Pili Multigemini and Cancer: Debunking Myths About a Rare Hair Follicle Condition
- Pili Multigemini and Cancer: Separating Fact from Fiction
- Histological Features of Pili Multigemini
- Differentiating Pili Multigemini from Skin Cancers
- Can Pili Multigemini Transform into Cancer?
- Common Diagnostic Challenges and Misidentification
- Genetic and Developmental Factors Behind Pili Multigemini
- Associations with Other Dermatologic Conditions
- Comparison of Pili Multigemini and Follicular Tumors
- Clinical Presentation and Areas Commonly Affected
- When to Seek Medical Advice
- Current Treatment Options and Cosmetic Management
- Psychological Impact and Cosmetic Anxiety
- Medical Literature and Case Report Summary
- Patient Experiences and Public Misunderstanding
- Differentiating Follicular Anomalies: Why Terminology Matters
- Final Summary: Is There a Cancer Link?
- FAQ: Pili Multigemini and Cancer – 15 Essential Answers
Pili Multigemini and Cancer: Separating Fact from Fiction
Understanding Pili Multigemini: A Rare Hair Follicle Condition
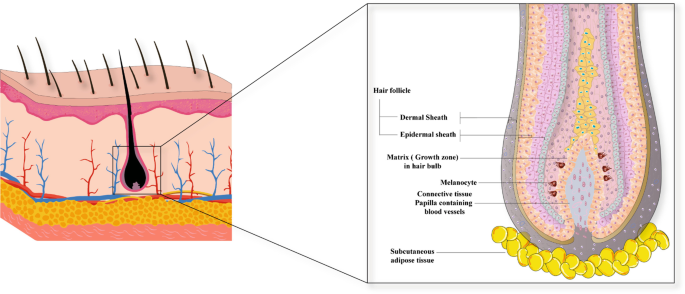
Pili multigemini is a rare and benign dermatological condition where multiple hair shafts emerge from a single follicular opening. Unlike typical hair follicles that produce one hair strand, pili multigemini can generate two or more shafts, often tightly packed and emerging as a cluster. This anomaly occurs due to the partial subdivision of the dermal papilla during embryonic development or hair follicle regeneration, leading to multiple hair matrices within a single outer root sheath.
Most commonly found on the beard area in men, upper back, or thighs, it is often discovered incidentally during shaving or routine dermatological exams. It may be asymptomatic or cause mild irritation, folliculitis, or cosmetic concerns. Importantly, pili multigemini is not considered harmful and is not inherently malignant. However, due to its unfamiliar appearance, it can sometimes be mistaken for more serious skin conditions by both patients and clinicians.
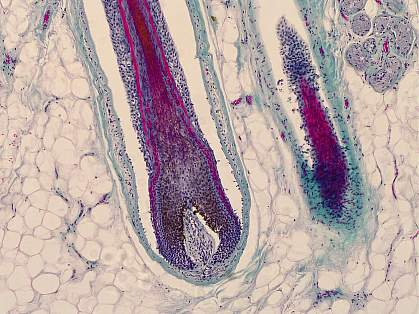
Histological Features of Pili Multigemini
To understand why pili multigemini is not cancerous, it’s important to look at its microscopic features. Histologically, it is characterized by multiple hair shafts enclosed within a single outer root sheath, originating from a shared follicular canal. Under the microscope, one can observe that each hair matrix in the follicle is independent but arises from the same dermal papilla structure. This distinguishes it from polytrichia (closely adjacent follicles) and more serious follicular tumors.
The individual hair shafts are usually of similar diameter and stage of growth (anagen), and the follicular unit maintains a benign architecture. There is no evidence of cellular atypia, invasion, or dysplasia—features typical of malignancies. Moreover, pili multigemini lacks mitotic figures, abnormal keratinization, or proliferation markers. These microscopic details affirm its status as a structural anomaly rather than a neoplastic process.
