Persistent Dry Throat: Possible Conditions and Clinical Evaluation
Clinical Meaning of Dry Throat
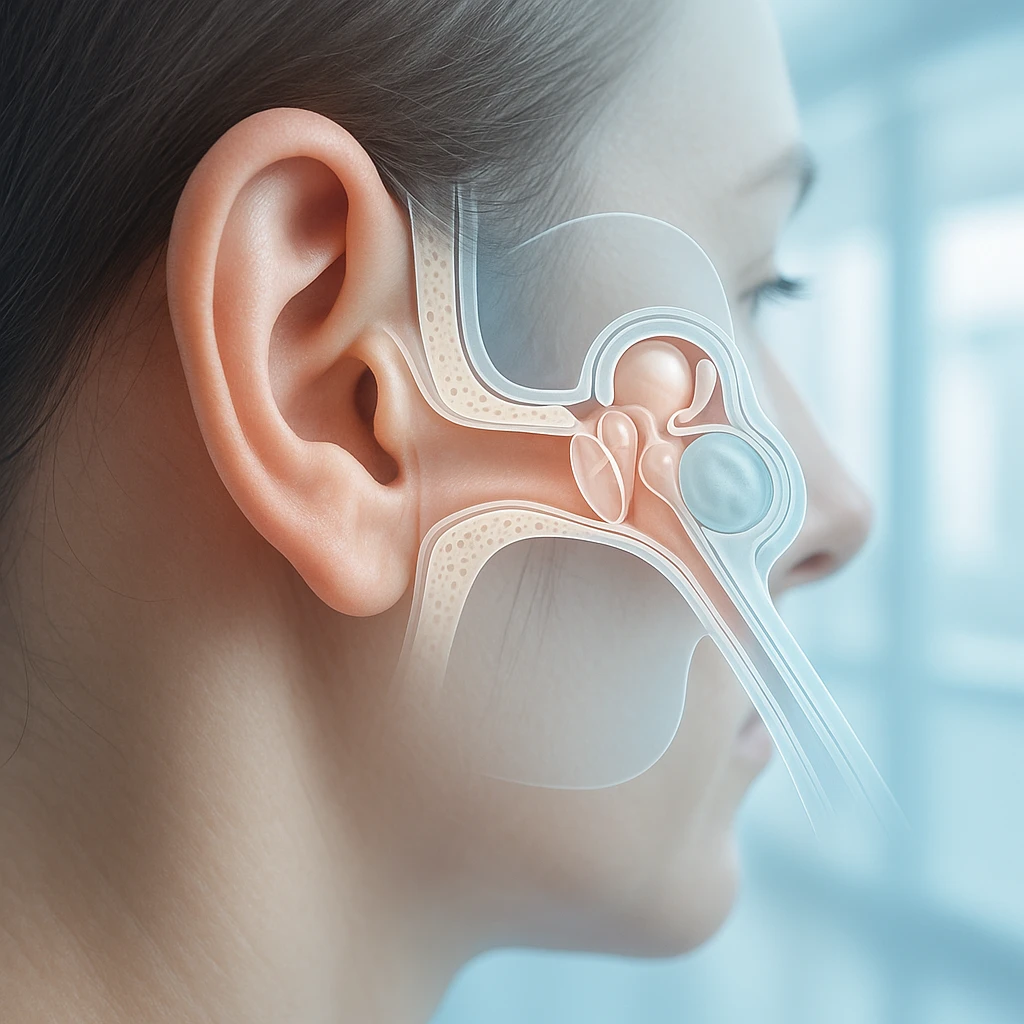
A dry throat is a common symptom that patients describe as a feeling of insufficient moisture, roughness, or irritation within the pharyngeal or oral tissues. This sensation often reflects the state of mucosal hydration and the effectiveness of salivary lubrication. While it may appear minor at first glance, dry throat can be an important clinical signal. It may emerge temporarily in everyday contexts, such as after speaking for extended periods in a dry environment, or it may indicate an underlying medical process that requires attention.
Environmental factors play a significant role. Dehydration and low ambient humidity can lead to a noticeable reduction in moisture within the throat, producing a sensation of dryness even when there is no inflammation or infection. In some cases, viral pharyngitis and other infections can also present with throat discomfort that includes a dry sensation, especially early in the illness before more pronounced inflammatory symptoms develop. When dryness is persistent, mucosal discomfort or irritation may occur, potentially affecting swallowing comfort and the quality of a patient’s daily activities.
