Sermorelin Side Effects and Cancer: A Comprehensive Overview
- Understanding Sermorelin: Mechanism and Purpose
- Common Side Effects of Sermorelin Therapy
- Exploring the Potential Cancer Risk Associated with Sermorelin
- Comparing Sermorelin with Other Growth Hormone Therapies
- Long-Term Effects of Sermorelin: What the Research Shows
- Sermorelin Use in Cancer Survivors and High-Risk Individuals
- Who Should Avoid Sermorelin Therapy Altogether?
- Interactions Between Sermorelin and Other Medications
- Hormonal Cascades and IGF-1 Elevation: The Cancer Concern
- Sermorelin Use in Men vs. Women: Hormonal Dynamics and Risks
- Sermorelin and Pediatric Use: Why It’s Not for Children with Cancer History
- Risk Stratification Before Initiating Sermorelin: A Clinical Necessity
- Long-Term Surveillance and Post-Treatment Monitoring
- Overlooked Symptoms That Could Signal a Cancerous Link
- Current Clinical Trials and Regulatory Perspectives on Sermorelin
- Is Sermorelin Safe for Patients at Cancer Risk?
- FAQ

Understanding Sermorelin: Mechanism and Purpose
Sermorelin is a synthetic analog of growth hormone-releasing hormone (GHRH), comprising the first 29 amino acids of the naturally occurring GHRH. Its primary function is to stimulate the pituitary gland to produce and release endogenous growth hormone (GH). Unlike direct GH therapies that introduce synthetic hormones into the body, Sermorelin encourages the body’s natural hormone production mechanisms, potentially reducing the risk of hormone imbalances.
Initially approved by the FDA for diagnosing and treating growth hormone deficiencies in children, Sermorelin has found off-label use in adults seeking anti-aging benefits, improved metabolism, and enhanced physical performance. Its ability to promote natural GH secretion makes it a preferred alternative for those wary of the risks associated with synthetic GH administration.
Common Side Effects of Sermorelin Therapy
While Sermorelin is generally well-tolerated, users may experience certain side effects, particularly during the initial stages of therapy. These side effects are typically mild and transient, often resolving as the body adjusts to the treatment.
The most frequently reported side effects include:
- Injection Site Reactions: Redness, swelling, or pain at the injection site are common due to the subcutaneous administration of Sermorelin.
- Flushing: A sensation of warmth or redness, particularly in the face and neck, may occur shortly after injection.
- Headaches and Dizziness: Some individuals report mild headaches or feelings of lightheadedness, especially during the early phases of therapy.
- Nausea: A temporary feeling of nausea can occur but typically subsides with continued use.
It’s important to note that these side effects are not uncommon with peptide therapies and often diminish over time. Proper administration techniques and adherence to prescribed dosages can mitigate many of these reactions.
Exploring the Potential Cancer Risk Associated with Sermorelin
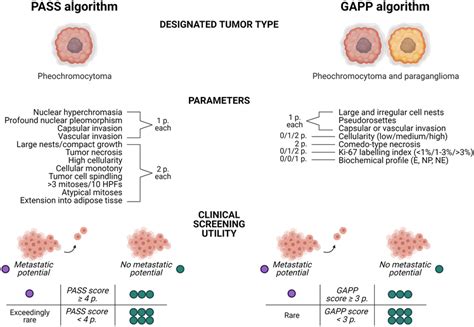
A critical concern among potential Sermorelin users is the possibility of an increased cancer risk. To date, there is no conclusive scientific evidence directly linking Sermorelin therapy to the initiation of cancer. However, the theoretical risk arises from its mechanism of stimulating growth hormone production, which could, in theory, accelerate the growth of existing cancerous cells.
Studies have shown that growth hormone and its releasing hormones can influence cell proliferation. For instance, research indicates that GHRH and its receptors may promote tumor growth in certain cancer cell lines, such as prostate cancer cells. However, these findings are primarily based on in vitro studies, and their applicability to clinical scenarios remains uncertain.