Differentiating Pili Multigemini from Skin Cancers
The confusion between pili multigemini and cancer arises mainly due to visual similarity with other dermatological lesions. In particular, certain hair follicle tumors such as trichoblastoma, pilomatricoma, or even basal cell carcinoma may have overlapping surface features. However, clinical differentiation can typically be made through dermoscopy and confirmed by histopathology.
Pili multigemini usually presents as multiple fine hairs from a single pore, often surrounded by normal-appearing skin, without ulceration, pigmentation, or infiltration. Malignant lesions, by contrast, tend to exhibit asymmetry, irregular borders, color variation, and architectural distortion. When doubt persists, a punch biopsy provides definitive diagnostic clarity, confirming benign follicular hyperplasia rather than malignant proliferation.

Can Pili Multigemini Transform into Cancer?
This question arises from a broader concern about whether chronic or structural skin conditions could potentially evolve into cancerous lesions. Currently, there is no scientific or clinical evidence to suggest that pili multigemini has malignant potential. Unlike premalignant conditions such as actinic keratosis or dysplastic nevi, pili multigemini lacks the hallmarks of cellular dysregulation. It does not show increasing proliferation, architectural disruption, or progression over time.
Longitudinal dermatological studies and case reports consistently describe pili multigemini as stable and non-progressive. In fact, many patients live with the condition for decades without experiencing any change in appearance or health status. No published data links this follicular anomaly with basal cell carcinoma, squamous cell carcinoma, or melanoma. Therefore, from a clinical standpoint, there is no rationale to treat or excise pili multigemini unless for cosmetic reasons or if recurrent inflammation occurs.
Common Diagnostic Challenges and Misidentification
When Visual Similarity Leads to Misdiagnosis
Despite its benign nature, pili multigemini is often misdiagnosed, primarily due to its rare occurrence and unusual presentation. Many dermatologists may encounter it only a few times in their careers, which can lead to confusion with other follicular anomalies or even early signs of cutaneous malignancies. For example, a cluster of emerging hair shafts from a single follicular unit may resemble pigmented basal cell carcinoma (BCC) if observed without dermoscopy, particularly if accompanied by inflammation or irritation.
Additionally, in patients with underlying inflammatory skin disorders like acne conglobata or folliculitis decalvans, the presence of pili multigemini may be overshadowed or mistakenly attributed to those primary conditions. Some patients, especially those with obsessive skin-checking habits or health anxiety, may present pili multigemini lesions with concern over “skin cancer,” creating diagnostic stress. These factors underscore the need for careful dermoscopic evaluation, pattern recognition, and, if warranted, a confirmatory skin biopsy to rule out atypical cell proliferation.
Genetic and Developmental Factors Behind Pili Multigemini
Why Multiple Hair Shafts Emerge From a Single Follicle
Pili multigemini is believed to originate from anomalies during embryological development of the hair follicle. Each follicle normally forms from an invagination of the epidermis into the dermis, guided by interactions between the dermal papilla and the follicular epithelium. In the case of pili multigemini, there is either a duplication or partial segmentation of the dermal papilla during early morphogenesis. This leads to several concentric hair matrix units developing in tandem within a shared outer root sheath.
Although no specific gene mutations have been identified to date, familial cases and reports of bilateral symmetry suggest that hereditary or epigenetic factors may be involved. Some studies hypothesize that local disruptions in signaling molecules—such as sonic hedgehog (SHH), Wnt, and BMP pathways, which are key in follicular morphogenesis—could play a role. However, this remains speculative and unconfirmed in large-scale studies.
In contrast to neoplastic skin lesions, which involve unchecked cellular proliferation and mutation accumulation, pili multigemini develops from stable, organized follicular structures. It behaves more like a congenital anomaly than a progressive disease process.
Associations with Other Dermatologic Conditions
Comorbid Skin Features That May Coexist
While pili multigemini is not linked directly to cancer, it has been observed alongside several non-malignant skin disorders. Patients with keratosis pilaris, folliculitis, or seborrheic dermatitis may occasionally present with this condition, particularly on the upper arms, back, or thighs. Whether this coexistence is incidental or due to shared structural anomalies of the follicular unit remains unclear, as research is limited.
