Severe Skin Itching in Liver Cancer
Severe Skin Itching in Liver Cancer: What You Need to Know
- What Is This Symptom—and Why It Can Arise in Liver Cancer
- Mechanism: How Liver Dysfunction and Treatment Trigger Itching
- How Common Is Itching in Liver Cancer Patients?
- What Triggers Itching in the Context of Cancer and Treatment
- When Itching Signals a Need for Urgent Medical Attention
- How Is Itching Due to Liver Cancer Diagnosed?
- Approaches to Relieve Itching and Provide Relief
- Can Itching Be Prevented in Liver Cancer?
- Will the Itching Go Away—What to Expect Long-Term?
- What Doctors Say About Cancer-Related Itching
- 15+ Questions to Ask Your Doctor About Skin Itching and Liver Cancer
What Is This Symptom—and Why It Can Arise in Liver Cancer

Severe itchy skin (pruritus) is a lesser-known but profoundly distressing symptom seen in many patients with liver cancer. Unlike typical itchiness from dry skin or allergies, cancer-related itching tends to be widespread, intense, and resistant to over-the-counter lotions. It can feel burning or crawling, often worsened at night, and may disrupt sleep and quality of life.
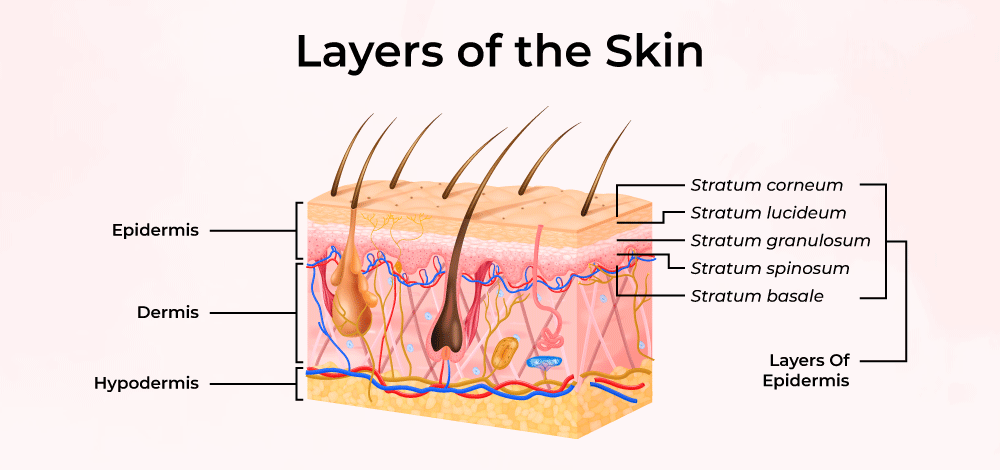
This itching is not just a peripheral phenomenon. In liver cancer, especially when there is cholestasis or bile duct involvement, substances like bile acids accumulate in the skin. These chemicals directly irritate nerve endings, eliciting a burning itch. Patients often describe it as “under the skin,” similar to the way some describe a rash associated with Liver Cancer Rash, but without visible lesions.
Itching may appear in early stages if bile flow is obstructed—or later, as complications from therapy or disease progression. Recognizing it as part of the liver cancer spectrum can help patients and providers address an often ignored but debilitating symptom.
Mechanism: How Liver Dysfunction and Treatment Trigger Itching
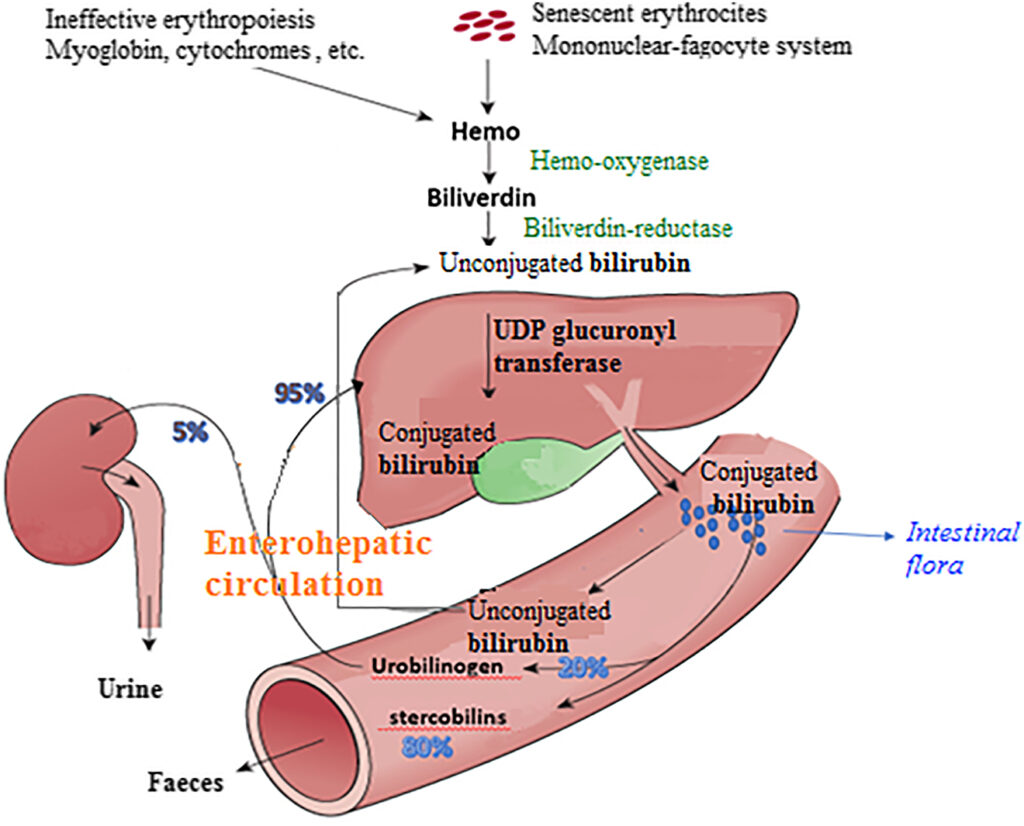
Itching in liver cancer arises through several interlinked mechanisms. When tumors grow in or near the bile ducts, they prevent normal bile flow, leading to cholestasis. Bile acids, bilirubin, and other pro-inflammatory substances then build up in the skin and systemic circulation. These directly stimulate itch-sensitive nerve fibers.
The liver also plays a role in metabolizing pruritogens—substances that provoke itching. As liver function declines, these compounds accumulate. Research suggests involvement of endogenous opioids and histamine as well; the imbalance heightens both sensation and response to itching.
Some treatments exacerbate the issue. Chemotherapy and targeted drugs can cause skin dryness or immune reactions. Radiation to liver-adjacent structures may inflame skin layers. As a result, patients undergoing symptomatic Breast Cancer Spreads to the Liver therapies or metastatic disease may experience intensified pruritus even if the primary tumor is not hepatic—highlighting systemic causes.