Dryness vs. Pain: Clinical Differentiation
| Dryness | Pain |
|---|---|
| Dryness reflects changes in mucosal hydration or salivary function. Patients may describe a scratchy or rough feeling, or note that they feel the need to sip water frequently. | Pain is more commonly associated with inflammatory or infectious processes affecting the throat tissues. |
Understanding this distinction also supports better patient communication. For medical students and clinicians, asking patients to describe their symptoms in their own words can provide valuable insight into whether the issue is primarily moisture-related or inflammatory in nature.
Why Dryness Matters Clinically
- Repeated or persistent dryness may indicate reduced hydration, prolonged exposure to dry indoor air, or insufficient saliva production.
- Dryness may signal medication effects or systemic processes affecting salivary gland function.
- A broader assessment is often considered when dryness does not resolve with routine hydration or environmental adjustments.
Myths and Facts
| Myth | Fact |
|---|---|
| A dry throat always indicates infection. | Dryness can occur in the absence of infection and can result from environmental conditions or reduced saliva production. |
| Dry throat is harmless and can be ignored. | Persistent dryness can contribute to irritation and discomfort and may point to underlying systemic causes that benefit from early assessment. |
Causes and Contributing Factors
Dry throat can arise from a variety of physiological and environmental influences. Understanding how these contributing factors operate helps clinicians and learners distinguish between temporary discomfort and symptoms that may reflect underlying disease processes. While some causes are short-lived and related to day-to-day conditions, others involve more persistent alterations in salivary gland function or mucosal health. The mechanisms described below focus on how changes in hydration, glandular activity, and tissue sensitivity can lead to the sensation of dryness in the throat.
Salivary Flow and Gland Dysfunction
Saliva plays a key role in maintaining moisture and comfort within the throat. When salivary flow is reduced, the mucosal surfaces may become dry, leading to sensations of roughness or irritation. Anticholinergic and other xerogenic medications can decrease saliva production, which in turn can manifest as dryness affecting both the mouth and throat. Patients taking multiple medications simultaneously may be especially vulnerable, as combined pharmacologic effects can amplify reductions in salivary output.
In addition to medication effects, autoimmune disease can also influence salivary gland function. Autoimmune conditions such as Sjögren’s syndrome are recognized causes of persistent dryness affecting oral and pharyngeal mucosa. In these cases, glandular inflammation may interfere with the normal secretion of saliva, leading to chronic dryness that does not resolve with typical environmental adjustments. Identifying this mechanism requires careful clinical assessment, as the symptom profile may be subtle in early stages.
- Reduced salivary flow can cause mucosal dryness.
- Medication effects may be cumulative when multiple agents are involved.
- Autoimmune inflammation can impair glandular secretion over time.
Environmental and Behavioral Contributors
Daily environmental conditions often contribute to transient episodes of dryness. Dehydration and low ambient humidity can reduce the moisture available to the tissues of the throat. This may occur during seasonal changes, exposure to heated indoor air, or after periods of increased physical activity without adequate fluid intake. Because these situations affect mucosal hydration directly, the resulting dryness may resolve once hydration is restored or environmental humidity increases.
Behavioral factors can also play a role. Mouth breathing, for example, can increase airflow across the mucosal surfaces, allowing moisture to evaporate more quickly. Occupational exposures involving dust, smoke, or chemical irritants can similarly affect throat comfort. When environmental or behavioral contributors are identified, addressing the source often helps reduce the frequency or intensity of dryness.
- Low humidity environments may temporarily reduce mucosal moisture.
- Mouth breathing increases evaporative loss from mucosal surfaces.
- Exposure to airborne irritants may influence throat comfort.
Infectious and Allergic Processes
In some cases, dryness occurs alongside other symptoms of infection or allergic response. Viral pharyngitis and other infections may present with throat discomfort that includes a sensation of dryness, particularly in the early stages before inflammation becomes more prominent. In this situation, dryness may be one part of a broader pattern of symptoms, such as low-grade fever or mild soreness.
