Refusing Hormone Therapy for Breast Cancer: Understanding Risks, Reasons, and Outcomes
- What Is Hormone Therapy in Breast Cancer?
- Why Some Patients Refuse Hormone Therapy
- Medical Consequences of Skipping Hormone Therapy
- Comparing Long-Term Outcomes With and Without Hormone Therapy
- Psychological Factors Behind the Decision
- Doctor–Patient Communication Barriers
- Alternative Approaches Patients May Consider
- Personal Narratives and Case Reflections
- Risk of Cancer Recurrence Without Hormone Therapy
- Impact on Survival Rates
- When Symptoms Become Unbearable: Managing Side Effects
- Long-Term Monitoring Without Hormone Therapy
- Communication Gaps Between Patients and Physicians
- Postponed Therapy and Disease Recurrence
- Survival Outcomes Without Hormone Therapy
- Connection to Other Hormonal Pathways and Cancers
- FAQ
What Is Hormone Therapy in Breast Cancer?
Hormone therapy, often called endocrine therapy, is used to treat breast cancers that are sensitive to hormones like estrogen or progesterone. These cancers, labeled hormone receptor-positive, grow more rapidly in the presence of these natural body chemicals. Hormone therapy works by either blocking the cancer cells’ access to hormones or by reducing the body’s production of hormones altogether. Common medications include tamoxifen, used for both premenopausal and postmenopausal women, and aromatase inhibitors, which are primarily prescribed after menopause. These drugs are not chemotherapy—they do not kill cells outright but act over time to prevent recurrence or slow tumor growth. The typical course lasts five to ten years and is considered a long-term strategy aimed at relapse prevention. While highly effective, hormone therapy isn’t without controversy or challenges, and understanding its function is key before evaluating reasons to refuse it.
Why Some Patients Refuse Hormone Therapy
Many patients initially agree to hormone therapy but discontinue it early, while others decide to never start. The reasons are diverse and often deeply personal. Side effects remain the top concern, as hormone therapy commonly induces hot flashes, weight gain, insomnia, vaginal dryness, and fatigue. In some patients, these symptoms become so disruptive to daily life that quality of life is severely reduced. Others cite mental health impacts, such as anxiety and depression, which may be linked to estrogen reduction or to the overwhelming nature of a cancer diagnosis itself. Some patients have philosophical or naturalistic beliefs and prefer to avoid pharmaceuticals altogether. There are also fears surrounding the long-term commitment of daily medication for half a decade or more. Financial concerns play a role as well, especially in regions where prescription costs are not fully covered. These motivations, while not medically advised, are valid from a human perspective and deserve understanding and support.
Medical Consequences of Skipping Hormone Therapy
Refusing hormone therapy carries quantifiable risks that should not be underestimated. Hormone receptor-positive breast cancer, which makes up about 70% of all breast cancer cases, responds particularly well to hormonal treatment. Studies show that skipping or discontinuing this therapy nearly doubles the risk of recurrence within 10 years, even in early-stage cancer. Moreover, the protective benefit of hormone therapy continues even after stopping treatment, so not starting at all means losing both short- and long-term safety nets. The mortality rate is also higher among those who refuse it, especially in patients under the age of 50 with aggressive tumors. Another issue is that if the cancer returns, the options for subsequent treatment may be more invasive and less effective, often involving chemotherapy or surgeries with more side effects. It’s also important to mention that the decision to refuse may contribute to psychological distress—some patients later feel regret or anxiety about whether they made the right choice.
Comparing Long-Term Outcomes With and Without Hormone Therapy
To illustrate the impact of hormone therapy refusal, it’s helpful to look at data comparing two patient paths—those who undergo the treatment and those who opt out. Below is a table summarizing key differences:
| Outcome | With Hormone Therapy | Without Hormone Therapy |
| 5-Year Recurrence Risk | ~10–12% (depending on subtype) | ~20–25% |
| 10-Year Survival Rate | ~85–90% | ~70–75% |
| Common Side Effects | Hot flashes, fatigue, joint pain | None related to treatment |
| Long-Term Safety Net | Present (estrogen suppression) | Absent |
| Psychological Impact | Mixed: regret in some, relief in others | Mixed: initial relief, later anxiety |
As seen in the table, the differences are not minor. Hormone therapy improves survival and reduces recurrence significantly. However, those benefits must be weighed against the side effects and the lifestyle changes required during treatment. Some patients report reclaiming autonomy by refusing therapy, but this often comes with increased emotional burden, especially as the years pass without incident or with new symptoms. This decision is deeply personal, and a full understanding of the consequences is essential for patients and their families.
