Shortness of Breath in Pleural Carcinoma
Shortness of Breath in Pleural Carcinoma: Understanding the Symptom, Its Causes, and Management
- What It Feels Like and Why It Happens in Pleural Carcinoma
- How Tumors Affect the Pleura and Breathing Function
- How Frequently Does This Symptom Occur in Patients with Pleural Carcinoma?
- Why Shortness of Breath Develops in Pleural Cancer Patients
- When Is Shortness of Breath a Medical Emergency?
- How Doctors Diagnose the Cause of Shortness of Breath in Pleural Carcinoma
- How Breathlessness Is Treated in Patients with Pleural Carcinoma
- Can Shortness of Breath Be Prevented or Reduced in Pleural Cancer?
- Will Shortness of Breath Resolve Completely?
- What Oncologists and Pulmonologists Say About Managing This Symptom
- Questions to Ask Your Doctor
- FAQ: Shortness of Breath in Pleural Carcinoma
What It Feels Like and Why It Happens in Pleural Carcinoma
Shortness of breath—also known as dyspnea—is one of the most distressing and common symptoms in patients with pleural carcinoma. It typically manifests as a sensation of air hunger, difficulty taking a full breath, or tightness in the chest. This symptom may begin gradually or come on suddenly, often worsening with physical exertion or when lying flat.
Pleural carcinoma refers to carcinoma that arises in or invades the pleura—the thin membranes lining the lungs and chest cavity. As the tumor grows, it interferes with normal lung mechanics and oxygen exchange. Patients may feel as though their lungs cannot expand properly or that there’s a weight on their chest.
This symptom is particularly prominent in malignant pleural mesothelioma and metastatic pleural involvement from other cancers such as breast, lung, or even cat mammary cancer in veterinary parallels.
How Tumors Affect the Pleura and Breathing Function
The pleura has two layers: the visceral pleura (attached to the lung) and the parietal pleura (lining the chest wall). These normally glide smoothly during breathing. In pleural carcinoma, tumor cells invade these layers, causing inflammation, fluid buildup, or fibrosis—all of which interfere with lung expansion.
Mechanisms Leading to Dyspnea in Pleural Carcinoma
| Pathophysiological Change | Effect on Breathing |
| Tumor mass compressing lung tissue | Reduces lung capacity |
| Pleural effusion (fluid buildup) | Prevents full lung expansion |
| Fibrosis and pleural thickening | Restricts lung mobility |
| Tumor infiltration of diaphragm | Weakens respiratory muscle function |
| Inflammatory response | Triggers pain and shallow breathing |
These effects can occur independently or in combination. The result is impaired ventilation and reduced oxygen exchange—leading to shortness of breath at rest or during exertion.
How Frequently Does This Symptom Occur in Patients with Pleural Carcinoma?
Dyspnea is among the most commonly reported symptoms in pleural malignancies. Studies show that it affects the majority of patients with advanced pleural disease—regardless of whether the carcinoma is primary or secondary (metastatic).
Clinical Data on Dyspnea in Pleural Carcinoma
| Condition Type | Prevalence of Dyspnea |
| Malignant Pleural Mesothelioma | ~90% |
| Metastatic Breast or Lung Carcinoma to Pleura | ~70–85% |
| Early-stage localized pleural carcinoma | ~30–50% |
| Advanced Metaplastic Carcinoma with pleural spread | Often present |
In some cases, dyspnea is the first presenting symptom, prompting diagnostic imaging. In others, it progresses over time in tandem with pleural effusion or tumor growth.
Why Shortness of Breath Develops in Pleural Cancer Patients
The development of breathlessness in pleural carcinoma is driven by several direct and indirect mechanisms. It may be caused by the tumor itself, secondary effects like fluid accumulation, or even side effects of treatment.
Contributing Causes of Dyspnea in Pleural Carcinoma
| Cause Type | Description |
| Tumor-related | Mass effect, pleural invasion, diaphragmatic involvement |
| Fluid-related | Malignant pleural effusion compressing lung tissue |
| Inflammatory | Cytokine-induced pleuritis causing pain and shallow respiration |
| Treatment-induced | Radiation fibrosis, chemotherapy-induced pneumonitis |
| Comorbidities | Anemia, heart failure, or pulmonary embolism further reducing oxygenation |
In many patients, dyspnea is multifactorial—necessitating a comprehensive workup to determine all contributing elements before initiating treatment.