Noninfectious triggers such as allergens and environmental irritants can also provoke throat dryness. These agents may affect the mucosal lining and contribute to temporary irritation without leading to persistent changes in salivary function. Recognizing this pattern may help differentiate temporary responses from ongoing salivary dysfunction or systemic disease.
- Dryness may present early in viral throat infections.
- Allergens can cause transient irritation without long-term dryness.
Recognizing Symptoms and Clinical Diagnosis
Understanding how patients describe dry throat symptoms and how these symptoms present during evaluation is essential for determining the underlying cause. A thoughtful clinical approach explores patient history, physical findings, and the broader medical context. By identifying characteristic patterns in sensation, salivary function, and associated features, clinicians can distinguish between dryness caused by environmental or behavioral factors and dryness linked to systemic or inflammatory processes.
Symptom Patterns and Examination Findings
Patients experiencing reduced salivary flow may report difficulty swallowing, particularly when attempting to swallow dry foods or speak for prolonged periods. This difficulty often stems from a lack of lubrication on the mucosal surfaces. Altered or diminished taste can accompany oral and throat dryness, as saliva contributes to the distribution and dissolution of taste molecules. These symptoms may present gradually and fluctuate depending on hydration levels and daily activities.
On examination, the mucosa of the throat or oral cavity may appear dry or lack the normal glistening layer of moisture. Saliva may appear thick or scant, and patients may demonstrate frequent swallowing or throat clearing in an attempt to relieve discomfort. Observations during clinical interaction can provide valuable clues to the nature and severity of dryness.
- Difficulty swallowing may indicate reduced salivary lubrication.
- Altered taste can accompany oral and throat dryness.
- Visible dryness of mucosal surfaces may support the clinical impression.
Medication and Medical History Review
A structured medication review is essential to identify xerogenic drugs that may reduce salivary flow. Anticholinergic medications are well-recognized contributors, and the likelihood of dryness may increase when multiple medications with similar effects are used together. Understanding the duration and dosage of these medications helps clarify whether they play a role in symptom onset.
Beyond medication assessment, evaluating the medical history for systemic conditions associated with salivary gland dysfunction is important. Autoimmune conditions and other chronic health concerns may affect glandular function, leading to persistent dryness. Identifying these associations early can support timely referral and further diagnostic workup when needed.
- Review current and recent medications for xerogenic effects.
- Consider polypharmacy as a compounding factor.
- Evaluate for systemic conditions associated with salivary gland involvement.
Distinguishing Infection vs. Noninfectious Etiologies
Clinical evaluation also involves distinguishing dryness associated with infection from dryness arising from noninfectious causes. Viral pharyngitis often presents with throat discomfort that may include dryness, particularly in early stages before more obvious signs such as redness or significant soreness develop. In these cases, dryness may be part of a broader constellation of symptoms.
Noninfectious dryness, by contrast, is more closely related to hydration status, salivary function, or environmental exposure. When evaluating a patient, clinicians consider the duration of symptoms, recent exposures, medication use, and the presence or absence of systemic signs. This helps determine whether further diagnostic testing or targeted management strategies are appropriate.
| Feature | Infectious Pattern | Noninfectious Pattern |
|---|---|---|
| Onset | Often acute | May be gradual or fluctuating |
| Associated symptoms | Possible fever or sore throat | May relate to hydration or medication use |
| Mucosal appearance | May show inflammation | Often appears dry without redness |
Management, Long-Term Impact, and Prevention
Managing dry throat involves addressing both immediate discomfort and any underlying contributors. The goal of treatment is to improve mucosal moisture, reduce evaporative loss, and protect oral tissues from long-term effects. At the same time, identifying systemic conditions or medication influences plays a key role in guiding care. By combining supportive strategies with targeted clinical approaches, patients can experience both symptom relief and improved overall throat health.
Supportive and Moisture-Based Interventions
Symptomatic measures often aim to increase moisture or reduce evaporative loss. Hydration is central to this process because adequate fluid intake supports normal saliva production. Humidifying indoor air may also help, particularly in environments where heated indoor air or naturally low humidity contributes to dryness. These environmental adjustments enhance mucosal hydration and may reduce fluctuations in comfort throughout the day.
