Reducing Redness on Face: Medical and Everyday Strategies
Causes of Redness on Face and Why It Happens
Redness on face, or facial erythema, occurs when the skin’s blood vessels widen and allow more blood to flow near the surface. While often harmless, persistent redness can be uncomfortable or distressing and may signal an underlying condition. Understanding how and why redness appears helps determine the most effective way to control it.
Not Just Rosacea: The Many Causes of Redness
Rosacea is one of the most common chronic causes of redness, typically affecting the cheeks, nose, chin, and forehead. However, not all redness is rosacea. Other skin disorders-such as seborrheic dermatitis, acneiform eruptions, and eczema-can also cause visible redness, irritation, or blotchiness. In some cases, redness is a temporary response to sun exposure, heat, or emotional stress, while in others it may result from reactions to topical medications or systemic conditions.
- Chronic causes: Rosacea, seborrheic dermatitis, acneiform eruptions, eczema.
- Temporary causes: Sun exposure, heat, emotional stress.
- Other triggers: Reactions to topical products, medications, or systemic conditions.
Because redness can arise from such diverse causes, identifying the underlying trigger is essential. What appears as mild flushing in one person could reflect inflammation or a vascular response in another. A careful assessment of symptoms, duration, and triggers helps clarify whether redness is short-lived or part of a chronic process.
How the Skin Turns Red
Redness develops when small blood vessels in the skin dilate, allowing increased blood flow. This process, known as vasodilation, is part of the body’s normal temperature regulation and inflammatory response. In chronic redness on face, these vessels may become overly reactive-a phenomenon called vascular hyperreactivity-causing the skin to appear red even without clear provocation. Inflammation and barrier dysfunction further amplify this process by weakening the skin’s natural defenses and increasing sensitivity to external irritants.
Over time, repeated dilation can lead to visible capillaries or a background flush that no longer fades completely. This physiological cycle helps explain why some individuals experience persistent redness while others only flush briefly.

Common Culprits
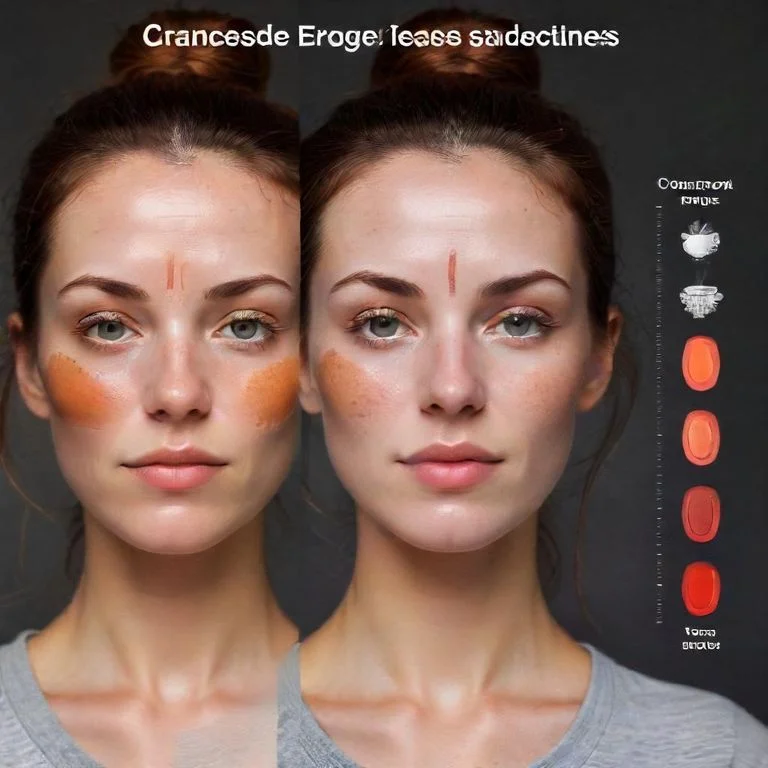
Several conditions and external factors can contribute to redness on face. Rosacea often produces central facial redness along with small bumps or visible vessels. Seborrheic dermatitis may create patchy redness with flaking, especially around the nose and eyebrows. Sunburn and windburn cause temporary inflammation due to environmental exposure, while reactions to skincare products or medications can lead to irritation or contact dermatitis. Occasionally, redness reflects internal or drug-induced processes that need medical evaluation.