How Common Is Itching in Liver Cancer Patients?
The prevalence of severe itching in liver cancer patients varies based on stage and biliary involvement. Clinical studies estimate that between 20% and 40% of patients with advanced hepatocellular carcinoma or cholangiocarcinoma report pruritus severe enough to require treatment. Table 1 outlines frequency by stage:
Table 1: Itching Prevalence by Liver Cancer Stage
| Cancer Stage | Approximate Itching Incidence |
| Stage I–II (localized) | 10–15% |
| Stage III | 20–30% |
| Stage IV (metastatic) | 30–40% |
Patients with biliary obstruction due to tumor compression or bile duct involvement often show higher rates—up to 60%. In addition, jaundice (elevated bilirubin) correlates strongly with pruritus severity. People with concurrent conditions such as primary sclerosing cholangitis or cirrhosis are at increased risk.
What Triggers Itching in the Context of Cancer and Treatment
Several factors converge to cause itching during liver cancer progression and therapy:
Oncological contributors include blockage of bile ducts by tumor mass, infiltration of viral cirrhosis, and metastasis to liver vasculature. Medications like sorafenib or immunotherapies can provoke immune-mediated skin reactions or dry the epidermis. Metabolic effects—such as elevated bile salts, bilirubin, and opioidergic imbalance—also intensify skin sensitivity.
Treatment side effects, including radiation dermatitis near liver irradiation fields, further compromise skin barrier. Finally, metabolic and nutritional disturbances (zinc deficiency, dehydration) contribute to xerosis, making the skin more prone to itch.
It’s often the combination of liver failure and treatment-related changes, rather than a single cause, which makes pruritus particularly problematic in this population.
When Itching Signals a Need for Urgent Medical Attention
Most itching, while uncomfortable, can be managed. However, certain features require prompt evaluation to rule out complications.
Sudden onset of intense itching along with jaundice may suggest rapid bile duct obstruction or tumor progression. Guillain-like symptoms, such as muscle weakness or tingling, alongside itching may indicate paraneoplastic neurological syndromes. Infection signs—fever, redness, or broken skin—can herald cholangitis or cellulitis, especially when scratching leads to skin breakdown.
Table 2: Warning Signs with Itching
| Symptom Combination | Possible Concern |
| Severe pruritus + worsening jaundice | Tumor progression, bile blockage |
| Itch + fever, chills | Cholangitis, skin infection |
| Itch + muscle weakness, paresthesia | Paraneoplastic syndrome |
| Itch + sudden worsening of fatigue or confusion | Liver failure progression |
Itching that does not respond to first-line therapies within two weeks, or that impairs sleep and mental health, should also lead to specialist referral, ideally to hepatology or supportive oncology teams.
How Is Itching Due to Liver Cancer Diagnosed?