Psychological Factors Behind the Decision
Refusing hormone therapy is often rooted not only in physical side effects, but also in emotional complexity. The initial cancer diagnosis can leave patients overwhelmed, anxious, and unsure of their trust in medical systems. Many feel that taking a pill for years after the primary treatment is a constant reminder of their illness—a shadow that follows them long after remission. Others describe a need to reclaim control over their lives after feeling helpless during surgery, chemotherapy, or radiation. There’s also the influence of misinformation or misunderstanding: some patients overestimate their prognosis without therapy or believe that dietary or natural methods are equally protective. Cultural and generational values may also play a role. For example, patients from communities with skepticism toward pharmaceuticals are more likely to consider hormone therapy unnecessary. This mindset is not unique; similar cognitive resistance can be seen in cases involving other cancers, such as those explored in retroperitoneum cancer, where rare diagnoses create space for self-guided treatment choices.
Doctor–Patient Communication Barriers
One of the most overlooked reasons patients refuse hormone therapy is poor communication with their oncologist. In some cases, discussions about hormone therapy are rushed or occur during a time of heightened stress when patients are still processing surgery or chemotherapy. When the information is too technical, patients may misunderstand the intent or assume it’s optional. Some feel pressured rather than supported and disengage from the conversation entirely. Others are uncomfortable asking questions or revealing fears about intimacy, menopause, or mental health changes that may accompany hormonal manipulation. When communication is incomplete, the patient’s perception of risks and benefits becomes distorted. Building trust requires time, empathy, and tailored education—not generic pamphlets or brief consultations. It’s critical for medical teams to listen actively, offer ongoing dialogue, and provide resources that address the long-term realities of treatment adherence.
Alternative Approaches Patients May Consider
Some patients who decline hormone therapy turn to alternative therapies—ranging from dietary supplements and acupuncture to phytoestrogens and high-dose vitamins. While some of these options may improve comfort or reduce stress, there is currently no scientific evidence that they replace the protective effect of hormone therapy. In rare cases, patients pursue integrative care plans with the guidance of a naturopathic doctor in combination with oncological monitoring. However, the danger arises when these methods are chosen instead of evidence-based treatment. Even when tumors seem to be in remission, residual cancer cells may remain dormant and can become active over time, particularly in hormone-sensitive cancers. The term “natural” can be misleading, especially when untested substances interfere with the body’s endocrine system. Patients need to understand that declining therapy doesn’t mean opting for a different version of the same thing—it often means removing a crucial safeguard against recurrence. In many ways, the debate resembles the one surrounding biomarkers in conditions like high alkaline phosphatase cancer, where alternative explanations are sought for clinically significant patterns.
Personal Narratives and Case Reflections
Throughout clinical practice, there have been countless stories of women who declined hormone therapy for breast cancer. Some felt liberated by the decision, stating they wanted to prioritize the present over hypothetical future risks. Others lived for years without recurrence but eventually faced a resurgence of cancer and expressed regret that they hadn’t pursued every available treatment. In a few cases, patients refused initially but reconsidered after discussions with survivors or family members. It is also common for survivors to feel caught between two extremes: accepting treatment with burdensome effects or refusing and living with the fear of return. One particularly striking case involved a 45-year-old woman who declined tamoxifen due to fears of uterine cancer, but later expressed how much more frightening it was when her cancer recurred in a distant organ. These stories remind us that behind every data point is a life shaped by deeply human choices, and those choices unfold in complex psychological, medical, and social contexts. They also reinforce the importance of addressing patient needs holistically—something that’s being explored in newer studies related to the eukaryotic cell cycle and cancer response mechanisms.
Risk of Cancer Recurrence Without Hormone Therapy
Hormone therapy is specifically designed to target hormone receptor-positive breast cancer by either blocking estrogen receptors or reducing estrogen levels in the body. Without it, the underlying hormonal stimulation that can fuel dormant cancer cells remains unchecked. This significantly increases the likelihood of recurrence, particularly in the first five to ten years following initial treatment. Clinical studies consistently demonstrate that patients who decline hormone therapy face a notably higher risk of relapse compared to those who adhere to it. Moreover, recurrence in these cases may not occur in the breast alone but may manifest in distant organs such as the bones, lungs, or liver. These distant metastases often indicate a more aggressive progression and poorer prognosis. Physicians often emphasize that while hormone therapy cannot guarantee absolute protection, its statistical benefits far outweigh its side effects. Declining this line of defense is a decision that must be weighed with full understanding of the biological risk it invites.