In some situations, saliva substitutes or lubricating mouth rinses may offer additional moisture when natural salivary flow is insufficient. These products help coat the mucosal surfaces, reducing friction that can occur when speaking, swallowing, or breathing through the mouth. Behavioral adjustments, such as taking breaks during extended speech or modifying breathing patterns, can further decrease moisture loss and help maintain a sense of throat comfort.
- Maintain adequate hydration throughout the day.
- Use humidification when indoor air is dry.
- Consider saliva substitutes when natural production is reduced.
- Adjust speech and breathing habits to minimize moisture loss.
Targeted Therapies Based on Etiology
When dryness is linked to underlying health conditions, treatment should focus on addressing those root causes. Treatment of underlying systemic disease is integral when identified, as improving the primary condition can help restore more typical salivary function. For example, when salivary gland dysfunction is associated with autoimmune processes, coordinated care with specialists may be valuable for long-term symptom improvement.
Pharmacologic sialogogues are options in selected patients with salivary hypofunction. These medications act on salivary glands to stimulate saliva production, potentially reducing symptoms of dryness when natural saliva flow is insufficient. Their use is generally tailored to the individual and guided by the severity of symptoms, patient tolerance, and underlying health context. These therapies support patients for whom supportive measures alone are not enough to maintain comfort.
| Approach | Purpose | Typical Use Case |
|---|---|---|
| Systemic disease management | Addresses root cause of gland dysfunction | Autoimmune or chronic systemic conditions |
| Pharmacologic sialogogues | Stimulates salivary gland output | Documented salivary hypofunction |
| Supportive moisture strategies | Reduces discomfort and dryness | Day-to-day symptom relief |
Preventive Measures and Monitoring
Prevention involves maintaining awareness of environmental and behavioral factors that influence mucosal moisture. Environmental dryness, such as that caused by heated indoor air, can precipitate symptoms. Adjusting humidity levels, staying well-hydrated, and recognizing early signs of dryness can help reduce the duration or intensity of episodes. These practices are particularly useful for individuals who experience recurrent, mild symptoms.
Monitoring for persistent or progressive dryness is important, because chronic oral dryness increases risk for dental caries. When saliva is reduced for extended periods, the natural protective mechanisms that support enamel integrity weaken. Mucosal injury and discomfort can also result from persistent dryness, particularly when friction occurs on already sensitive tissues. For this reason, early recognition and ongoing evaluation can help identify when further medical assessment is needed. Encouraging patients to report changes in symptom frequency or severity can support timely intervention and reduce long-term impact on oral health and comfort.
- Monitor dryness patterns and triggers over time.
- Adjust environment and hydration proactively.
- Seek evaluation if symptoms are persistent or worsening.
Frequently Asked Questions
Why does my throat feel dry even when I’m drinking enough water?
Hydration supports saliva production, but environmental conditions like heated indoor air or mouth breathing can still dry the mucosal surfaces. If dryness continues despite good hydration, other factors such as medication effects or salivary gland function may be involved.
Is a dry throat always related to an infection?
No. Dry throat can be caused by noninfectious factors such as low humidity, dehydration, or reduced saliva flow. Infections may cause dryness too, but they typically include additional symptoms like fever or noticeable soreness.
Why do some medications cause throat dryness?
Certain medications, including anticholinergic drugs, can reduce salivary gland output. When saliva is limited, the throat may feel rough or irritated because natural lubrication is decreased.
Can a dry throat be a sign of an underlying medical condition?
Yes. Persistent dryness may be associated with conditions that affect salivary glands, such as autoimmune diseases. In these cases, the dryness may continue even with hydration and environmental adjustments.
What symptoms might accompany chronic throat dryness?
Some people experience difficulty swallowing, especially with dry foods, or notice altered taste. Over time, prolonged dryness can also increase the risk of dental caries and oral discomfort.
How do clinicians tell the difference between dry throat from infection and dryness from other causes?
Clinicians look at symptom patterns, timing, mucosal appearance, and associated signs. Infectious dryness often appears with inflammation or fever, while noninfectious dryness may be more gradual and linked to hydration status or medication use.
When should someone seek medical evaluation for a dry throat?
If dryness is persistent, worsens over time, or is accompanied by difficulty swallowing, changes in taste, or dental concerns, evaluation is appropriate. A clinician can determine whether the dryness is environmental, medication-related, or linked to a systemic condition.