It’s essential for individuals with a history of cancer or those at high risk to consult healthcare professionals before initiating Sermorelin therapy. Regular monitoring and comprehensive evaluations can help mitigate potential risks.
Comparing Sermorelin with Other Growth Hormone Therapies
When considering hormone therapies, it’s beneficial to compare Sermorelin with other options to understand its unique advantages and potential drawbacks.
| Aspect | Sermorelin | Synthetic GH Therapy |
| Mechanism | Stimulates natural GH production via the pituitary gland | Directly introduces synthetic GH into the bloodstream |
| Regulation | Subject to body’s feedback mechanisms, reducing overdose risk | Higher risk of hormone imbalances due to external GH levels |
| Cancer Risk | Theoretical risk in accelerating existing tumors; no direct evidence | Potential risk due to elevated IGF-1 levels; more studies needed |
| Side Effects | Generally mild and transient | Can include joint pain, insulin resistance, and edema |
| Cost | Typically more affordable | Often more expensive due to synthetic hormone production |
This comparison highlights Sermorelin’s role in promoting the body’s natural hormone production, potentially offering a safer profile for certain individuals, especially when monitored appropriately.
Long-Term Effects of Sermorelin: What the Research Shows
Although short-term studies suggest Sermorelin is generally safe for most users, long-term data remain limited and warrant careful consideration. Continuous stimulation of the pituitary gland to produce growth hormone raises questions about chronic effects on endocrine feedback loops, metabolic health, and cell replication.
Current long-term observations have not shown a strong causal link between Sermorelin and cancer development, but the lack of extensive data leaves room for clinical caution. Some practitioners argue that prolonged GH stimulation might elevate insulin-like growth factor 1 (IGF-1) levels, a biomarker associated with increased risk in hormone-sensitive cancers such as breast or prostate cancer. However, this remains theoretical without robust clinical trials.
Importantly, individual variability plays a critical role. Patients with underlying genetic conditions or a family history of malignancies should undergo additional screening. In these cases, clinicians often recommend alternatives or enhanced monitoring to balance therapeutic benefit with possible long-term risks. Patients with a hereditary predisposition to hematological malignancies, such as myeloma, should consult with their oncologist before initiating GH-based treatments.

Sermorelin Use in Cancer Survivors and High-Risk Individuals
The question of whether Sermorelin is appropriate for individuals with a history of cancer remains complex. While it does not inherently initiate cancer, its action on cell growth raises concerns about stimulating dormant or microscopic tumor cells.
Oncologists typically approach such cases conservatively. For cancer survivors in remission, especially those with hormone-sensitive tumors, Sermorelin may be contraindicated unless compelling clinical benefits outweigh theoretical risks. This includes survivors of breast cancer, melanoma, and certain lymphomas.
For high-risk populations—such as those with BRCA mutations, Lynch syndrome, or a personal history of precancerous lesions—risk assessment is vital. Personalized medicine is key: genetic profiling, hormone level analysis, and imaging studies should guide decision-making.
It’s worth noting that similar caution applies in other cancers with a strong hereditary component, including those that metastasize early, such as colon cancer with peritoneal spread.
Who Should Avoid Sermorelin Therapy Altogether?