When Is Shortness of Breath a Medical Emergency?

While mild or moderate shortness of breath is common in pleural carcinoma, certain signs require immediate medical intervention. Any sudden worsening of breathing, especially if accompanied by chest pain, bluish lips or fingertips (cyanosis), confusion, or rapid heartbeat, should be treated as a potential emergency.
Acute respiratory distress may indicate a rapidly expanding pleural effusion, tumor compression of major airways, or a pulmonary embolism. In rare cases, tension hydrothorax or pneumothorax may develop when the tumor erodes into lung tissue or pleural blood vessels, leading to life-threatening complications.
A patient with pleural carcinoma should never ignore a sharp change in their baseline breathing pattern. In such cases, urgent imaging and intervention—such as pleural drainage or oxygen support—may be lifesaving.
Red Flags for Urgent Evaluation
| Symptom or Sign | Possible Cause |
| Sudden inability to breathe deeply | Rapid pleural fluid accumulation |
| Sharp chest pain with breathing | Tumor invasion or pleuritis |
| Dizziness, low oxygen saturation | Hypoxemia from lung compression |
| Asymmetric chest expansion | Lung collapse or massive effusion |
| Confusion or agitation | Respiratory failure |
Prompt recognition of these warning signs ensures rapid stabilization and prevents further decline in respiratory function.
How Doctors Diagnose the Cause of Shortness of Breath in Pleural Carcinoma
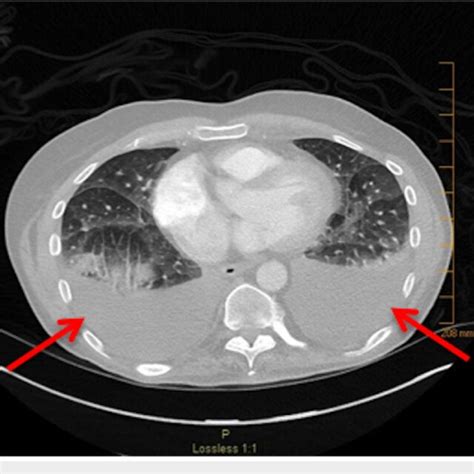
Diagnosis begins with a detailed clinical history and physical examination, followed by imaging and specialized tests. Physicians assess the character of the breathing difficulty, onset, aggravating factors, and any associated symptoms like cough, fever, or pain.
Common Diagnostic Methods for Dyspnea in Pleural Carcinoma
| Diagnostic Tool | Purpose |
| Chest X-ray | Identifies effusions, masses, or lung collapse |
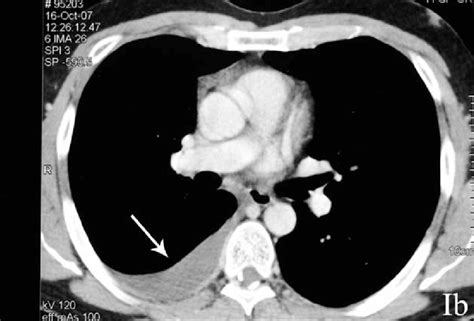
| CT Scan of Chest | Detailed view of pleural thickness, tumor spread, nodules |
| Thoracic Ultrasound | Assesses fluid volume for guided drainage |
| Pulmonary Function Tests | Measures lung capacity and airway resistance |
| Arterial Blood Gas (ABG) | Evaluates oxygenation and CO₂ retention |
| Thoracentesis with Cytology | Analyzes pleural fluid for malignant cells |
| Pleural Biopsy | Confirms diagnosis if fluid analysis is inconclusive |
CT imaging is especially critical in pleural carcinoma because it reveals the full extent of pleural and diaphragmatic involvement—key to differentiating tumor growth from other causes of breathlessness. When fluid is present, thoracentesis provides both diagnostic and therapeutic relief.