- Rosacea: Central redness, bumps, or visible vessels.
- Seborrheic dermatitis: Patchy redness with flaking.
- Sunburn/Windburn: Temporary inflammation from environmental exposure.
- Product or drug reactions: Irritation or contact dermatitis.
Because facial erythema can have multiple overlapping causes, it is important to view redness as a symptom rather than a diagnosis. Distinguishing between these possibilities allows for more accurate treatment and better control of chronic redness.
Recognizing Facial Redness Patterns, Symptoms, and Triggers
Redness on face can appear in many forms, ranging from brief flushing to constant discoloration that persists throughout the day. Recognizing how redness behaves-when it comes and goes, what triggers it, and what other symptoms appear-helps distinguish between occasional irritation and a chronic skin condition. Understanding these patterns is an important step toward effective management and accurate diagnosis.
Flushing vs Constant Redness
Facial erythema can present as short-term flushing or as persistent background redness. Flushing episodes often occur suddenly and fade after the trigger passes, such as after heat exposure, embarrassment, or spicy food. In contrast, persistent redness may remain visible for weeks or months and may include fine, dilated blood vessels or patchy discoloration. Chronic redness can also occur with small bumps or pustules, particularly in rosacea, or with thickening of the skin in more advanced cases.
- Flushing: Sudden and short-lived redness that fades once the trigger subsides.
- Persistent redness: Long-lasting redness that can include visible blood vessels, bumps, or thickened skin.
Distinguishing between these two patterns helps doctors identify whether the redness is a temporary vascular response or a sign of ongoing inflammation. Persistent redness is more likely to involve structural changes in the skin and blood vessels, making it less responsive to simple trigger avoidance alone.
Other Symptoms You Might Notice
Facial redness is often accompanied by other symptoms that provide diagnostic clues. Some people experience burning, stinging, or a sensation of warmth in the affected areas. In rosacea, visible blood vessels, known as telangiectasias, may become apparent, and the skin can develop small inflammatory bumps. Ocular involvement-such as dryness, redness, or irritation of the eyes-can also occur in some individuals and is an important sign of a more complex form of the condition. In some cases, thickening of the skin around the nose, known as phymatous change, may develop over time.
- Burning, stinging, or warmth on the skin
- Visible blood vessels (telangiectasias)
- Inflammatory bumps or pustules
- Eye redness or irritation (ocular symptoms)
- Thickening of the skin around the nose (phymatous changes)
Recognizing these additional features helps differentiate facial redness from other transient or surface irritations, guiding clinicians toward the most appropriate evaluation and treatment plan.
Everyday Triggers for Redness on Face
Many environmental and lifestyle factors can make redness on face worse, even in otherwise mild cases. Common triggers include sun exposure, extreme temperatures, hot drinks, spicy foods, alcohol, and emotional stress. These stimuli cause temporary dilation of facial blood vessels, leading to increased warmth and redness. Repeated exposure to these triggers may heighten vascular reactivity, making the redness more pronounced or longer lasting over time.
- Sun exposure or wind
- Hot drinks and spicy foods
- Alcohol consumption
- Emotional stress or anxiety
- Extreme heat or cold
In addition, certain skincare products and medications can aggravate sensitive skin. Topical corticosteroids, harsh cleansers, or heavily fragranced products may cause or intensify irritation, especially in those with an impaired skin barrier. Being aware of such triggers allows individuals to make small adjustments that reduce flare-ups and discomfort while seeking medical evaluation when necessary.
Who Gets Facial Redness and When to Seek Medical Help
Redness on face can affect anyone, but some people are more prone to developing persistent or chronic redness. Understanding who is at higher risk and when to seek medical evaluation helps differentiate normal skin reactions from conditions that require targeted treatment or further investigation.