While Sermorelin is generally safe when administered under medical supervision, specific populations should approach with extreme caution—or avoid it altogether. These include:
- Individuals with active cancer
- Patients with a personal history of hormone-responsive tumors
- People with uncontrolled diabetes or insulin resistance
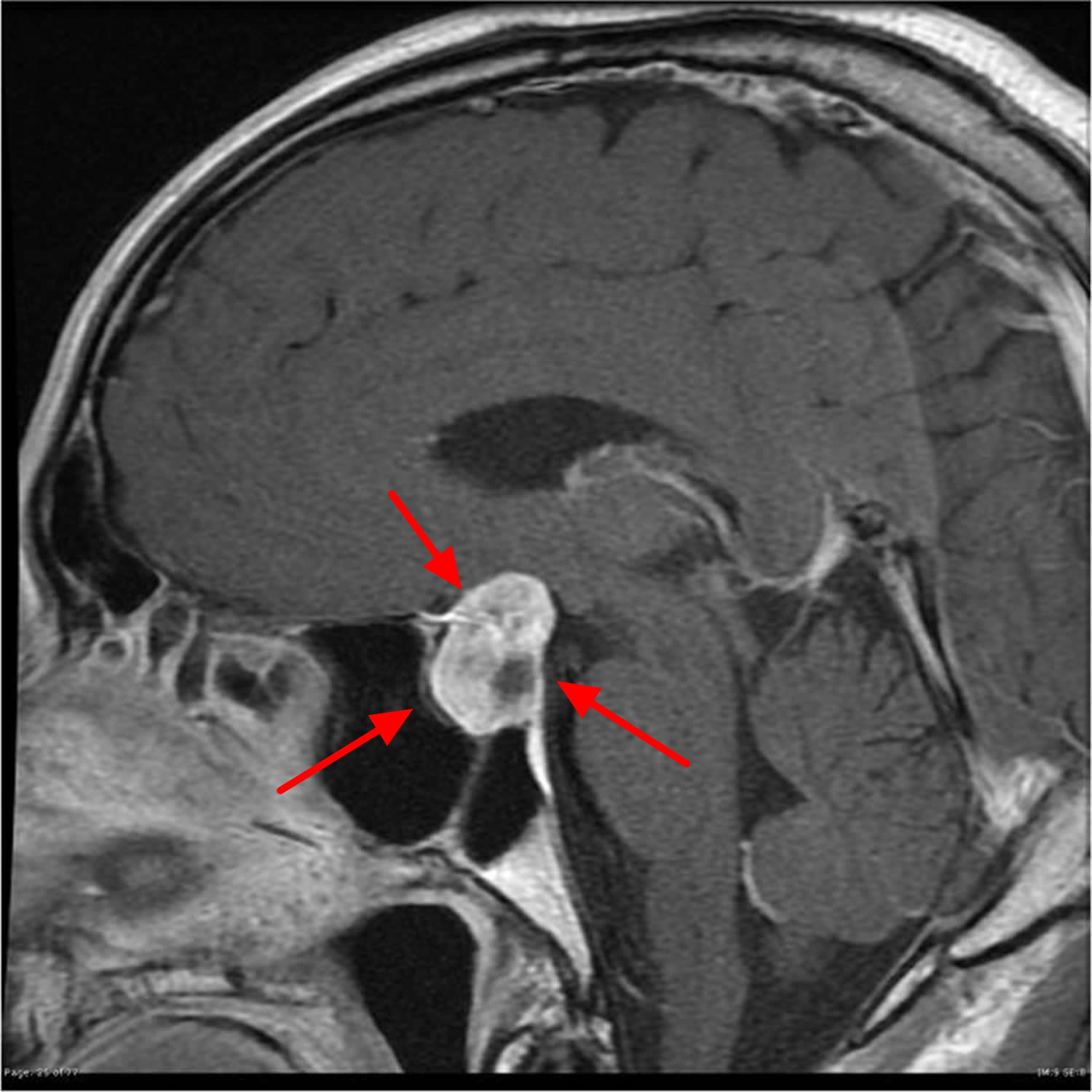
- Those with pituitary adenomas or unexplained growth hormone abnormalities
Furthermore, individuals with poorly understood symptoms such as unexplained weight loss, persistent night sweats, or uninvestigated masses should not begin Sermorelin until full diagnostic workup is complete. In some cases, these symptoms may point to early-stage malignancies or systemic disorders.
In this context, diagnostic imaging becomes crucial. Techniques like MRI, CT scans, and targeted bone density tests.
Interactions Between Sermorelin and Other Medications
Patients on complex medication regimens must disclose all drugs and supplements to their prescribing physician before starting Sermorelin. Some medications can interfere with GH production or Sermorelin’s absorption, while others may amplify side effects.
