Persistent Fever in Stage 3 Melanoma
Persistent Fever in Stage 3 Melanoma: Causes, Concerns, and What to Do
- Why Does Fever Happen in Patients with Stage 3 Melanoma?
- Understanding the Mechanisms Behind Fever in Cancer
- How Common Is Persistent Fever in Stage 3 Melanoma?
- Clinical Trends and How Fever Relates to Cancer Stage
- What Causes Fever During Cancer or Its Treatment?
- When to Be Concerned: Alarming Signs That Need Immediate Attention
- How Doctors Diagnose the Source of a Fever in Melanoma
- Therapies That Help Manage and Control Persistent Fever
- Can Persistent Fever Be Prevented in Stage 3 Melanoma?
- How Long Will the Fever Last—Temporary or Ongoing?
- What Oncology Experts Say About Fever in Melanoma
- 15+ Frequently Asked Questions (FAQ)
Why Does Fever Happen in Patients with Stage 3 Melanoma?
Fever is a common but often misunderstood symptom in cancer care. In the case of stage 3 melanoma, a persistent fever may indicate multiple underlying issues—some benign, others serious. Fever can arise from the immune system’s response to tumor activity, side effects of cancer therapies, or as a result of infection due to a weakened immune system.
In advanced skin cancers, the body may develop systemic inflammatory reactions in response to tumor proteins, triggering a sustained rise in body temperature. This reaction is not necessarily harmful in itself, but when fever continues without clear cause, it becomes a warning sign.
Patients with melanoma often experience fatigue, chills, and night sweats alongside their fever, which can be mistaken for viral infections. However, when these symptoms persist, worsen, or don’t respond to antibiotics, it’s essential to consider the possibility of tumor-related fever or treatment-induced immune activation.
Understanding the Mechanisms Behind Fever in Cancer
The biological mechanism of fever in melanoma is often tied to the body’s immune and inflammatory responses. Cytokines—chemical messengers like interleukin-1, interleukin-6, and tumor necrosis factor (TNF)—are released in large amounts either by tumor cells or by immune cells reacting to them. These cytokines act on the hypothalamus in the brain, which controls body temperature, resulting in elevated fevers.
Fever may also occur as part of the body’s response to immunotherapy, which is frequently used in stage 3 melanoma cases. Drugs like checkpoint inhibitors (e.g., nivolumab or pembrolizumab) stimulate the immune system to attack cancer cells, but can also lead to inflammatory syndromes, including high fevers.
In some cases, tumor necrosis—the death of cancerous tissue due to treatment—can cause a “tumor fever.” The release of cellular debris into the bloodstream during this process may provoke high or fluctuating temperatures. Unlike infectious fevers, these are typically not responsive to antibiotics and may be resistant to antipyretics.
It’s important to distinguish fever as a symptom of disease progression, therapy reaction, or secondary infection—each with a different clinical implication and treatment pathway.
How Common Is Persistent Fever in Stage 3 Melanoma?
While fever is not the most frequent symptom associated with melanoma, it becomes more relevant in advanced stages—particularly during or after treatment. In stage 3 patients, fever is reported in approximately 15–25% of cases, depending on the therapy regimen used and overall disease activity.
Patients receiving immunotherapy or targeted therapy are more likely to report persistent fevers than those undergoing surgical treatment alone. According to observational studies, around 1 in 5 patients on checkpoint inhibitors may develop fever as a side effect of immune activation.
Clinical data also show that patients with bulky nodal disease or active inflammation near the primary tumor site may exhibit sustained febrile responses, particularly if there is lymph node involvement or regional recurrence—both common in stage 3 melanoma.
These trends emphasize the importance of monitoring temperature closely in this patient group, as persistent fever may sometimes signal treatment response—but it can also reflect serious complications such as sepsis, autoimmune toxicity, or rapid tumor progression.
