Pelvic Pain in Cervical Cancer
Pelvic Pain in Cervical Cancer: Understanding the Causes, Risks, and Management
- Why Does Pelvic Pain Occur in Cervical Cancer?
- Tumor Pressure and Inflammatory Mechanisms
- How Common Is This Symptom in Cervical Cancer?
- Underlying Causes: Cancer and Treatment-Related Triggers
- When to Consider the Pain a Red Flag
- How Doctors Diagnose the Cause
- Managing and Relieving the Discomfort
- Prevention Strategies: Is It Possible?
- Will the Pain Eventually Go Away?
- Clinical Advice from Oncology Experts
- Recognizing Pelvic Pain in Cervical Cancer: What It Feels Like and Why It Happens
- The Biological Link Between Cervical Tumors and Pelvic Pain
- What Drives Pelvic Pain in Cancer Patients?
- How Doctors Determine the Source of the Pain
- 15+ Questions to Ask Your Doctor
Why Does Pelvic Pain Occur in Cervical Cancer?
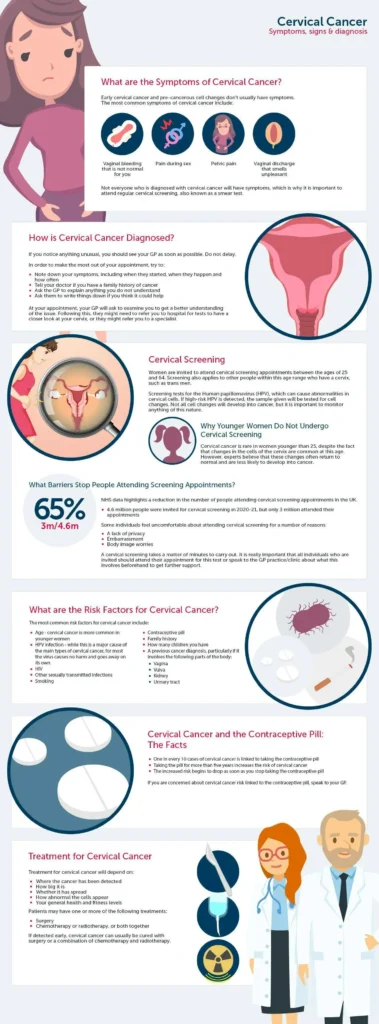
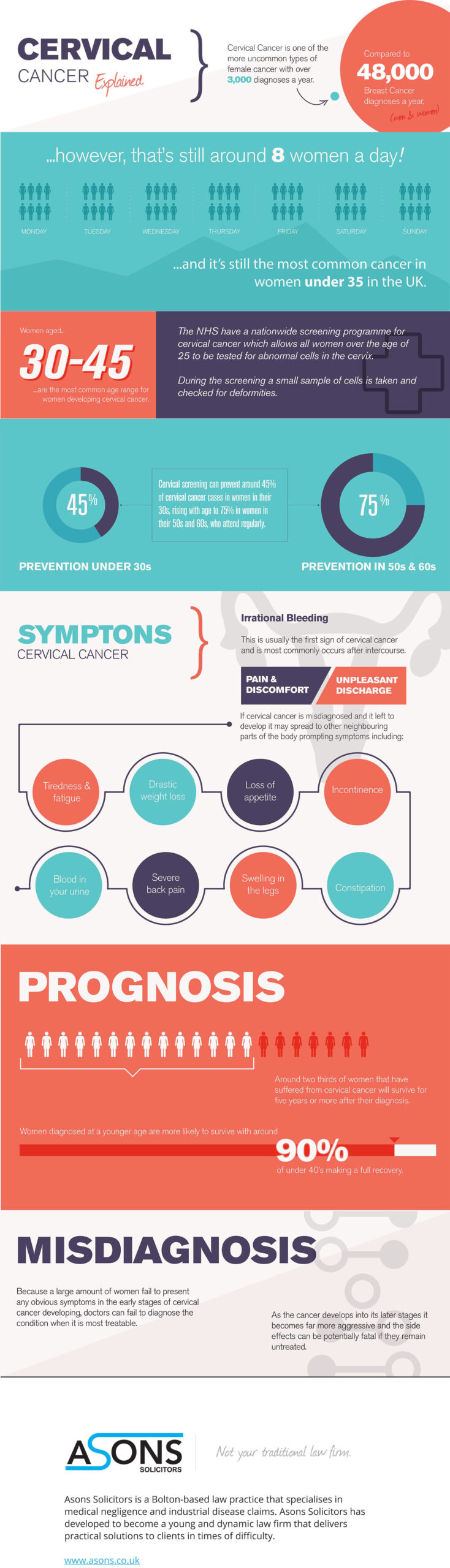
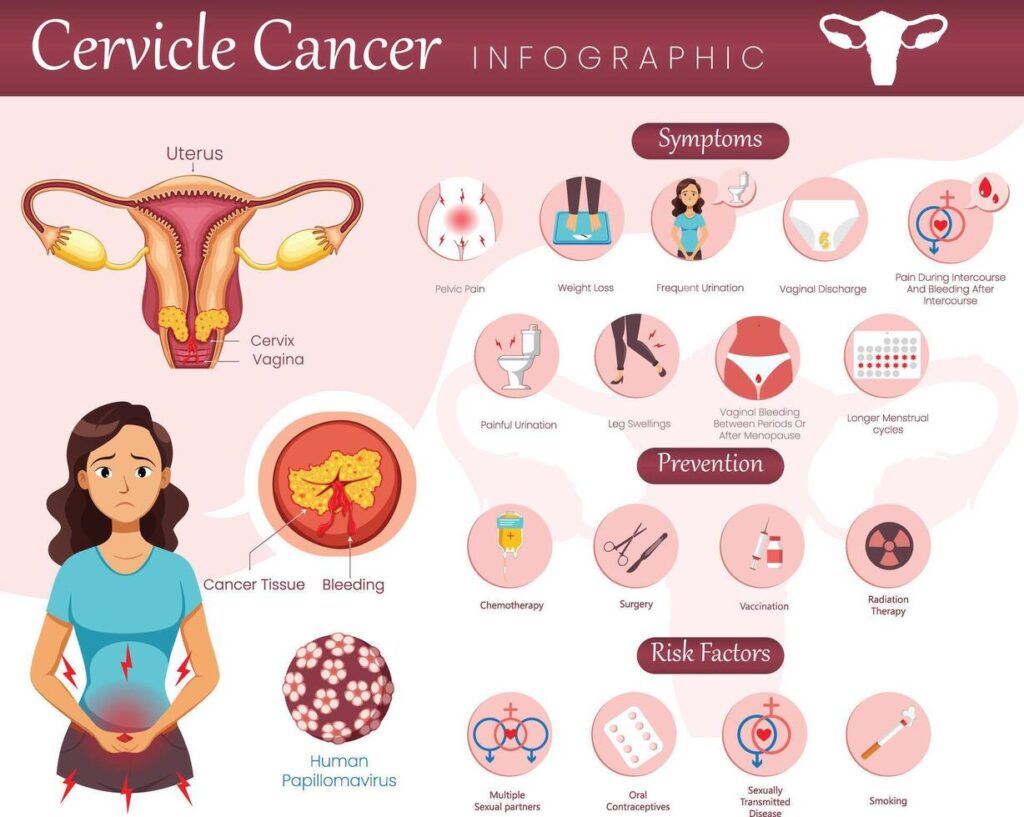
Pelvic pain in cervical cancer is not just a localized discomfort; it often reflects deeper biological and structural disruptions caused by tumor presence or treatment effects. Patients commonly describe this pain as a dull ache, cramping, or pressure sensation in the lower abdomen, which may radiate to the back or legs. It can worsen with activity, menstruation, or bowel/bladder movements. As with breast cancer headaches, which may suggest progression or metastasis, cervical pain can be an early warning sign of local tumor spread.
