Pain Behind the Knee: Causes, Relief, and When to See a Doctor
Hello, I’m Dr. Emily Hart, MD. Pain behind the knee can range from simple overuse to conditions that need attention. In this guide, you’ll learn the most common causes, safe home steps that actually help, and the warning signs that mean it’s time to see a doctor.
- What “pain behind the knee” usually means
- Top causes: strain, Baker’s cyst, meniscus, arthritis
- Practical relief: movement, warm/cold, footwear
- When to seek care and what a doctor may check
What Does Pain Behind the Knee Mean?
Pain at the back of the knee is a frequent concern, but it can feel very different depending on the situation. Some people notice a dull ache after standing for long periods, while others describe a sharp pinch when bending, squatting, or climbing stairs. Because this area contains muscles, tendons, blood vessels, and the joint capsule, several structures can be responsible.

In many cases, discomfort comes from overuse or strain, especially after exercise that challenges the knee more than usual. However, it may also be related to a Baker’s cyst, meniscus irritation, or the first signs of arthritis. In rare cases, sudden severe pain in this area can be linked to circulation problems, which is why context and additional symptoms are important.
Recognizing what “pain behind the knee” can represent helps patients and doctors decide when rest and home care are enough — and when a proper medical evaluation is the safer path.
The Most Common Causes
Muscle Strain and Overuse
One of the most frequent reasons for pain behind the knee is simple muscle strain. Activities like running, cycling, or sudden increases in workout intensity can overload the hamstrings and calf muscles. This tension may radiate to the back of the knee, especially after long sessions or inadequate warm-up.
In most cases, the discomfort is temporary and eases with rest, gentle stretching, and hydration. However, if the pain persists beyond a few days or is severe enough to limit normal movement, a doctor’s evaluation can help rule out more significant injury.
Baker’s Cyst (Fluid Buildup)
A Baker’s cyst, also called a popliteal cyst, is a pocket of fluid that forms behind the knee. It usually develops when the knee produces excess joint fluid, often due to arthritis or a meniscus tear. The result is a noticeable swelling or tightness at the back of the joint, which may feel worse when the knee is fully bent.
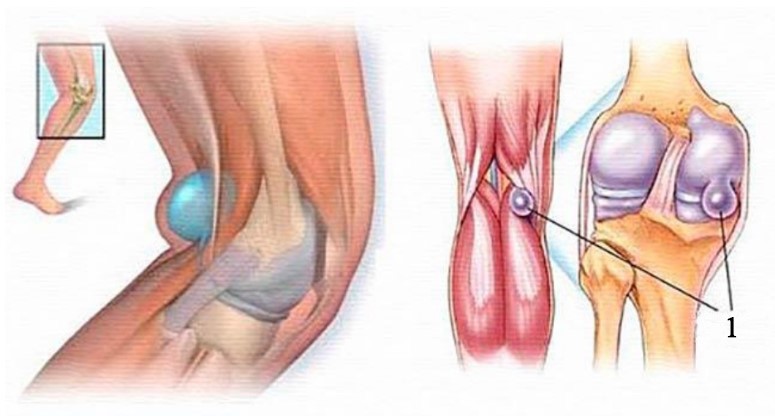
For many people, a Baker’s cyst causes only mild discomfort and sometimes even goes unnoticed. However, larger cysts can limit motion or create a sense of pressure during activity. While small cysts may improve on their own with rest and gentle activity, a doctor can confirm the diagnosis and recommend treatments if swelling or pain continues.
Meniscus Irritation or Tear
The meniscus is a C-shaped piece of cartilage that cushions the knee joint. When it becomes irritated or torn, pain can appear at the back or sides of the knee, often after a twist, squat, or sudden misstep. Some people describe a popping sensation at the time of injury, followed by swelling or stiffness.
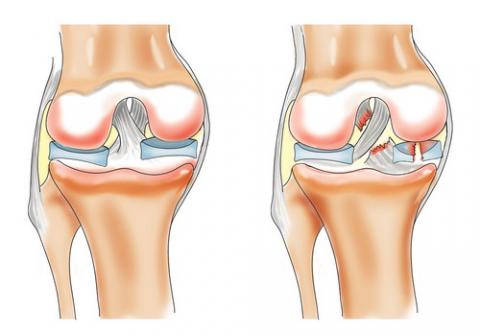
Minor meniscus irritation may cause only mild aching and improve with rest and gentle movement. In contrast, a significant tear can lead to catching, locking, or a knee that feels unstable. Because symptoms vary widely, a medical exam is often needed to determine whether the issue is temporary strain or a more serious injury that requires treatment.
Arthritis and Cartilage Changes
As joints age or undergo repeated stress, the smooth cartilage that protects the knee can begin to wear down. This process may cause aching, stiffness, and sometimes a grinding or cracking sensation when climbing stairs or standing up after rest. Pain behind the knee in these cases often develops gradually rather than suddenly.