How Breathlessness Is Treated in Patients with Pleural Carcinoma
Managing shortness of breath in pleural cancer requires both symptom relief and treatment of the underlying cause. Often, a multidisciplinary approach is needed—combining oncology, pulmonology, and palliative care teams.
Clinical Approaches to Relieve Dyspnea
| Treatment Approach | Application |
| Therapeutic Thoracentesis | Removes pleural fluid to improve lung expansion |
| Indwelling Pleural Catheter | Allows ongoing drainage at home for recurrent effusions |
| Pleurodesis (Talc or Chemical) | Prevents reaccumulation of malignant fluid |
| Systemic Chemotherapy or Immunotherapy | Reduces tumor mass and fluid production |
| Oxygen Therapy | Improves oxygen levels in hypoxic patients |
| Opioids (e.g., morphine) | Reduces breathlessness perception, especially at end-stage |
| Non-invasive ventilation (BiPAP/CPAP) | Supports breathing in selected patients |
Symptom control is often prioritized in advanced disease stages, where curative treatment is not possible. Gentle physiotherapy, upright positioning, and calm breathing techniques may also offer relief.
Can Shortness of Breath Be Prevented or Reduced in Pleural Cancer?
While not all cases of dyspnea in pleural carcinoma are preventable, early intervention can reduce severity and frequency. Monitoring patients for fluid accumulation or tumor progression allows for timely therapeutic drainage or medication adjustments.
Lifestyle modifications and positioning strategies also play a role in comfort. Sleeping with the head elevated, avoiding tight clothing around the chest, and using a fan for airflow across the face may alleviate perceived breathlessness.
Preventive Strategies and Supportive Care
| Strategy | Benefit |
| Regular imaging follow-up | Detects effusion or tumor growth early |
| Early thoracentesis for minor fluid buildup | Prevents acute respiratory distress |
| Ongoing symptom monitoring | Promotes proactive treatment adjustments |
| Respiratory therapy involvement | Supports breathing mechanics and pacing |
| Nutritional and psychological support | Reduces fatigue-related breathlessness perception |
Although breathlessness is a hallmark of pleural malignancy, comprehensive care can improve function and quality of life, especially in those with slowly progressing forms of carcinoma.
Will Shortness of Breath Resolve Completely?
Whether dyspnea resolves in pleural carcinoma depends on multiple factors: the cancer’s stage, rate of progression, type of treatment, and presence of complications like pleural effusion or fibrosis. In early or localized cases, treating the tumor and removing fluid may significantly relieve breathing symptoms—sometimes completely.
However, in advanced disease, especially with extensive pleural involvement or metaplastic carcinoma that’s resistant to treatment, shortness of breath may persist or worsen despite intervention. Even when tumors shrink with chemotherapy or immunotherapy, scarring or permanent pleural thickening may limit full recovery of lung function.
In palliative care settings, the focus is on improving quality of breath rather than eliminating the symptom entirely. With coordinated support—including drainage, medication, oxygen, and psychological comfort—most patients can achieve meaningful relief.
Outcomes Based on Disease Stage
| Disease Stage or Scenario | Likelihood of Symptom Resolution |
| Early-stage pleural carcinoma | High, especially after resection or local therapy |
| Moderate pleural effusion, no fibrosis | Moderate; improves with drainage |
| Advanced-stage with thickening/fibrosis | Partial relief; may remain chronic |
| Terminal cases (widespread metastasis) | Symptom management is focus, not full resolution |
The key takeaway: while breathlessness may not always disappear, it can often be managed effectively with timely and tailored care.
What Oncologists and Pulmonologists Say About Managing This Symptom
Experts in thoracic oncology and pulmonology agree that shortness of breath in pleural carcinoma should never be dismissed as “just part of the cancer.” Instead, it’s a treatable, often reversible symptom that significantly affects patient comfort and prognosis.
Oncologists recommend integrating dyspnea management into the broader cancer treatment plan. This includes scheduling routine thoracic imaging, identifying early signs of pleural fluid buildup, and planning early intervention strategies—even in outpatient settings.
Pulmonologists emphasize the value of indwelling pleural catheters for long-term control of recurrent effusions. They also advocate for non-pharmacologic strategies like breath retraining, positioning, and anxiety-reducing therapies, which help patients cope with the sensation of breathlessness.