Tumor Pressure and Inflammatory Mechanisms
Pain originates either from direct tumor invasion into surrounding pelvic tissues or due to inflammation provoked by the body’s immune response. Cervical tumors can press against nerves, ligaments, or the pelvic wall, triggering nociceptors (pain receptors). Treatments like radiotherapy may also cause tissue fibrosis or nerve irritation, exacerbating discomfort. Additionally, hormonal shifts and vascular changes induced by cancer therapy can sensitize the pelvic region.
How Common Is This Symptom in Cervical Cancer?
Pelvic pain is a hallmark symptom of advanced-stage cervical cancer but may appear earlier depending on tumor size and location. In stages IB2 and above, over 50% of patients report intermittent or constant pelvic discomfort. Clinical data suggest pain intensity often correlates with disease progression and local invasion.
| Stage | % Reporting Pelvic Pain | Notes |
| IA1 | Rare | Usually asymptomatic |
| IB2 | ~40% | Pain with movement or menstruation |
| IIB+ | 50–70% | Often continuous, requiring medication |
Underlying Causes: Cancer and Treatment-Related Triggers
Pelvic pain can be linked to:
- Tumor progression pressing on pelvic nerves or organs
- Radiation effects (fibrosis, nerve entrapment)
- Chemotherapy-induced inflammation
- Post-surgical adhesions or nerve injury
- Metastases to surrounding lymph nodes or bones
- Urinary or gastrointestinal obstruction
Some pain may even be referred from neighboring organs, as occurs in certain differential diagnoses between Cervical Cancer vs. Ovarian Cancer.
When to Consider the Pain a Red Flag
There are moments when pelvic pain is more than a nuisance. If it escalates suddenly, interferes with walking, sleep, or daily functions, or is accompanied by abnormal bleeding, weight loss, or incontinence, this warrants immediate evaluation. Worsening pain during treatment could also suggest tumor resistance or complications like infection or metastasis.
How Doctors Diagnose the Cause
Proper diagnosis involves a multi-modal approach:
- Pelvic examination to assess tenderness, mass effect, or rigidity
- Pelvic ultrasound or MRI to visualize tumor extent and tissue changes
- PET-CT scans for metastatic spread
- Biopsies if new lesions are identified
- Pain mapping with anesthetic blocks to locate origin
Blood work may also rule out infection, anemia, or hormonal shifts contributing to discomfort.
Managing and Relieving the Discomfort
Pain relief should be personalized. Non-steroidal anti-inflammatory drugs (NSAIDs) may be sufficient for mild pain. Opioids are reserved for severe cases. Nerve blocks, pelvic floor physical therapy, or acupuncture can offer non-pharmacologic relief. Radiologic interventions like tumor debulking may also alleviate mechanical pressure.
In cases of muscle tension, therapies that target the pelvic floor may be prescribed in parallel to cancer treatment.
Prevention Strategies: Is It Possible?
While not all pelvic pain is preventable, minimizing its severity is achievable with proactive care. Early-stage treatment, pre-radiation planning to avoid nerve damage, and physical rehabilitation to maintain muscle balance are key. Maintaining good hydration, gentle movement, and stress management also help reduce inflammatory pain.
Will the Pain Eventually Go Away?