Additionally, there have been scattered reports of pili multigemini in individuals with syndromes that affect ectodermal structures (e.g., hair, nails, teeth), though the correlation is tenuous. It’s essential to understand that these associations do not suggest causality or malignancy but highlight the importance of full-skin assessment when such anomalies are present.
In patients receiving chemotherapy, radiotherapy, or immunosuppressive therapy, temporary changes in hair follicle behavior may mimic features of pili multigemini, including distorted or clustered regrowth. However, this represents a treatment-related effect rather than true structural duplication of the follicle. “7 symptoms of colon cancer in women” – as a reminder of the importance of recognizing alarming symptoms and distinguishing benign conditions from potentially malignant ones.
Comparison of Pili Multigemini and Follicular Tumors
| Feature | Pili Multigemini | Trichoblastoma | Basal Cell Carcinoma (BCC) | Pilomatricoma |
| Nature | Benign hair follicle anomaly | Benign follicular tumor | Malignant skin tumor | Benign calcifying follicular tumor |
| Appearance | Clustered hair from one follicle | Flesh-colored or pigmented nodule | Pearly or ulcerated lesion | Hard, deep-seated nodule |
| Onset | Congenital or acquired | Slow-growing | May arise de novo or from sun damage | Often in children/adolescents |
| Risk of Cancer | None | None | High if untreated | Very low |
| Diagnostic Method | Dermoscopy or biopsy if unclear | Biopsy | Clinical + biopsy confirmation | Biopsy with calcification signs |
| Histopathology | Multiple hair shafts in single sheath | Basaloid cell proliferation | Peripheral palisading, retraction | Shadow cells, calcification |
This comparison illustrates the clear diagnostic boundaries between pili multigemini and actual neoplastic entities, supporting the view that it does not require aggressive investigation unless atypical features arise.
Clinical Presentation and Areas Commonly Affected
Where and How Pili Multigemini Manifests on the Body
Pili multigemini typically presents as multiple fine hair shafts emerging from a single follicular opening. These hair groupings may appear thicker or darker due to the close clustering and often go unnoticed until the area is shaved, inflamed, or evaluated with dermoscopy. In many patients, it does not cause any symptoms unless accompanied by irritation, folliculitis, or cosmetic concern.
The most frequently affected anatomical regions include the beard area (particularly in men), upper back, neck, thighs, and occasionally the scalp. In females, it may be more subtle and discovered incidentally during cosmetic treatments such as waxing or laser hair removal. The density and visibility of pili multigemini can vary widely between individuals, and in some cases, it appears as an isolated patch rather than widespread distribution.
Despite its striking appearance under magnification, the lesion is typically surrounded by healthy, unpigmented skin. There is no associated redness, scale, or ulceration unless secondary inflammation or trauma occurs. Because of this, many cases remain undiagnosed unless brought to medical attention out of concern for a skin abnormality.

When to Seek Medical Advice
Understanding What Warrants Clinical Evaluation
Although pili multigemini is a benign and non-progressive anomaly, there are instances when a dermatological consultation is appropriate. Any sudden change in appearance, such as ulceration, rapid growth, bleeding, or pigmentation, should prompt professional evaluation to rule out malignancy. While pili multigemini itself does not become cancerous, coincidental development of other lesions nearby cannot be excluded without a thorough assessment.
Patients experiencing chronic irritation, repeated follicular infections, or cosmetic distress may also seek treatment options. In some individuals, frequent shaving over the affected area can lead to pseudofolliculitis or ingrown hairs due to the dense and abnormal follicular pattern. These cases can benefit from targeted skin care, laser therapy, or, in rare cases, follicular ablation.
It’s also vital to educate patients about what pili multigemini is not: it is not an infection, not a contagious condition, and not a form of skin cancer. However, because some cancer-related skin changes also start subtly, maintaining a low threshold for clinical review when any lesion evolves remains a prudent approach. “can cancer cause low phosphate levels” – As with electrolyte imbalances, some skin symptoms may seem minor but require attention.
