Painful Urination in Prostate Cancer
Painful Urination in Prostate Cancer: Understanding Symptoms, Causes, and Treatment
- Why Does It Hurt to Urinate During Prostate Cancer?
- The Underlying Mechanism: Tumor Pressure, Inflammation, and Nerve Involvement
- How Common Is Painful Urination in Men with Prostate Cancer?
- Clinical Data and Symptom Progression
- Causes of Painful Urination: Cancer, Treatment, and More
- When to Take This Symptom Seriously
- Diagnostic Tools for Understanding Dysuria in Cancer
- Therapeutic Approaches and Comfort Measures
- Preventing Painful Urination During Treatment
- Will the Pain Go Away Over Time?
- What Oncologists Say About Managing Urinary Pain
- Questions to Ask Your Doctor
- 15+ FAQ: Painful Urination in Prostate Cancer
Why Does It Hurt to Urinate During Prostate Cancer?

Painful urination—also called dysuria—is a frequent complaint among men with prostate cancer, particularly in the more advanced stages or during specific treatments. While occasional discomfort while urinating can result from infections or irritation, persistent or severe pain may indicate tumor involvement in or around the urinary tract.
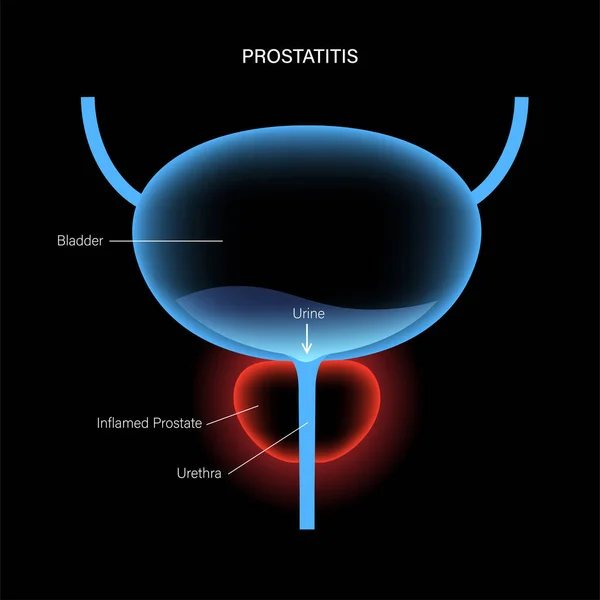
The prostate gland surrounds the urethra, the tube that carries urine from the bladder out of the body. As cancer grows, it may compress or infiltrate the urethra or bladder neck, leading to symptoms like burning, stinging, or sharp pain during urination.
Painful urination is also linked to inflammation, infection, or scarring resulting from biopsy, radiation therapy, or hormonal treatment. In some cases, it coincides with frequent urination without pain, evolving later into more severe discomfort.
The Underlying Mechanism: Tumor Pressure, Inflammation, and Nerve Involvement
There are several ways prostate cancer contributes to painful urination:
- Tumor growth compresses the urethra, making urination strained and painful.
- Cancer cells infiltrating the bladder neck or surrounding tissue trigger inflammation and localized pain.
- Radiation therapy and some hormone treatments cause irritation or fibrosis of the bladder lining.
- Nerve endings around the prostate may be activated by tumor invasion, especially in later stages.
These processes irritate the delicate mucosal surfaces and nerves involved in urination, making the act of passing urine painful—particularly at the beginning or end of the stream.
Table: Key Mechanisms Leading to Painful Urination in Prostate Cancer
| Cause | Description |
| Urethral compression | Tumor growth narrows urinary pathway |
| Bladder neck invasion | Cancer spreads to bladder entry point |
| Radiation cystitis | Inflammation of bladder due to radiation |
| Hormonal side effects | Tissue thinning, dryness, or irritation |
| Infection (secondary to cancer) | Incomplete voiding leads to bacterial growth |
| Nerve involvement | Cancer irritates pain-sensitive nerve fibers |
How Common Is Painful Urination in Men with Prostate Cancer?