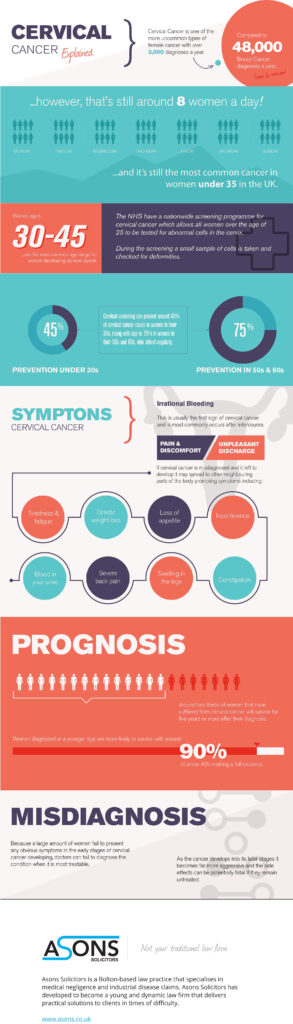
Pain duration varies. For early-stage patients post-surgery, discomfort may subside in weeks. Radiation-induced pain might linger for months. In metastase or late-stage disease, chronic pain management becomes part of long-term care. Pain-free status often aligns with cancer remission.
| Scenario | Prognosis of Pain |
| Early-stage post-op | Temporary |
| Radiation fibrosis | Months to years |
| Active metastatic spread | Often persistent |
Clinical Advice from Oncology Experts
Doctors emphasize early reporting of pelvic pain as it can signal recurrence or treatment complications. Multidisciplinary teams—including pain specialists, radiologists, gynecologic oncologists, and physical therapists—are crucial. Personalized approaches that combine medication, physical therapy, and psychosocial support yield the best outcomes.
Recognizing Pelvic Pain in Cervical Cancer: What It Feels Like and Why It Happens
Pelvic pain is one of the hallmark symptoms of cervical cancer, particularly in its more advanced stages. For many women, the pain is dull and persistent, often radiating into the lower back or down the thighs. Some describe it as a heavy, cramping ache, not unlike menstrual discomfort, but more continuous and less responsive to typical pain relievers. This discomfort can stem directly from the tumor’s pressure on surrounding pelvic structures, nerve involvement, or inflammation in adjacent tissues.
Pelvic pain in cervical cancer can also intensify during physical activity, urination, or sexual intercourse. This pain often correlates with the cancer’s growth and its invasion of nearby organs such as the bladder, uterus, or rectum. Recognizing the nature of this pain early is crucial, especially when it appears alongside other signs like abnormal vaginal bleeding or discharge.
The Biological Link Between Cervical Tumors and Pelvic Pain
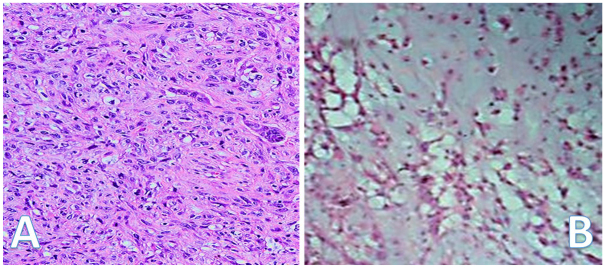
Cervical cancer begins in the cells lining the cervix and often progresses locally before spreading to distant organs. As the tumor grows, it can exert pressure on pelvic nerves or invade surrounding tissues. Inflammatory responses triggered by cancer cells contribute to local swelling, nerve sensitization, and referred pain patterns that extend into the pelvis, abdomen, or thighs.
Moreover, treatment itself—especially radiation and some chemotherapeutic agents—can cause neuropathic pain or tissue irritation that mimics or amplifies cancer-related discomfort. For instance, radiation-induced fibrosis can stiffen soft tissues, reducing flexibility and causing aching in the lower pelvis.
What Drives Pelvic Pain in Cancer Patients?
| Category | Contributing Factors |
| Tumor Involvement | Pressure on nerves, tissue invasion, mass effect |
| Treatment Side Effects | Radiation fibrosis, chemotherapy-induced neuropathy |
| Metabolic Disturbance | Inflammation, lactic acidosis, hormone shifts |
| Psychological Factors | Anxiety, depression, and stress response amplification |
Pain may be multifactorial, with overlapping causes. For example, a patient undergoing pelvic radiation may have both direct tumor pain and radiation-induced nerve irritation. Additionally, psychological distress related to a cancer diagnosis can exacerbate pain perception, a phenomenon well-documented in oncologic care.