For example, glucocorticoids may suppress GH activity, diminishing Sermorelin’s effectiveness. Conversely, insulin therapy in diabetics may mask certain symptoms, such as fatigue or swelling, making it harder to detect adverse responses.
Additionally, estrogen therapy, often used in postmenopausal women, may impact IGF-1 levels and thereby alter Sermorelin’s expected outcomes. In oncology patients, any overlap with chemotherapy or immunotherapy must be reviewed to prevent unanticipated effects on tumor microenvironments.
Medical practitioners recommend a baseline panel of endocrine markers and regular re-assessment every 3 to 6 months for those combining peptide therapy with other pharmacologic agents.
Hormonal Cascades and IGF-1 Elevation: The Cancer Concern
Sermorelin indirectly increases levels of insulin-like growth factor 1 (IGF-1) by stimulating endogenous growth hormone release from the anterior pituitary. IGF-1, a potent anabolic peptide, plays a key role in cellular growth, proliferation, and survival. Its role in normal physiology is well-established, especially in tissue repair and metabolic regulation. However, its elevated levels have been implicated in several cancers.
Epidemiological data suggest correlations between high IGF-1 and increased risk of prostate, breast, and colorectal cancers. The mechanism appears to involve suppression of apoptosis and promotion of mitogenesis—conditions favorable for tumor growth. While Sermorelin does not directly inject IGF-1 into the system, its indirect stimulation means its influence must be carefully tracked.
Clinicians are advised to monitor IGF-1 levels throughout the course of treatment. If levels consistently exceed the upper reference range, dosing should be adjusted or discontinued. Additionally, if a patient has a history of borderline oncologic findings, IGF-1 monitoring is especially critical to avoid reactivation of dormant cancer cells.
Sermorelin Use in Men vs. Women: Hormonal Dynamics and Risks
Though often marketed toward aging men for its testosterone-sparing effects, Sermorelin is also used by women for growth hormone deficiencies and anti-aging protocols. However, sex-specific endocrine pathways mean the risks and benefits differ significantly.
In men, elevated IGF-1 is more strongly associated with prostate tissue proliferation. As such, prostate-specific antigen (PSA) levels should be monitored in male patients over 45. For patients already classified as having unfavorable intermediate-risk prostate cancer, Sermorelin is typically contraindicated due to its potential to aggravate cellular activity in the prostate gland.
In women, particularly those undergoing hormone replacement therapy (HRT), Sermorelin may synergize with estrogenic pathways. This necessitates enhanced caution in women with a history of breast cancer, uterine fibroids, or endometrial hyperplasia. Mammograms and transvaginal ultrasounds are often recommended prior to and during therapy.
Sermorelin and Pediatric Use: Why It’s Not for Children with Cancer History
Sermorelin was originally developed as a diagnostic agent and later a therapy for children with idiopathic growth hormone deficiency. In pediatric endocrinology, it has a favorable safety profile. However, its use is now largely overshadowed by recombinant human GH therapies.
When considering use in children with a family history of cancer, particularly hereditary cancer syndromes (e.g., Li-Fraumeni, RET mutations), Sermorelin becomes controversial. In these cases, stimulating endogenous GH may accelerate neoplastic transformations in tissues already vulnerable due to inherited mutations.
Because pediatric cancer survivors remain at increased lifetime risk for secondary malignancies, Sermorelin is usually avoided unless the benefits are overwhelmingly clear. Multidisciplinary teams including pediatric oncologists, genetic counselors, and endocrinologists are often involved in decision-making for this population.