Clinical Trends and How Fever Relates to Cancer Stage
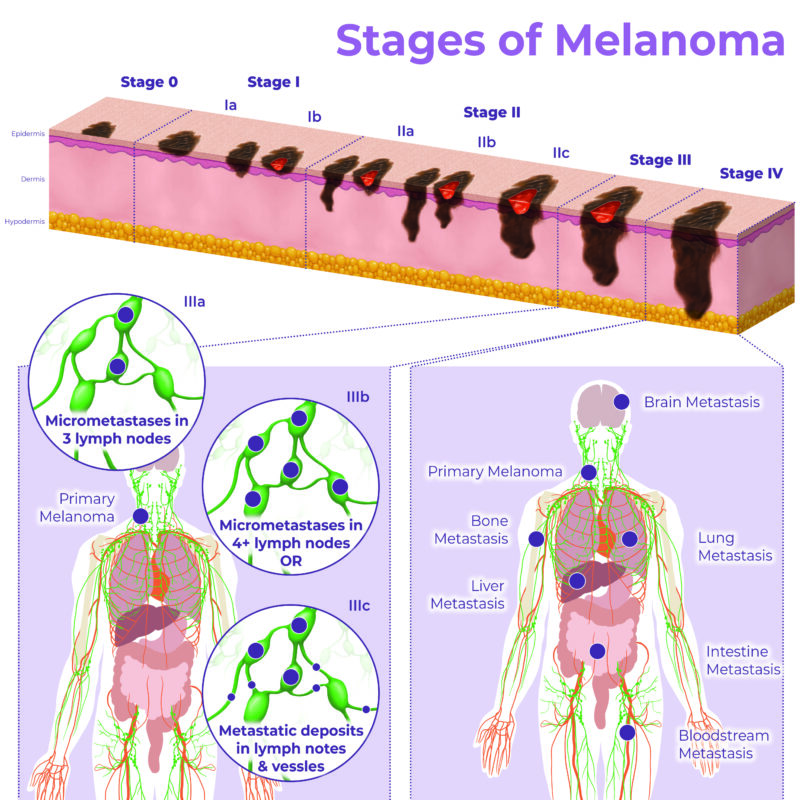
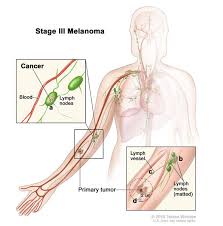
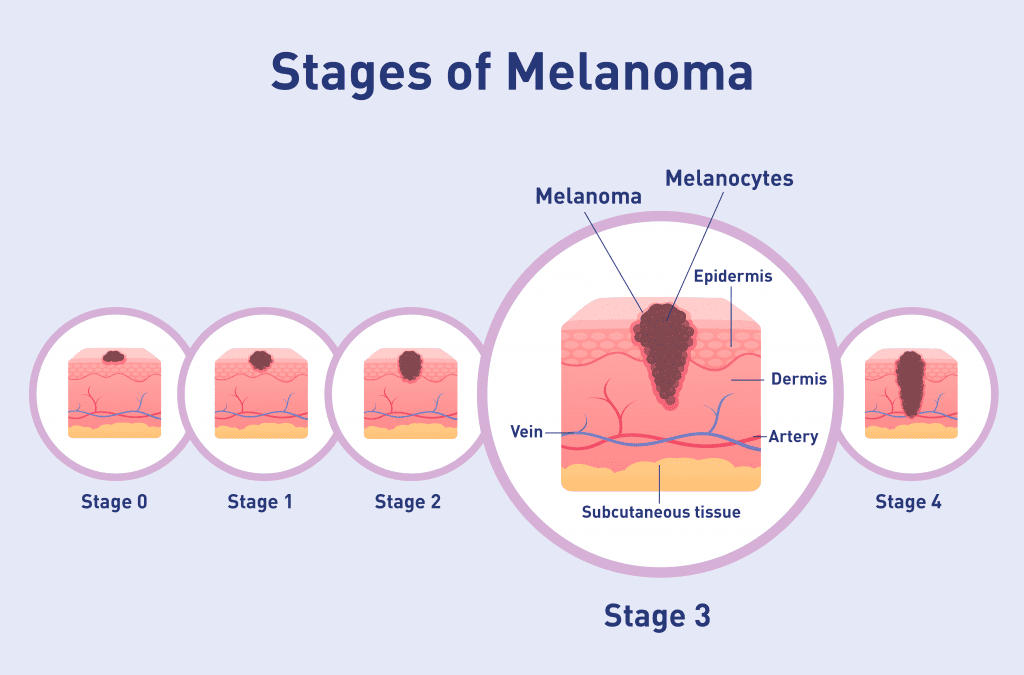
Persistent fever becomes more clinically significant as melanoma progresses through different stages. In early stages (0–1), fever is rare and usually unrelated to the cancer itself. However, in stage 3—where regional lymph nodes are involved—the incidence of systemic symptoms, including fever, increases.
