experience breathlessness during mild activities?
- For some individuals, conditions like heart or lung diseases or even poor physical conditioning can cause breathlessness even during light activities like walking or climbing stairs.
- What should I do if I experience persistent breathlessness?
- If shortness of breath on exertion persists, it’s important to seek medical evaluation to identify the underlying cause and prevent potential complications.
- Can exercise rehabilitation help with exertional dyspnea?
- Yes, exercise rehabilitation programs can improve endurance and lung capacity, reducing symptoms of exertional breathlessness over time.