In complex cases—such as when cat mammary cancer or other metastatic cancers invade the pleura—specialists highlight the importance of multidisciplinary collaboration to optimize both cancer control and respiratory comfort.
Questions to Ask Your Doctor
To better understand and manage breathing difficulties in pleural carcinoma, patients and caregivers should ask informed, practical questions during clinical visits. These conversations help shape effective and proactive care plans.
| Suggested Questions | Why It Matters |
| What is causing my shortness of breath? | Helps target the exact mechanism (fluid, tumor, fibrosis) |
| Is this a sign that the cancer is progressing? | Identifies whether further staging is needed |
| Do I need drainage or imaging now? | Guides urgent vs. planned intervention |
| How can we monitor changes in my breathing? | Establishes follow-up and self-checks |
| What treatments are available to help me breathe better? | Clarifies both medical and procedural options |
| Should I consider a pleural catheter or pleurodesis? | Explores long-term symptom control strategies |
| Is supplemental oxygen helpful or necessary? | Evaluates oxygen needs at rest and during activity |
| Can I still exercise or move around safely? | Encourages physical activity within safe limits |
| Should I sleep in a certain position? | Enhances comfort during nighttime breathing |
| How does anxiety affect this symptom? | Identifies psychosomatic triggers of breathlessness |
| Can I prevent fluid from coming back? | Discusses tumor control and pleural interventions |
| Are there medications to make me feel less breathless? | Explores palliative relief options |
| What should I do if the symptom suddenly worsens? | Prepares for emergencies |
| Will treatment improve this symptom over time? | Sets expectations realistically |
| Who can I contact for at-home respiratory support? | Involves home care or hospice if needed |
FAQ: Shortness of Breath in Pleural Carcinoma
1. Why does pleural carcinoma cause shortness of breath?
Tumors in the pleura compress lung tissue or cause fluid buildup, which interferes with lung expansion and oxygen exchange.
2. Can pleural effusion cause breathlessness even without a large tumor?
Yes. Even moderate fluid accumulation can restrict breathing, especially in older patients or those with underlying lung issues.
3. Will draining the fluid help me breathe better immediately?
Often, yes. Therapeutic thoracentesis usually provides rapid relief, although the effect may be temporary if fluid reaccumulates.
4. What is an indwelling pleural catheter, and is it safe?
It’s a soft tube left in place to allow at-home drainage. It’s generally safe and greatly improves comfort in patients with recurrent effusions.
5. Are opioids like morphine safe for breathlessness in cancer?
Yes. Low-dose opioids reduce the sensation of air hunger and are commonly used in advanced disease—even if no pain is present.
6. Can anxiety make my breathing feel worse?
Absolutely. Anxiety increases respiratory rate and tension, which can exacerbate the sensation of not getting enough air.
7. Should I go to the emergency room if I suddenly can’t breathe?
Yes. Sudden, severe dyspnea may indicate a life-threatening complication like tension effusion, embolism, or pneumothorax.
8. How do doctors know if the tumor or fluid is causing the problem?
Through imaging (X-ray, CT), physical exam, and analysis of pleural fluid if drained.
9. Can I have shortness of breath even if my lungs look clear?
Yes. Inflammatory or nerve-related factors, anemia, or weakness of the diaphragm can all affect breathing.
10. What’s pleurodesis and how does it help?
It’s a procedure that seals the pleural space to prevent fluid from returning, improving long-term breathing stability.
11. Can breathing exercises or rehab help?
Yes. Pulmonary rehab and guided breathing techniques reduce anxiety and improve functional breathing.
12. Will chemotherapy or immunotherapy relieve breathlessness?
If effective, yes—they reduce tumor size and inflammation, which can restore lung capacity.
13. Is this symptom always a sign of late-stage cancer?
Not always. Even early pleural involvement can cause dyspnea depending on location and tumor type.
14. What home adjustments can make breathing easier?
Use of fans, elevated sleeping positions, loose clothing, and reducing environmental stress all help.
15. How do I cope emotionally with this symptom?
Support from counselors, palliative care, and breathing-focused relaxation therapies can improve psychological resilience.