Who’s Most Affected
Rosacea is a leading cause of chronic facial redness and commonly affects adults who experience lasting redness in the central areas of the face, such as the cheeks, nose, chin, and forehead. It tends to occur more frequently in individuals with sensitive skin and those prone to flushing. While it can affect all skin types, some patterns and subtypes are more commonly seen in certain demographic groups, depending on skin phototype and genetic background. The condition usually develops gradually and may worsen over time if triggers or inflammation remain uncontrolled.
- Most common in adults: Especially those with persistent redness in central facial areas.
- More frequent in sensitive skin types: Individuals prone to flushing or reactivity.
- Varies by skin tone and genetics: Certain rosacea subtypes appear more often in specific phototypes or populations.
Chronic redness can also appear alongside other features like visible blood vessels or thickened skin, particularly in adults. Identifying these patterns helps clinicians distinguish rosacea and similar conditions from short-term redness caused by environmental or irritant factors.
How Doctors Investigate Redness
When redness on face persists, doctors take a structured approach to determine its cause. They begin with a detailed history-asking about when the redness started, how long it lasts, where it appears, and what factors make it worse or better. Additional questions may focus on associated symptoms such as burning, eye irritation, or thickening of the skin. Reviewing medications, skincare habits, and systemic symptoms helps narrow down potential triggers or related conditions.
- Onset, duration, and distribution of redness
- Associated symptoms such as burning or eye irritation
- Medication use and skincare products
- Environmental or emotional triggers
- Presence of systemic signs (fever, swelling, or pain)
During a physical examination, clinicians look for visible blood vessels, bumps, or textural changes in the skin. Distinguishing between temporary flushing and long-standing redness allows for a more focused diagnosis and avoids unnecessary testing. If symptoms suggest a systemic or more serious underlying problem, further evaluation or referral to a specialist may be warranted.
When to See a Doctor
- Redness that spreads or worsens despite basic care
- Thickened or bumpy skin around the nose
- Eye symptoms such as dryness, irritation, or vision changes
- Systemic symptoms including fever, joint pain, or swelling
Persistent, progressive, or atypical facial redness should prompt a medical evaluation. These features may signal underlying inflammation or a condition beyond common skin sensitivity and should be assessed by a healthcare professional.

Effective Treatments and Everyday Management for Redness on Face
Redness on face can be effectively reduced with a combination of medical therapies, procedural options, and practical daily strategies. While most forms of chronic redness cannot be fully cured, consistent treatment and trigger control can lead to substantial improvement in both appearance and comfort. Managing redness successfully often involves addressing inflammation, supporting the skin barrier, and targeting visible vascular changes when necessary.
Topical and Oral Treatments
Evidence-based treatment for redness on face typically begins with prescription topical medications designed to calm inflammation or reduce excessive blood flow in the skin. These formulations may include anti-inflammatory agents that target the underlying redness and irritation seen in rosacea or other chronic conditions. For patients with more pronounced symptoms or persistent inflammatory lesions, oral medications may be used to further suppress inflammation or modulate vascular reactivity.
- Topical therapies: Anti-inflammatory or vasoconstrictive creams and gels that reduce redness and irritation.
- Oral medications: Used when inflammation is more extensive or involves deeper vascular changes.
- Combination approach: Often combines topical and systemic therapies for better symptom control.
Therapeutic choices depend on the pattern and severity of redness, as well as the presence of associated bumps or sensitivity. Because chronic redness reflects a combination of vascular and inflammatory mechanisms, treatment plans often combine topical care with systemic therapies to maximize control and minimize flare-ups.
Laser and Light Therapy
When redness persists despite medical therapy, laser and light-based treatments can help by directly targeting dilated blood vessels and diffuse erythema. Devices such as pulsed-dye or intense pulsed light systems emit controlled energy that selectively heats and collapses small vessels near the skin’s surface, leading to gradual fading of visible redness over multiple sessions. These approaches are particularly effective for telangiectasias and background vascular redness that do not respond fully to medication.
- Laser options: Pulsed-dye and other vascular lasers that precisely target blood vessels.
- Light-based systems: Intense pulsed light (IPL) for diffuse redness and overall tone improvement.
- Expected results: Gradual fading of visible redness with multiple treatments and minimal downtime.