Impact on Survival Rates
The refusal of hormone therapy not only affects recurrence risk but also has a direct impact on overall survival rates. For estrogen receptor-positive (ER+) breast cancers, adjuvant hormone therapy has been shown to reduce mortality by up to 30% over a decade. This is not a marginal difference—it is a cornerstone of long-term disease control. When patients choose not to undergo hormone therapy, they forgo this significant survival advantage. Survival curves from large-scale cohort studies show that the gap in survival begins to widen within the first few years post-diagnosis and continues to diverge with time. It’s crucial for patients to understand that hormone therapy isn’t just a preventive tool—it’s a statistically validated measure to extend life. Physicians often struggle to communicate this without sounding coercive, but the data speaks clearly. Choosing not to take hormone therapy means accepting a lower probability of long-term survival.

When Symptoms Become Unbearable: Managing Side Effects
The side effects of hormone therapy—hot flashes, mood changes, joint pain, and fatigue—are among the primary reasons patients discontinue or refuse treatment. These symptoms are real and often distressing, impacting quality of life in ways that can be difficult to articulate. However, it’s important to note that these effects can often be managed or reduced through tailored interventions. Dose adjustments, switching from one hormone therapy drug to another (such as from tamoxifen to an aromatase inhibitor), and incorporating supportive therapies like cognitive behavioral therapy, acupuncture, or physical activity have been shown to improve tolerance. Open communication with healthcare providers is key to finding a sustainable path forward. When symptoms are discussed honestly and early, the treatment plan can often be adapted to help patients stay on therapy without overwhelming their daily lives. In many cases, patients who initially refused hormone therapy returned to it later after proper symptom management was initiated.
Long-Term Monitoring Without Hormone Therapy
For patients who refuse hormone therapy, the follow-up care plan becomes significantly more intensive. Since hormone therapy acts as a suppressive mechanism against recurrence, its absence requires closer surveillance to catch potential relapse early. This includes more frequent physical exams, imaging studies, and bloodwork. Additionally, the emotional burden can be greater; patients often live with heightened anxiety, knowing they’ve declined a protective measure. Some oncologists recommend implementing lifestyle modifications and closer biomarker monitoring, though these are not substitutes for hormone therapy. It’s also essential to note that once recurrence occurs, treatment becomes more aggressive, and therapeutic options may be more limited. The strategy for those who forgo hormone therapy must be carefully structured, individualized, and consistently reviewed. Unlike standard survivorship plans, this approach depends more heavily on early detection and quick response to subtle changes, which may not always be evident without regular diagnostic procedures.
Communication Gaps Between Patients and Physicians
In many cases, the refusal of hormone therapy stems not from defiance but from misunderstanding. Oncologists may underestimate the emotional and informational needs of their patients, especially when trying to cover complex details in short visits. Conversely, patients may feel overwhelmed or hesitant to voice their true concerns. This creates a silent void where assumptions replace dialogue. When physicians use medical jargon or gloss over side effects, patients might interpret hormone therapy as dangerous or unnecessary. Clear, empathetic conversations can transform fear into trust. Regular check-ins, patient education sessions, and shared decision-making tools can improve adherence and help patients feel respected rather than pressured.
Postponed Therapy and Disease Recurrence
Delaying or skipping hormone therapy can have measurable consequences. For hormone receptor-positive breast cancers, each month of delay may slightly increase the risk of recurrence, especially in premenopausal women. The rationale behind this is rooted in the nature of how these cancers respond to estrogen. Without therapy, even microscopic residual cancer cells can be stimulated to grow over time. Moreover, if recurrence does occur, it may present more aggressively or with resistance to subsequent hormone therapy. While some patients consider postponement a temporary reprieve, clinicians should communicate that time-sensitive decisions can influence long-term survival.
Survival Outcomes Without Hormone Therapy
| Scenario | With Hormone Therapy | Without Hormone Therapy |
| 5-year recurrence risk (ER+) | ~10% | ~25% |
| 10-year survival (Stage I–II, ER+) | 85–92% | 70–78% |
| Risk of metastasis | Lower with treatment | Higher without intervention |
| Treatment resistance upon recurrence | Less likely | More likely |
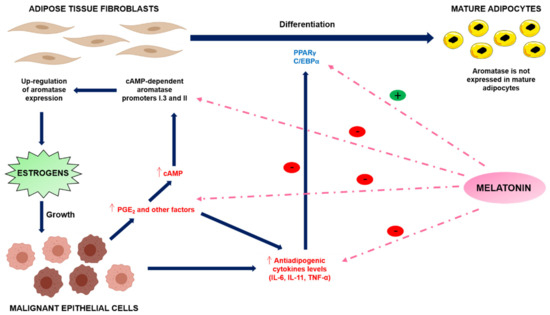
Connection to Other Hormonal Pathways and Cancers
Refusing hormone therapy in breast cancer may also be linked to deeper concerns about hormonal influence across other cancers. Some women worry that manipulating estrogen could affect future hormonal balance, fertility, or increase susceptibility to unrelated hormone-sensitive conditions. These fears often arise after reading conflicting studies about hormone therapy’s relationship with other cancers or cellular processes. In fact, similar concerns arise in studies related to cell proliferation seen in hormone-sensitive tumors, such as those explored in the eukaryotic cell cycle and cancer in depth. Addressing these multidimensional concerns requires both medical facts and compassionate understanding of each patient’s journey.