Risk Stratification Before Initiating Sermorelin: A Clinical Necessity
Proper risk stratification is foundational to the responsible use of Sermorelin. Physicians must evaluate both oncologic and metabolic profiles before prescribing it. This involves:
- Reviewing personal and family cancer history
- Assessing hormone-sensitive organ systems (prostate, breast, endometrium)
- Establishing IGF-1, GH, and glucose/insulin baselines
- Evaluating concurrent medications and medical conditions
The following table summarizes clinical risk categories:
| Risk Group | Criteria | Sermorelin Suitability |
| Low Risk | No personal/family cancer history, normal hormone levels | Safe with periodic monitoring |
| Moderate Risk | Controlled diabetes, family history of cancer | Use with enhanced endocrine tracking |
| High Risk | Previous hormone-sensitive cancer, genetic predisposition | Generally contraindicated |
| Active Cancer/Remission < 5 years | Ongoing treatment or recent remission | Not recommended |
Such risk stratification not only enhances patient safety but also helps tailor therapeutic strategies that align with the patient’s unique medical profile.

Long-Term Surveillance and Post-Treatment Monitoring
While Sermorelin is often administered in cycles of 3 to 6 months, its biological effects—especially on hormonal and cellular proliferation—can persist beyond the treatment window. This makes long-term surveillance essential, even in patients who tolerate the drug well initially.
For patients with any oncologic history or high baseline IGF-1, follow-up protocols typically include:
- Quarterly IGF-1 serum panels for 12 months after therapy
- Annual imaging of at-risk organ systems (e.g., prostate MRI, mammography)
- Cancer marker monitoring in genetically predisposed individuals
This proactive strategy allows for early detection of aberrant cellular activity and helps reduce long-term oncologic risk. It also aligns with clinical recommendations seen in studies discussing Unfavorable intermediate risk prostate cancer and related growth-hormone-sensitive malignancies.
Overlooked Symptoms That Could Signal a Cancerous Link
Certain side effects from Sermorelin are often dismissed as benign but may warrant further oncologic evaluation. Symptoms like unexplained fatigue, persistent joint pain, or localized swelling could be signs of hormone-sensitive tumor growth—especially in patients with silent risk markers.
For example, emerging evidence suggests that bone pain unresponsive to NSAIDs in patients using Sermorelin could reflect early myeloma flare. This warrants further investigation via imaging such as DEXA scans or skeletal surveys, even though DEXA alone cannot detect malignancy.
This underscores the importance of educating patients to recognize atypical symptoms and encouraging them to report them promptly.
Current Clinical Trials and Regulatory Perspectives on Sermorelin
As of 2025, Sermorelin is not FDA-approved for adult anti-aging or performance enhancement indications. Most prescriptions are off-label and managed through private longevity clinics or integrative health practices. However, ongoing trials are evaluating its role in:
- Sarcopenia prevention in aging men
- GH regulation in postmenopausal women
- Adjuvant recovery in chemotherapy patients
Although these studies do not yet establish clear links between Sermorelin and cancer promotion, regulators urge caution—particularly in populations with known colon cancer metastasis to the peritoneum, where cellular environments are already primed for growth. (ВСТАВИТЬ ССЫЛКУ НА COLON CANCER METASTASIS PERITONEUM)
The outcome of these trials will likely shape future guidelines, possibly introducing stricter eligibility criteria or new black-box warnings.
Is Sermorelin Safe for Patients at Cancer Risk?
Sermorelin is a potent modulator of the growth hormone/IGF-1 axis, which intersects with several critical cellular pathways. While it may offer therapeutic benefits in hormone-deficient patients, its use in populations with a history—or even a predisposition—to cancer must be approached with clinical precision.
Key takeaways:
- Sermorelin does not cause cancer directly but may exacerbate growth in hormone-sensitive tissues.
- Risk is stratified by genetics, personal history, and concurrent hormone use.
- Vigilant monitoring of IGF-1 and organ-specific markers is mandatory.
- Any off-label use should be supported by multidisciplinary medical oversight.
Patients and providers alike must weigh benefits against long-term risks. Until more data becomes available, the safest path is one grounded in clinical evidence, genetic insight, and cautious optimism.
FAQ
Can Sermorelin directly cause cancer?
No, Sermorelin itself does not directly cause cancer. However, it stimulates the production of growth hormone (GH), which in turn elevates insulin-like growth factor 1 (IGF-1). High IGF-1 levels have been associated with increased cellular proliferation, including in tissues that may already have oncogenic mutations. Thus, in genetically predisposed individuals or those with previous malignancy, caution is warranted.