Painful urination is one of the most commonly reported lower urinary tract symptoms in prostate cancer patients, although its prevalence depends on the cancer’s stage, treatment type, and other individual factors. While early-stage cancers may cause minimal symptoms, as the tumor enlarges or therapy intensifies, urinary pain often worsens.
It is especially common during or after:
- External beam radiation therapy
- Brachytherapy (internal radiation)
- Hormone deprivation therapy
- TURP or biopsy-related interventions
In clinical settings, up to 40–60% of men undergoing aggressive radiation or late-stage treatment for prostate cancer report pain or burning during urination.
Clinical Data and Symptom Progression
The severity and frequency of dysuria often reflect the cancer’s proximity to the urinary system and the cumulative effects of therapy. While not all patients experience pain, those with high-risk or locally advanced cancers are at greater risk.
Below is a comparative overview of pain occurrence across different treatment stages and cancer types:
| Context | Frequency of Painful Urination |
| Early-stage prostate cancer | Low to moderate (~15–20%) |
| Post-biopsy phase | Temporary, ~30% |
| Radiation therapy (EBRT or seeds) | Moderate to high (40–60%) |
| Hormonal treatment | Moderate (~25–40%) |
| Advanced/metastatic stage | High (~60–70%) |
Note: Pain may also coincide with other urinary symptoms such as frequent urination without pain, urgency, or nighttime urination.
Causes of Painful Urination: Cancer, Treatment, and More
Painful urination in men with prostate cancer is rarely caused by a single issue. Instead, it is the result of overlapping oncological, treatment-related, infectious, and metabolic factors. Understanding these underlying mechanisms helps clinicians tailor symptom management effectively.
Cancer itself contributes through tumor expansion, urethral compression, and bladder involvement. Radiation therapy often leads to inflammation and microvascular damage of the bladder and urethra. Hormonal treatments can thin the tissues and make them more sensitive, while catheterization or urinary retention increases the risk of secondary infection.
Table: Categories of Causes of Painful Urination in Prostate Cancer
| Cause Type | Specific Factors |
| Oncologic | Urethral invasion, tumor-induced inflammation |
| Therapeutic | Radiation cystitis, side effects of hormone therapy |
| Infectious | Urinary tract infections due to incomplete emptying |
| Metabolic | Dehydration, concentrated urine irritating the urethra |
| Neurological | Nerve pain related to cancer near pelvic plexus |
This multifactorial nature explains why pain can fluctuate during treatment cycles or worsen unexpectedly, especially in patients with advanced disease.
When to Take This Symptom Seriously
Not all urinary discomfort requires emergency care, but some scenarios should prompt immediate medical evaluation. For men undergoing treatment for prostate cancer, any new or worsening urinary pain can signal infection, bladder damage, or even progression of the tumor.
Pain that occurs with fever, chills, hematuria (blood in the urine), or difficulty starting or stopping urine flow can indicate serious complications. If pain intensifies with every voiding attempt or prevents urination altogether, urgent intervention is needed.
When Painful Urination Becomes a Warning Sign
| Symptom Combination | Possible Concern |
| Pain + fever + urgency | Urinary tract infection |
| Burning + blood in urine | Radiation injury or tumor erosion |
| Pain with interrupted flow or retention | Obstruction from cancer |
| Sudden onset during therapy | Drug side effect or acute inflammation |
| Pain worsening at night or after urination | Urination reflex arc irritation |
Persistent or worsening symptoms deserve attention, even if they initially seem mild. Patients are advised not to self-treat with antibiotics or analgesics without consultation.
Diagnostic Tools for Understanding Dysuria in Cancer
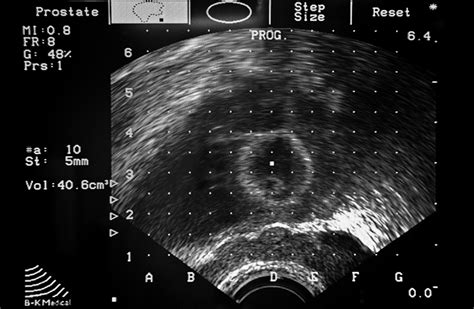
Diagnosis of painful urination in prostate cancer patients begins with a detailed symptom review and physical examination, including a digital rectal exam. Laboratory and imaging studies help determine the source of the symptom—be it cancer progression, infection, or therapy-related inflammation.