Current Treatment Options and Cosmetic Management
Addressing Aesthetic Concerns and Symptom Relief
Since pili multigemini is non-malignant and usually asymptomatic, treatment is not medically necessary in most cases. However, for patients distressed by its appearance or experiencing skin discomfort, several therapeutic avenues may be considered. Topical therapies like keratolytics (e.g., urea, salicylic acid) may help reduce follicular keratin buildup and prevent secondary folliculitis. Antibacterial cleansers or short courses of topical antibiotics may be useful if inflammation is present.
Laser hair removal using selective photothermolysis (especially diode or Nd:YAG lasers) has shown good results in reducing hair shaft density and minimizing recurrence. By targeting the follicular unit, laser therapy can suppress regrowth, particularly in high-density or visibly clustered regions. This method is often chosen by individuals with recurrent shaving bumps or cosmetic dissatisfaction.
In rare and resistant cases, minor surgical options such as follicular ablation or electrocoagulation may be discussed, although they carry a higher risk of scarring. Patient education remains central to management, helping individuals differentiate harmless anomalies like pili multigemini from more serious dermatologic threats.
Psychological Impact and Cosmetic Anxiety
Understanding the Emotional Repercussions of a Benign Condition
Even though pili multigemini is medically harmless, its presence can lead to considerable psychological discomfort, especially in individuals concerned about skin appearance or health. In societies where hair density, distribution, and grooming are closely tied to aesthetic norms, an unusual pattern like clustered hair shafts can draw attention or self-consciousness. This is particularly relevant for lesions on visible areas like the face or neck.
Patients may express anxiety about whether the condition is contagious, cancerous, or indicative of a more serious illness. Others may fear social judgment or become preoccupied with cosmetic correction. In dermatology, this aligns with a broader understanding of how benign conditions—like acne, vitiligo, or even benign moles—can carry emotional weight disproportionate to their physical impact.
Clear communication from healthcare providers is essential in these scenarios. Emphasizing that pili multigemini poses no threat to health, does not require excision, and can be improved cosmetically may offer reassurance. When anxiety persists or interferes with quality of life, referral to a psychologist or counselor experienced in body image disorders may be helpful.
Medical Literature and Case Report Summary
What the Scientific Community Has Documented
Although pili multigemini remains a relatively under-researched anomaly, it has been acknowledged in medical literature through case reports, dermatological reviews, and occasional textbook mentions. These reports consistently highlight its benign and non-proliferative nature, reaffirming that it is a structural variation rather than a pathological process. In several cases, patients presented with this condition alongside other follicular abnormalities or after routine skin exams.
No documented case has ever confirmed malignant transformation of pili multigemini. Histological analyses from biopsies show structurally organized follicular units with no signs of cellular atypia, mitotic activity, or invasive behavior. Case studies further emphasize that most patients are young adults or middle-aged individuals who notice the condition during grooming or treatment for unrelated skin concerns.
A handful of articles also explore its cosmetic impact and the use of laser hair reduction as a non-invasive treatment. Overall, the scientific consensus is clear: pili multigemini is benign, visually distinct, and completely unrelated to cutaneous carcinomas.
Patient Experiences and Public Misunderstanding
Why Clarity and Awareness Still Matter
Despite the clear evidence of benignity, many patients encountering pili multigemini for the first time experience anxiety, largely due to its unusual appearance and low public awareness. Online forums and unverified sources often contribute to misinformation, where clustered hair growth is incorrectly associated with cancer, parasites, or rare skin diseases.
Patients frequently report concern that the condition might be contagious, worsening over time, or indicative of a compromised immune system. These fears are amplified in those with a personal or family history of skin cancer or chronic skin conditions. Unfortunately, in the absence of accessible dermatological advice, many turn to cosmetic removal or harsh exfoliation, which can worsen inflammation or cause scarring.
To counteract this, healthcare professionals should prioritize education and reassurance. Sharing visual references, histological data, and patient-centered management plans helps bridge the gap between clinical facts and public misconceptions. Greater visibility in dermatological platforms and academic databases can also reduce confusion.