Stage 3 melanoma is defined by the spread of cancer to nearby lymph nodes or skin areas but not distant organs. In this stage, the immune system is often highly active, either fighting the cancer or reacting to treatment. This leads to a higher chance of experiencing paraneoplastic fevers or immune-related adverse events.
Moreover, patients undergoing combination therapy—such as surgery followed by adjuvant immunotherapy—have a greater risk of systemic inflammatory responses. These reactions can sometimes be mistaken for infection or misattributed to unrelated causes.
It’s important to remember that not all fevers in cancer patients are dangerous. In fact, some studies suggest that low-grade fever after immunotherapy may correlate with better long-term outcomes. However, persistent high fevers or those accompanied by other red flags should always be evaluated, especially in advanced stages cancer.
What Causes Fever During Cancer or Its Treatment?
Fever in patients with melanoma—especially in stage 3—can originate from various sources. Understanding the cause is crucial for determining the right course of action.
1. Tumor-Related (Paraneoplastic) Fever
As melanoma cells proliferate or die (due to necrosis), they release inflammatory signals that affect the hypothalamus. This type of fever typically occurs without any signs of infection and may be accompanied by fatigue, weight loss, and night sweats. These are classic symptoms cancer patients report during progression.
2. Therapy-Induced Fever
Checkpoint inhibitors like nivolumab or ipilimumab activate the immune system to fight cancer but can cause systemic inflammation. Fever as part of immune-related adverse events (irAEs) can occur days or even weeks after infusion. Targeted therapies like BRAF/MEK inhibitors (e.g., dabrafenib + trametinib) may also cause drug-related fever in up to 50% of patients.
3. Infectious Fever
Patients undergoing cancer treatment are immunocompromised, increasing the risk of bacterial, viral, or fungal infections. These fevers usually come with chills, sore throat, cough, or localized signs like urinary or respiratory symptoms. Unlike tumor-related fevers, infectious ones often respond to antibiotics.
4. Autoimmune/Inflammatory Syndromes
Melanoma therapies can unmask or trigger autoimmune conditions like colitis, hepatitis, or thyroiditis, which present with fever. These inflammatory flares require immunosuppressive treatments and careful monitoring.
Recognizing the origin of fever helps determine whether to adjust cancer treatment, start steroids, or initiate antimicrobial therapy.
When to Be Concerned: Alarming Signs That Need Immediate Attention
While fever alone isn’t always dangerous, certain features demand urgent medical evaluation—especially in the context of stage 3 melanoma.
Seek immediate care if the fever:
- Exceeds 38.5°C (101.3°F) and persists more than 48 hours
- Is accompanied by chills, rigors, or sweating unrelated to ambient temperature
- Occurs after recent immunotherapy or targeted therapy
- Appears alongside chest pain, shortness of breath, abdominal pain, or persistent headache
Neurological symptoms such as confusion, dizziness, or seizures may point to autoimmune encephalitis or severe systemic infection. Similarly, a rapid drop in blood pressure, increased heart rate, or disorientation could signal sepsis or cytokine release syndrome.
Patients receiving immunotherapy should especially be vigilant about low-grade fever that escalates over time, as this can precede serious complications like pneumonitis or myocarditis.
In cases where fever is paired with elevated liver enzymes, jaundice, or gastrointestinal symptoms, physicians may suspect immune-mediated hepatitis or colitis, both of which require immediate steroid therapy.
Persistent fever in stages cancer is not something to ignore—especially when paired with rapidly changing clinical status.
How Doctors Diagnose the Source of a Fever in Melanoma
The workup for fever in melanoma patients involves a comprehensive approach that considers oncology, infectious disease, and autoimmune possibilities.
Initial Assessment
Doctors begin with a detailed history and physical exam. They ask about timing (post-therapy, duration), associated symptoms (rash, diarrhea, cough), and recent medication changes.