While not a permanent cure, these procedures offer long-lasting cosmetic and symptomatic improvement. They are best performed by experienced dermatology professionals and can be combined with ongoing medical therapy and trigger management to maintain results.
Lifestyle Adjustments That Help
Daily habits play an important role in keeping redness on face under control. Avoiding known triggers-such as prolonged sun exposure, extreme temperatures, hot drinks, spicy foods, alcohol, and emotional stress-can significantly reduce flare frequency. Using gentle, fragrance-free cleansers and moisturizers helps protect the skin’s barrier and limit irritation.
- Identify and avoid common triggers like heat, sunlight, spicy food, and alcohol.
- Use mild, non-fragranced skincare products.
- Apply broad-spectrum sunscreen daily.
- Maintain consistent skincare and stress management routines.
Consistent use of broad-spectrum sunscreen is also essential, as ultraviolet light is a frequent aggravating factor in chronic redness. By combining these lifestyle adjustments with prescribed treatments, individuals can achieve steady improvement and better long-term skin stability.

Living Well With Redness on Face
Redness on face can be more than a physical concern-it often affects how people feel about their appearance and interact socially. Long-term redness, especially when visible or difficult to conceal, can influence confidence, social comfort, and emotional well-being. Recognizing these effects is an important part of overall care and supports a balanced approach that combines medical treatment with emotional resilience.
Emotional and Social Effects
Persistent facial redness can lead to self-consciousness, frustration, or embarrassment, particularly in social or professional settings. Many individuals report avoiding public situations or altering routines because of concerns about how others perceive their skin. These feelings are valid and understandable-chronic skin conditions are known to carry a psychological burden similar to other long-term health issues.
- Feelings of self-consciousness or social withdrawal
- Impact on confidence or daily interactions
- Increased stress or frustration during flare-ups
Seeking reassurance from healthcare providers, support groups, or mental health professionals can be beneficial. Addressing the emotional side of redness on face alongside physical treatment helps improve quality of life and fosters a sense of control and confidence in managing the condition.
Myth vs Fact: Can It Be Cured?
| Myth | Fact |
|---|---|
| Redness on face is a permanent condition that cannot improve, no matter what you do. | While chronic redness such as rosacea cannot always be fully cured, it can be effectively managed with evidence-based treatments and consistent care. |
Understanding that improvement, not perfection, is the realistic goal can reduce frustration and set healthier expectations. With ongoing care, most individuals can achieve clearer, more comfortable skin and live confidently despite occasional flare-ups.

Frequently Asked Questions About Redness on Face
- Is facial redness always caused by rosacea?
- No. While rosacea is a common cause, redness on face can also stem from dermatitis, eczema, sunburn, or reactions to skincare products and medications.
- Can stress really make facial redness worse?
- Yes. Emotional stress can trigger blood vessel dilation and inflammation, which may temporarily worsen redness or flushing in sensitive skin.
- Why does my face turn red after drinking alcohol or eating spicy food?
- These triggers cause blood vessels to expand, increasing blood flow to the surface of the skin and creating visible facial redness.
- When should I see a doctor about persistent redness?
- Seek medical advice if redness lasts for weeks, worsens despite care, or appears with eye irritation, swelling, or thickened skin.
- Can skincare products make redness on face worse?
- Yes. Products containing fragrance, alcohol, or harsh cleansers can irritate the skin barrier and intensify facial redness or discomfort.
- What treatments help reduce chronic redness?
- Dermatologists often recommend topical or oral anti-inflammatory medications, laser therapy, and trigger management to control inflammation and visible redness.
- Does sun exposure affect facial redness?
- Ultraviolet light is a frequent trigger that can worsen redness and irritation, making daily sunscreen use an important part of prevention.
- Is redness on face curable?
- While chronic redness such as rosacea cannot be fully cured, most people see significant improvement with consistent treatment and lifestyle adjustments.
- Can changes in weather affect redness?
- Yes. Sudden temperature shifts, cold winds, or heat can all provoke flushing and increase visible redness, especially in sensitive skin.
- Does facial redness affect mental well-being?
- Persistent redness can impact self-esteem and social comfort, which is why addressing both physical and emotional aspects of care is important.