Urine analysis is essential to rule out bacterial or fungal infections. Post-void residual scans help assess bladder function, while cystoscopy can visualize the urethra and bladder wall directly. In some cases, prostate imaging (MRI or TRUS) is used to evaluate structural changes.
Table: Diagnostic Approach to Painful Urination in Prostate Cancer
| Diagnostic Test | Purpose |
| Urinalysis and culture | Rule out infection or hematuria |
| Cystoscopy | Direct visualization of bladder and urethra |
| PSA and other blood tests | Monitor tumor activity and inflammation |
| Post-void residual (PVR) | Evaluate urinary retention |
| Transrectal ultrasound (TRUS) | Assess prostate volume, potential blockage |
| MRI pelvis | Detect tumor spread or compression |
These tests collectively provide a clearer picture of whether the symptom is temporary or indicative of deeper complications, including recurrence or post-treatment scarring.
Therapeutic Approaches and Comfort Measures
Treatment of painful urination in the context of prostate cancer depends on its underlying cause. If the symptom is linked to infection, antibiotics or antifungals are prescribed. Inflammatory causes may require anti-inflammatory medications, bladder instillations, or corticosteroids. For radiation-induced pain, protective agents like pentosan polysulfate sodium or sodium hyaluronate are sometimes used.
Patients undergoing hormonal therapy may benefit from dose adjustment or adjunct treatments for bladder irritation. In select cases, procedures like transurethral resection of the prostate (TURP) or temporary catheterization can reduce obstruction-related pain.
Symptom relief is critical for maintaining quality of life during cancer treatment.
Table: Treatment Options Based on Cause
| Cause | Management |
| Infection | Targeted antimicrobial therapy |
| Radiation cystitis | Bladder protectants, hydration, anti-inflammatories |
| Hormonal irritation | Therapy adjustment, local estrogen/urethral creams |
| Urethral obstruction | Catheter, TURP, alpha-blockers |
| Neuropathic pain | Gabapentin, antispasmodics |
Supportive care also includes adequate fluid intake, pain management, and pelvic floor relaxation techniques. In advanced stages, palliative care may offer integrated strategies for comfort and dignity.
Preventing Painful Urination During Treatment
Prevention of painful urination in men with prostate cancer centers on anticipating risk factors and minimizing damage to the urinary tract during treatment. Although not all causes can be avoided, careful planning and supportive care can reduce incidence and severity.
Prior to starting radiation, patients often undergo bladder training and receive bladder-protective agents. Adequate hydration, maintaining normal urinary pH, and avoiding irritants like caffeine, alcohol, and spicy food are simple yet effective preventive strategies.
Proactive infection monitoring is key—especially for those using catheters or experiencing incomplete voiding. Androgen deprivation therapy should be monitored closely for side effects that may increase urinary sensitivity.
Table: Prevention Strategies for Painful Urination
| Prevention Focus | Actions Taken |
| Radiation therapy prep | Hydration protocols, bladder conditioning |
| Infection prevention | Sterile catheter handling, regular urinalysis |
| Diet and fluid balance | Avoid bladder irritants, maintain urine dilution |
| Hormone therapy monitoring | Adjust doses if dysuria develops |
| Early symptom reporting | Allows timely intervention and reduces complications |
Patient education plays a vital role—those who understand the risks are more likely to report early symptoms, enabling fast and effective responses.
Will the Pain Go Away Over Time?

Whether painful urination resolves depends on its cause and the patient’s treatment status. For many, it is a temporary side effect of radiation or hormonal therapy, improving within weeks to months as tissues heal and inflammation subsides.
However, if pain stems from tumor obstruction or advanced prostate cancer, relief often requires targeted cancer therapy—such as surgery, radiation, or androgen suppression. Chronic irritation, scarring (especially post-radiation), or nerve damage may cause prolonged or recurring discomfort.