Blood Tests
Standard labs include complete blood count (CBC), C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), and liver/renal panels. Tumor fever often presents with elevated inflammatory markers but normal white blood cell counts, while infection shows leukocytosis.
Blood cultures and urine tests help rule out bacterial infections. In immunotherapy patients, thyroid function and autoimmune antibody panels may be included.
Imaging
Chest X-rays or CT scans detect pulmonary infections, lymphadenopathy, or treatment-related inflammation. Whole-body PET-CT can identify occult metastases or inflammatory lesions. Abdominal ultrasound or MRI may be used if gastrointestinal or liver symptoms are present.
Specialized Tests
If CNS involvement is suspected, lumbar puncture is performed. In some cases, tissue biopsy may be required to differentiate between tumor necrosis, infection, or drug-induced inflammation.
Early and accurate diagnosis ensures that persistent fever is treated effectively without delaying cancer therapy unnecessarily.
Therapies That Help Manage and Control Persistent Fever

Once the source of the fever is identified, treatment can be targeted to its underlying cause. This often requires a multidisciplinary strategy.
1. Paraneoplastic Fever
If related to tumor activity, NSAIDs (like naproxen) are often more effective than acetaminophen. Corticosteroids may also be prescribed in cases of severe inflammation, but they must be balanced carefully to avoid suppressing the anti-tumor immune response.
2. Treatment-Induced Fever
For immunotherapy-related fever, mild cases may be observed or treated with antipyretics. More severe cases require dose adjustments or temporary discontinuation. Corticosteroids are used for moderate-to-severe immune-related fever syndromes.
BRAF/MEK inhibitor-induced fever is managed by pausing the medication until symptoms resolve, followed by dose reduction or prophylactic antipyretics on rechallenge.
3. Infectious Fever
When infection is suspected or confirmed, empirical antibiotics are started immediately, often before cultures return. Broad-spectrum coverage is important in immunocompromised patients. Antifungals or antivirals may be added depending on symptoms and risk factors.
4. Supportive Measures
Hydration, rest, and cooling methods (e.g., tepid baths, compresses) can help improve comfort. Close monitoring of vitals and bloodwork is essential, especially during immunotherapy cycles.
When persistent fever leads to hospitalization, oncology teams collaborate with infectious disease and critical care specialists to manage complex cases while ensuring cancer treatment continues as safely as possible.
Can Persistent Fever Be Prevented in Stage 3 Melanoma?
Preventing persistent fever in stage 3 melanoma is not always possible, especially when the fever is linked to necessary cancer treatments or immune activity. However, several preventive strategies can reduce the risk of serious or prolonged fever episodes.
Proactive Monitoring
Regular temperature tracking—especially during immunotherapy cycles—can help detect low-grade fevers before they escalate. Patients should be encouraged to report any temperature spikes, even if they seem mild or unrelated.
Infection Prevention
Since infection is a leading cause of fever in cancer patients, maintaining hygiene, handwashing, and avoiding crowded or high-risk environments can significantly lower risk. Some high-risk patients may benefit from prophylactic antibiotics or antivirals during neutropenic periods.
Pre-Treatment Counseling
Before initiating checkpoint inhibitors or targeted therapies, oncologists often review potential immune-related side effects—including fever—with patients and caregivers. Some clinicians may prescribe prophylactic antipyretics or corticosteroids if previous fevers occurred during treatment.
Nutritional and Lifestyle Support
Proper hydration, rest, a balanced diet rich in anti-inflammatory foods, and stress reduction may also reduce the body’s inflammatory burden and lower the chances of systemic fever episodes.
Ultimately, while fever is often a reflection of the body’s active response to cancer or treatment, early action and preventive planning can limit its duration and severity.
How Long Will the Fever Last—Temporary or Ongoing?
The duration of fever in melanoma, particularly at stage 3, depends on the cause. Tumor-related fevers may persist until cancer is controlled or necrotic tissue is cleared. In contrast, fevers related to immune therapy or infections are usually temporary and resolve with appropriate treatment.
Checkpoint inhibitor–associated fevers may last several days to a week, though recurrent fevers may occur with repeated doses. For BRAF/MEK inhibitors, fever often resolves within 2–3 days after pausing the drug and may not return with adjusted dosing.