FAQ
What are the most common reasons patients refuse hormone therapy for breast cancer?
Many patients refuse hormone therapy due to fear of side effects such as hot flashes, mood swings, and bone loss. Others may be concerned about long-term health risks, like endometrial cancer or cardiovascular disease. A lack of clear communication with their medical team can also leave patients confused or mistrustful about the benefits of treatment.
Is it dangerous to refuse hormone therapy after breast cancer surgery?
Yes, particularly for hormone receptor-positive breast cancer. Hormone therapy significantly reduces the risk of recurrence by suppressing estrogen’s effect on cancer cells. Refusing it may leave microscopic cancer cells untreated, increasing the likelihood of the cancer returning or spreading.
Can lifestyle changes replace hormone therapy?
While healthy lifestyle habits like diet, exercise, and stress management support overall recovery and reduce general cancer risk, they are not a substitute for hormone therapy. These approaches lack the targeted biological mechanism that hormone therapy uses to block or lower estrogen levels.
What happens if I stop hormone therapy early?
Stopping early can reduce the protective benefits of the treatment. Studies have shown that completing the full 5–10 years of therapy significantly reduces recurrence risk, especially in hormone receptor-positive cases. Ending treatment prematurely may result in higher chances of cancer returning.
How long does hormone therapy last for breast cancer?
Standard hormone therapy typically lasts five to ten years. The duration depends on individual factors like cancer stage, menopausal status, and tolerance of side effects. For some high-risk patients, extended therapy beyond five years may be recommended.
Are the side effects of hormone therapy manageable?
Most side effects can be managed with adjustments to medication, lifestyle interventions, or supportive therapies. For instance, hot flashes may be eased with non-hormonal medications or acupuncture, and bone loss can be monitored and treated with supplements or medications.
Can hormone therapy cause other cancers?
This is a common concern. Some forms of hormone therapy, like tamoxifen, may slightly raise the risk of uterine cancer, particularly in postmenopausal women. However, the overall benefits often outweigh the risks, and regular monitoring helps detect any complications early.
Does hormone therapy affect fertility?
Yes, particularly in premenopausal women. Some hormone therapies may suppress ovulation during treatment. However, fertility can often return after therapy ends. Women concerned about fertility should consult their oncologist about preservation options before starting treatment.
Can you switch hormone therapy drugs if side effects are severe?
Yes, many patients successfully switch between different types of hormone therapies, such as from tamoxifen to aromatase inhibitors or vice versa. Oncologists often tailor treatments to balance effectiveness with tolerability.
What’s the risk of recurrence without hormone therapy?
The risk varies depending on cancer stage, receptor status, and other treatments received. However, in hormone receptor-positive patients, not taking hormone therapy can double the risk of recurrence compared to those who complete therapy.
How soon should hormone therapy start after surgery or radiation?
Typically, hormone therapy begins within weeks of completing surgery, chemotherapy, or radiation. Starting promptly helps reduce the risk of leftover cancer cells responding to circulating hormones.
What should I do if I regret refusing hormone therapy?
It’s not too late to talk to your doctor. Depending on how much time has passed, you may still be able to start hormone therapy or take alternative measures to reduce recurrence risk. Open communication with your care team is key.
Does age affect the benefits of hormone therapy?
Both younger and older women benefit from hormone therapy, though drug selection and side effect management may differ. Postmenopausal women often receive aromatase inhibitors, while tamoxifen is more common in younger patients.
Are there natural alternatives to hormone therapy?
No natural treatments have been proven to match the effectiveness of prescribed hormone therapies in reducing breast cancer recurrence. Some supplements may interact with treatment or mimic estrogen, so always consult your doctor before using them.
Can counseling help patients stick with hormone therapy?c
Absolutely. Psychosocial support, cognitive behavioral therapy, and patient education can improve adherence by addressing anxiety, misconceptions, and emotional barriers related to treatment. A supportive care plan often increases therapy success.