How Doctors Determine the Source of the Pain
Diagnosis typically begins with a thorough history and pelvic examination. If cervical cancer is suspected or already diagnosed, imaging studies play a vital role:
| Diagnostic Method | Purpose |
| Pelvic Ultrasound | Assesses cervical mass, fluid collection, ovarian involvement |
| MRI or CT Scan | Maps tumor spread, checks for nodal or organ involvement |
| PET-CT | Detects distant metastases and functional tumor activity |
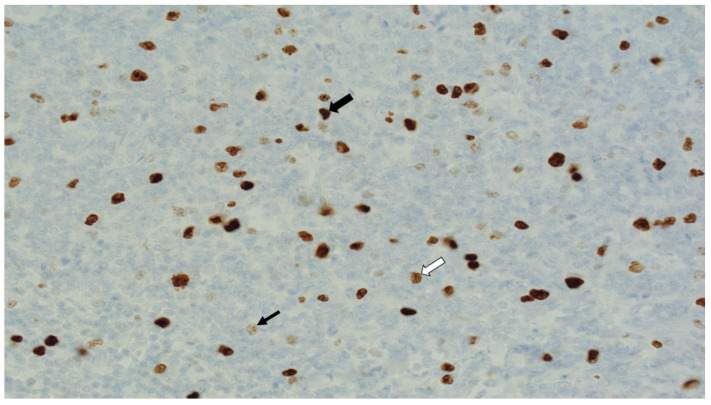
| Biopsy and Histology | Confirms malignancy and determines histological subtype |
Blood tests may also be used to check inflammatory markers, kidney function, and tumor markers relevant to differential diagnoses.
15+ Questions to Ask Your Doctor
1. What is causing my pelvic pain—is it the tumor or something else?
Understanding whether the discomfort stems from tumor pressure, inflammation, nerve compression, or treatment side effects is crucial for tailored care.
2. Can imaging confirm the exact source of the pain?
Knowing whether scans will help pinpoint the origin can guide further diagnostic or therapeutic steps.
3. Are there medications that can help without too many side effects?
Patients should be informed of pain relief options and their impact on daily function.
4. Could pelvic floor therapy be helpful in my case?
Ask if a referral to a specialist in pelvic rehabilitation is appropriate for your type of pain.
5. Will my pain get worse as treatment progresses?
Getting a realistic expectation helps patients prepare and adjust their lifestyle accordingly.
6. What are signs that my cancer is coming back if pelvic pain increases?
Clarify what symptoms indicate recurrence so they can be monitored proactively.
7. Should I see a pain management or palliative care specialist?
Timely referrals can greatly improve pain control and overall well-being.
8. Could hormonal changes be playing a role in this pain?
Hormonal shifts from treatment or menopause can influence pelvic discomfort.
9. Is there anything I should avoid doing to prevent the pain from worsening?
Lifestyle adjustments may be necessary to reduce pelvic strain or inflammation.
10. How does this symptom affect my cancer prognosis or treatment plan?
Pain status can impact treatment tolerance and decisions.
11. Will I always need medication, or can I wean off it over time?
Discuss tapering strategies and alternatives if symptoms stabilize.
12. How often should I have follow-up exams if I have ongoing pelvic pain?
Clear monitoring schedules reduce anxiety and catch problems early.
13. Can pelvic pain affect my bladder or bowel function?
Find out if symptoms are interconnected and need multidisciplinary care.
14. Is my pain typical for someone with cervical cancer at my stage?
This question gives context and reassurance or alerts to unusual issues.
15. What can I do at home to manage pain better day-to-day?
Practical tips like hot compresses, posture adjustments, or dietary choices matter.