If the fever stems from an infection, it typically resolves within 48–72 hours of appropriate antibiotics—though resistant organisms or delayed diagnosis can prolong this window.
Autoimmune fevers or those related to cytokine release may require corticosteroids and tapering over weeks, especially if organ systems are involved. Rarely, persistent low-grade fevers can last months in cases of chronic inflammation or metastatic disease.
In general, once the underlying trigger is managed—whether infection, treatment, or inflammation—fevers tend to improve. However, ongoing or recurrent fever in the context of advanced stages cancer warrants thorough investigation.
What Oncology Experts Say About Fever in Melanoma
Experienced oncologists stress the importance of evaluating fever in melanoma patients within the broader context of treatment phase, disease burden, and overall symptoms.
Dr. Natalie Huang, a melanoma immunotherapy specialist, explains: “Fever after immune checkpoint blockade isn’t rare. What matters is whether it’s accompanied by lab abnormalities, organ symptoms, or rapid deterioration. Low-grade fever alone might be a good sign—it shows immune activity.”
Dr. Kevin Ramesh, a surgical oncologist, emphasizes vigilance: “After lymph node dissection in stage 3 melanoma, fever may mean infection or lymphatic complications. We often see delayed wound healing, cellulitis, or even abscesses. Post-op fever should never be brushed off.”
Experts recommend early and routine lab workups with any unexplained fever. They also encourage patients not to self-medicate repeatedly with antipyretics before identifying the source, as this can mask important signs.
Most importantly, oncologists agree that fever, while concerning, is also manageable with proper coordination between oncology, infectious disease, and internal medicine teams. The goal is always to treat the cause without interrupting effective cancer therapy unnecessarily.
15+ Frequently Asked Questions (FAQ)
1. Is fever normal in stage 3 melanoma?
Fever is not “normal,” but it can occur due to tumor inflammation, treatment side effects, or infection. Persistent or unexplained fevers should always be evaluated.
2. Can immunotherapy cause high fever?
Yes. Immune checkpoint inhibitors can cause systemic inflammatory reactions, including fever, sometimes within days or even weeks after administration.
3. Should I take paracetamol for every fever?
Mild fever may be monitored without medication. However, consult your oncologist before using antipyretics regularly, as they can mask more serious issues.
4. How do I know if my fever is from infection or cancer?
Infectious fever often comes with chills, rapid heart rate, or localized symptoms. Tumor or therapy-related fevers tend to persist and may not respond to antibiotics.
5. What tests will I need if I have persistent fever?
Common tests include blood cultures, CBC, CRP, liver/kidney panels, and imaging such as chest X-ray or PET-CT to identify infection or tumor activity.
6. Can I continue treatment if I have a fever?
It depends on the cause. For mild treatment-related fever, therapy may continue. But for infections or severe inflammation, treatment may be paused or adjusted.
7. Is fever a sign of melanoma spreading?
It can be. If fever is new or persistent in a patient with known disease, metastasis or tumor necrosis should be considered.
8. Can targeted therapy drugs cause fever?
Yes. BRAF and MEK inhibitors like dabrafenib/trametinib are known to cause fevers, sometimes severe enough to interrupt treatment.
9. What helps bring down cancer-related fever?
NSAIDs, corticosteroids, and sometimes just pausing treatment can help. The right choice depends on the fever’s cause.
10. Is fever dangerous in immunocompromised patients?
Yes. Fever in patients with low white blood cell counts (neutropenia) is a medical emergency and should be treated immediately.
11. How quickly should I report fever to my care team?
If your fever is over 38.5°C (101.3°F) or lasts more than 24 hours, contact your oncologist right away—especially during active treatment.
12. Does a persistent fever mean cancer is getting worse?
Not always. Some fevers come from immune activation or drug reactions, but it should always be checked to rule out progression.
13. Can steroids help reduce fever during cancer care?
Yes, especially for immune-related fevers. However, they may suppress your immune system, so they’re used carefully.
14. Are natural remedies safe for managing fever?
Cool compresses and hydration may help, but herbal supplements should be avoided unless approved by your medical team.
15. Will fever stop after treatment ends?
In most cases, yes. If the fever is therapy-related, it usually resolves post-treatment. If tumor-driven, it improves with disease control.