What is the connection between Sermorelin and IGF-1?
Sermorelin acts by stimulating the pituitary gland to release natural GH, which then increases IGF-1 production in the liver. IGF-1 plays a central role in cell growth and survival. Elevated IGF-1 has been linked to several types of cancer, especially prostate, breast, and colorectal, due to its effect on mitogenic signaling pathways.
Who should not take Sermorelin due to cancer risks?
Patients with active cancers, a history of hormone-sensitive tumors, or a family history of cancers such as breast, prostate, or colon should consult an oncologist before considering Sermorelin. In some cases, genetic testing for BRCA or Lynch syndrome may be advised prior to therapy.
Can Sermorelin reactivate cancer in remission?
While data is limited, theoretical concerns suggest that increased IGF-1 from Sermorelin might stimulate residual malignant cells, especially in cancers that are known to be hormone-sensitive. Post-remission patients are generally advised to avoid hormone therapy without supervision.
What are the signs that Sermorelin might be causing a problem?
Unexpected symptoms like persistent fatigue, unexplained muscle or bone pain, swelling in soft tissues, or sudden weight changes should prompt a medical evaluation. These could indicate metabolic imbalances or the growth of abnormal tissue.
How does Sermorelin compare to other growth hormone therapies in terms of safety?
Sermorelin is generally considered safer than synthetic GH (somatropin) because it mimics natural physiology by stimulating the body’s own production. However, the end effect—higher IGF-1—is the same, so cancer-related risks are comparable depending on dosage and individual susceptibility.
Can Sermorelin be safely used in cancer survivors?
There is no consensus. Some clinicians use it in tightly controlled settings with extensive monitoring, especially in survivors of non-hormonal cancers. Others avoid it entirely in patients with a cancer history. Risk-benefit analysis is crucial.
Is there evidence linking Sermorelin to prostate cancer?
Studies have raised concerns about elevated IGF-1 contributing to prostate cell proliferation. While Sermorelin has not been directly tied to initiating prostate cancer, men with elevated PSA or a strong family history should be screened thoroughly before use.
Are women at particular risk when taking Sermorelin?
Yes, especially postmenopausal women who may have undetected hormone-sensitive tissue changes. Breast cancer risk is a concern, and any patient using hormone modulators must be monitored for mammographic changes and serum markers.
Can Sermorelin affect precancerous conditions like MGUS or adenomas?
Yes, there is theoretical concern that GH and IGF-1 stimulation could accelerate the transformation of conditions like MGUS (monoclonal gammopathy of undetermined significance) into multiple myeloma, or lead to the growth of benign adenomas into malignant forms.
What are the recommendations for monitoring Sermorelin users?
Patients should undergo baseline and follow-up IGF-1 testing, as well as annual imaging and lab tests based on individual risk factors. Those with prior cancer history may require more frequent and specialized follow-up, including oncologic input.
Can Sermorelin be used in patients with genetic cancer syndromes?
Generally, no. Patients with BRCA mutations, Li-Fraumeni syndrome, or familial adenomatous polyposis are at higher risk for early-onset cancers, and exogenous stimulation of growth hormone pathways could theoretically elevate this risk further.
How do lifestyle factors influence the risks of Sermorelin?
Diet, smoking, alcohol intake, and exercise all modulate endogenous hormone levels and oxidative stress. Sermorelin use in patients with unhealthy lifestyles may compound risk factors. Healthy habits reduce the chance of adverse responses.
Is Sermorelin safer in younger vs. older adults?
Younger individuals with natural GH deficiency may benefit more safely from therapy when monitored. In older adults, especially over 60, natural tumor suppressor mechanisms weaken, making unchecked cell growth more problematic if stimulated.
What alternatives exist to Sermorelin for aging support?
Alternatives include lifestyle interventions (sleep, resistance training, protein intake), non-hormonal peptides, or targeted supplementation. These approaches support wellness without activating hormonal pathways that may carry cancer risk.