Diagnosing cancer-related pruritus often begins with a thorough history and clinical exam. The pattern, timing, severity, and associated symptoms like jaundice, weight loss, or abdominal pain are noted.
Blood tests typically include liver function panels (bilirubin, alkaline phosphatase), bile acids, and inflammatory markers. Imaging studies such as ultrasound, CT, or MRI help Detect Liver Cancer and reveal biliary obstruction. A liver elastography or MRCP may visualize ductal blockages.
In some cases, skin biopsy or allergy tests are used to rule out dermatologic diseases. Itching severity may be scored using the 5-D itch scale or visual analog scale (VAS) to monitor response to treatments.
Approaches to Relieve Itching and Provide Relief
Treatment combines symptom relief with addressing underlying liver dysfunction. First-line agents include bile acid sequestrants (cholestyramine), rifampicin for bile metabolism, and serotonin reuptake inhibitors like sertraline for neuropathic itch. Antihistamines offer limited benefit but may help sleep.
Table 3: Therapeutic Options for Itchy Skin
| Treatment | Mechanism | Typical Use |
| Cholestyramine | Binds bile acids in gut | Mild to moderate GV-related itch |
| Rifampicin | Modulates nuclear receptors to reduce itch | Moderate-severe pruritus |
| Sertraline or Gabapentin | Alters itch signaling in CNS | Refractory or neuropathic itch |
| Topical emollients, cooling gels | Moisturize and soothe irritated skin | Adjunct to systemic therapy |
| UVB phototherapy | Reduces skin nerve excitability | Persistent pruritus unresponsive to meds |
Adjunct therapies include maintaining hydration, loose cotton clothing, nightly cooling and moisturizing routines. Referral to dermatology or palliative care improves outcomes when pruritus is severe.
Can Itching Be Prevented in Liver Cancer?
Preventive strategies focus on minimizing cholestasis and supporting skin health. Early detection of bile duct involvement, potentially via Ovarian Cancer MRI-style imaging approaches, helps intercept problems. Prophylactic application of emollients, avoiding skin irritants, and managing hydration are foundational.
Regular monitoring of liver function and higher vigilance in those receiving biliary-interacting drugs can reduce early pruritus. Coordination between oncology and hepatology teams ensures that bile flow is maintained where possible.
Will the Itching Go Away—What to Expect Long-Term?
Itching tends to improve as bile flow is restored—after stenting, tumor shrinkage, or effective therapy. In cases of advanced liver disease or end-stage cancer, itch may persist and fluctuate with disease burden. Treatments like rifampicin or sertraline may provide sustained relief but come with side effects requiring ongoing monitoring.
Overall, prognosis depends on tumor control. If the cancer responds and biliary function is restored, even severe pruritus can resolve.
What Doctors Say About Cancer-Related Itching
Dr. Elena Brooks, hepatologist, emphasizes: “Itching may seem benign, but it’s one of the most distressing symptoms patients describe. Evaluating it early can uncover bile duct obstruction before severe complications arise.”
Oncologist Dr. Raj Patel adds: “We often underestimate skin symptoms as trivial. Severe itch impacts sleep, mood, even adherence to therapy. That’s why pruritus management is now part of standard supportive care protocols in liver cancer.”
These experts advocate routine itch assessment in oncology visits and inter-disciplinary approaches involving hepatology, dermatology, and palliative care.
15+ Questions to Ask Your Doctor About Skin Itching and Liver Cancer
1. What is causing my itching—is it cholestasis or another issue?
Determines best treatment approach.
2. What treatments can safely reduce my itching without harming the liver?
Identifies suitable medications (e.g., cholestyramine).
3. Could this itch be from the cancer spreading or treatment side effects?
Ruling out progression or dermatologic reaction.
4. When should I report worsening or new symptoms associated with itching?
Enables prompt investigation of complications.
5. Are there lifestyle changes to reduce itch—diet, clothing, baths?
Supports self-management and comfort.
6. Might I need imaging to check bile ducts or liver nodes?
Early detection of obstruction can relieve symptoms.
7. Could my medications cause or worsen itching?
Adjusting drugs may reduce cholestatic or immune reaction.
8. Who can I see for itch relief—dermatologist, hepatologist, palliative?
Clarifies care pathway.
9. How long before I might see relief from prescribed therapy?
Sets expectations and encourages adherence.
10. Can this itch become chronic if untreated?
Emphasizes importance of early intervention.
11. Are there side effects from treatments like rifampicin or sertraline?
Prepares you for possible lab monitoring and risks.
12. Will itch indicate cancer recurrence or liver failure?
Helps understand prognostic significance.
13. What skin-care products are safe for me?
Prevents irritation and supports skin barrier.
14. Could an itch mask a dangerous skin condition, like cancer rash?
Ensures dermatologic evaluation if unusual signs appear.
15. When should I see emergency care—e.g., for fever or skin breaks?
Prevents infection and further complications.