Differentiating Follicular Anomalies: Why Terminology Matters
Avoiding Confusion with Similar Conditions
Pili multigemini is often confused with other follicular disorders such as polytrichia, compound follicles, or even trichostasis spinulosa. Each of these conditions presents differently under both clinical examination and histopathology, but to an untrained eye, the differences can be subtle.
Polytrichia involves several follicles growing in close proximity rather than multiple shafts from a single follicle. Trichostasis spinulosa, by contrast, refers to the retention of multiple telogen-phase hairs in a single follicular opening, often accompanied by keratin plugs. Meanwhile, compound follicles can be a normal anatomic variant or may arise in inflammatory skin conditions.
Understanding and communicating these distinctions are crucial in both medical practice and patient education. Mislabeling can lead to inappropriate treatments or unnecessary concern. Clear clinical terminology ensures accurate diagnosis, avoids conflation with neoplastic processes, and guides proper management.
Final Summary: Is There a Cancer Link?
A Professional Conclusion on the Pili Multigemini–Cancer Debate
After a thorough review of clinical evidence, histological data, and scientific literature, there is no credible basis to suggest that pili multigemini is associated with skin cancer or any form of malignancy. Its unique follicular architecture may appear suspicious but has never demonstrated behavior consistent with neoplasia, invasion, or dysplasia.
This condition should be viewed in the same category as other benign structural anomalies—non-threatening, non-progressive, and manageable if needed for cosmetic reasons. In fact, over-medicalizing such anomalies can divert attention from more serious dermatological assessments and foster patient anxiety.
Education, gentle monitoring, and cosmetic care are the pillars of proper management. There is no indication for biopsy, excision, or surveillance unless other suspicious symptoms coexist. For both patients and clinicians, distinguishing harmless skin patterns from high-risk lesions is part of promoting dermatologic clarity and peace of mind. “Does botox cause cancer” is an example of concerns that are not based on facts, but on misinterpretations of information.
FAQ: Pili Multigemini and Cancer – 15 Essential Answers
Can pili multigemini become cancerous?
No, there is no scientific evidence that pili multigemini can turn into skin cancer. It remains a benign follicular anomaly without signs of dysplasia or cellular proliferation.
What does pili multigemini look like?
It typically appears as a cluster of thin hair shafts emerging from a single skin pore, most often on the face, neck, or back.
Is this condition common?
No, it is considered rare, although it may be underdiagnosed due to its subtle appearance and lack of symptoms.
Is a biopsy necessary?
In most cases, no. A biopsy is only performed if the lesion changes in appearance or if there is diagnostic uncertainty with similar-looking skin conditions.
Can this happen on the scalp?
Yes, although less common, pili multigemini can occur on the scalp, particularly in areas where hair is dense or shaving is frequent.
Are there genetic causes?
The exact cause is unclear, but developmental anomalies in the hair follicle structure during embryogenesis are likely responsible.
Does it cause pain or discomfort?
Typically no, but some patients may experience minor irritation if the area is shaved repeatedly or if folliculitis develops.
How is it treated?
Treatment is not usually required. If desired for cosmetic reasons, laser hair removal or topical skin care may help reduce visibility.
Is it contagious?
Absolutely not. Pili multigemini is not an infection and cannot be spread from person to person.
Does age or gender influence its appearance?
It may be more noticeable in men due to facial hair growth but can occur in any gender and at any age.
Can it be confused with skin cancer?
Visually, yes. In rare cases, it may resemble pigmented or irregular lesions, which is why clinical evaluation is helpful.
Is it linked to other skin conditions?
Sometimes it coexists with benign conditions like keratosis pilaris or seborrheic dermatitis, but not with cancer.
Does it go away on its own?
No, it tends to remain stable over time but doesn’t worsen or spread.
Can cosmetic treatments worsen it?
Overly aggressive skin treatments like exfoliation or waxing may irritate the follicles and should be done cautiously.
Why do people confuse this with cancer?
Mainly due to unfamiliar appearance and misinformation. Proper education and clinical reassurance resolve this concern.