Prognosis Table: Will It Go Away?
| Source of Pain | Likelihood of Resolution |
| Radiation-induced inflammation | High (within 3–6 months) |
| Hormone therapy effects | Moderate (varies by patient) |
| UTI or prostatitis | High (with proper treatment) |
| Tumor obstruction | Moderate to low (requires intervention) |
| Nerve-related (neuropathic) | Variable, often needs chronic management |
Thus, for many, the pain does go away—especially with prompt symptom management. For others, it may become part of long-term survivorship care.
What Oncologists Say About Managing Urinary Pain
Practicing oncologists emphasize that painful urination should never be dismissed as “normal” or inevitable. According to clinicians, it often reflects a modifiable issue—whether treatment-related or disease-driven.
Urologic oncologists stress the importance of bladder protection during radiation, as well as infection screening before and after procedures. They advocate for the use of alpha-blockers and anticholinergics in select patients to ease bladder spasms.
Multidisciplinary cancer teams also recommend referring patients to pain specialists or palliative care if dysuria becomes chronic, especially in advanced disease. They reinforce the message that quality of life is a key treatment goal—not just cancer control.
One urologist summarized:
“Painful urination is common but manageable in prostate cancer. The key is not just treating the cancer, but caring for the whole person. We can usually reduce or eliminate the pain—if we act early and take it seriously.”
Questions to Ask Your Doctor
Before or during treatment, asking informed questions helps patients and caregivers prepare, understand risks, and participate in decision-making.
| Patient Question | Why It Matters |
| Is my pain related to the cancer or the treatment? | Determines the root cause |
| Could I have a urinary tract infection? | Guides antibiotic use |
| Will this pain go away after treatment ends? | Helps set expectations |
| Can I take medication to reduce the burning? | Improves comfort and adherence |
| Is it safe for me to drink more fluids? | Supports bladder health |
| Should I avoid any foods or drinks? | Prevents aggravation |
| Could radiation be causing this pain? | Triggers protective protocols |
| Are any of my drugs irritating my bladder? | Enables adjustments |
| Should I see a urologist or pain specialist? | For expert opinion and interventions |
| Will catheter use make the pain worse? | Addresses mechanical irritation |
| Can you check for scarring or strictures? | Structural problems may need surgery |
| How can I tell if it’s serious? | Flags warning signs |
| What options exist if the pain becomes chronic? | Palliative and supportive options |
| Are alpha-blockers or antispasmodics an option? | For flow and bladder control |
| How will this affect my sexual and urinary health? | Long-term quality of life considerations |
15+ FAQ: Painful Urination in Prostate Cancer
1. Is painful urination normal with prostate cancer?
It’s common, but not normal. It indicates irritation, inflammation, or tumor pressure that should be addressed.
2. Can radiation therapy cause it?
Yes. Radiation-induced cystitis is a major cause of burning and frequency in urination.
3. Will it get better after treatment ends?
In most cases, yes. Especially if caused by radiation or medication side effects.
4. Can painful urination mean the cancer is spreading?
It might—especially if new or worsening. It can indicate tumor growth or invasion.
5. How do I know it’s not a urinary infection?
Only urine testing and clinical evaluation can confirm or rule it out.
6. What medications help?
Alpha-blockers, anticholinergics, anti-inflammatories, or nerve pain drugs may help.
7. Is it safe to drink a lot of water?
Yes, unless contraindicated. Hydration often reduces bladder irritation.
8. Can food make it worse?
Yes—alcohol, caffeine, spicy or acidic foods may aggravate symptoms.
9. Should I use a heating pad?
Yes, gentle warmth may relieve pelvic discomfort, but check with your doctor.
10. Can I still take chemotherapy with this symptom?
Often yes—but the treatment plan may need to be adjusted if the pain worsens.
11. Will a catheter relieve the pain?
Sometimes, especially if caused by retention. But catheters may also irritate the urethra.
12. What if nothing helps?
Your oncologist may refer you to a pain specialist or supportive care team.
13. Could scarring be the issue?
Yes. Radiation and surgery can cause urethral narrowing or fibrosis.
14. Can painful urination lead to complications?
Yes—such as retention, infection, or poor hydration from fear of urinating.
15. Is it linked to other urinary symptoms?
Often. Burning can be accompanied by frequency, urgency, or weak stream.