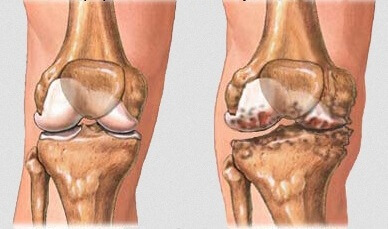
Osteoarthritis is the most common form, but inflammatory types of arthritis can also affect the back of the knee. While lifestyle changes, exercise, and weight management can reduce strain, ongoing or worsening discomfort should be assessed by a doctor to confirm the cause and discuss management options.
Rare but Serious: Blood Clot
Although uncommon, a blood clot in the deep veins of the leg (deep vein thrombosis, or DVT) can cause pain or pressure behind the knee. Unlike muscle strain or a cyst, this pain often comes with swelling, warmth, or a change in skin color. It may worsen when standing still for long periods or during travel.
Because a clot can be dangerous if it moves to the lungs, this scenario requires urgent medical care. Anyone who experiences sudden back-of-the-knee pain with swelling, redness, or unexplained heaviness should seek medical attention immediately rather than waiting for symptoms to pass.
Home Care and Self-Relief
Most people with mild pain behind the knee can try simple steps at home before seeking medical care. Resting the joint after long activity, applying a warm compress or gentle ice pack, and using supportive shoes often make a noticeable difference. Light stretching of the hamstrings and calves can also ease tension that builds up at the back of the leg.
From my experience, patients sometimes assume that complete rest is best, but gentle movement is usually more helpful. Short walks, light cycling, or basic mobility exercises keep the joint from stiffening and improve circulation. What matters most is to avoid sudden, heavy strain right after a break or long sitting.
Supportive footwear and cushioned insoles can reduce stress on the knee, especially during exercise or daily routines. In many cases, this small change lessens discomfort significantly. While home care cannot fix every cause of knee pain, these steps often provide relief and create a safer base if further treatment is needed.
Knee Braces and Supports
Knee braces and elastic sleeves are often used to stabilize the joint and reduce discomfort. They work by providing mild compression, which can limit swelling, and by offering mechanical support that helps the knee feel more secure during movement. There are several types — from simple elastic sleeves to structured braces with hinges designed for sports or injury recovery.

In practice, these supports can be most helpful for people with instability after a minor injury or those returning to activity after a period of rest. I often remind patients that braces are not a cure; they do not repair cartilage or ligaments, but they can reduce pain during daily tasks or exercise.
Choosing the right type depends on the situation: soft sleeves for mild symptoms, more rigid models only under medical guidance. Over-relying on a brace without strengthening the surrounding muscles can sometimes slow long-term recovery. For that reason, I usually suggest combining supportive gear with gradual exercise rather than using it as the only solution.
ICD-10 Codes for Knee Pain
In medical records, knee pain is often classified using ICD-10 codes. These codes are used by doctors and insurance providers to describe the exact location of the problem. Knowing them is not essential for patients, but it helps when reviewing medical documents or discussing billing.
Here are the most common codes:
| Code | Description | Notes |
|---|---|---|
| M25.561 | Pain in right knee | Used when pain is primarily on the right side |
| M25.562 | Pain in left knee | Used when pain is primarily on the left side |
| M25.569 | Pain in unspecified knee | When the side is not clearly documented |
From a patient’s perspective, these numbers simply translate a symptom into a standardized format. For doctors and insurers, they provide clarity and consistency. If you see one of these codes in your paperwork, it refers to the location of the knee pain rather than a specific diagnosis.
When to See a Doctor
Most back-of-the-knee discomfort improves with simple care, but some signs mean it’s safer not to wait.
Seek medical attention if you notice:
- sudden sharp pain after a twist or misstep,
- swelling, warmth, or redness that develops quickly,
- a feeling of instability or locking when you try to move,
- pain that lingers for more than a week despite rest.
In my practice, many patients are unsure whether their symptoms are “serious enough.” I usually explain that it’s better to get checked if pain interrupts sleep, prevents normal walking, or comes with visible swelling.
During an evaluation, a doctor may start with a physical exam and history of the pain. Imaging such as ultrasound, X-ray, or MRI is considered only if symptoms or exam findings suggest a more specific problem. Often, recommendations include physical therapy, load adjustment, or anti-inflammatory medications prescribed under supervision.
Expert Conclusion
Back-of-the-knee discomfort rarely points to something dangerous on its own. What matters is the context: how the pain started, whether it limits movement, and which activities make it worse. In my practice, most people feel better with small, consistent changes rather than dramatic fixes.
- Move gently, but regularly: short walks, light mobility, and gradual return to activity help more than full rest.
- Support the basics: warm-up, simple stretches, hydration, and footwear with good cushioning reduce day-to-day strain.
- Use tools wisely: sleeves and braces can add comfort, but they’re a complement to strengthening—not a replacement.
If your pain arrives with swelling, locking, or a sudden sharp onset after a twist or fall, that’s a good reason to get checked. Otherwise, steady habits and patient progress are usually enough to settle symptoms and keep you moving.
FAQ
Is pain behind the knee serious?
Often it isn’t. Overuse or minor strain is common and improves with rest and gentle movement. See a doctor if pain comes with swelling, warmth, locking, or sudden onset after a twist or fall.
What causes pain behind my knee after exercise?
Most often, tight hamstrings or calf strain after a hard session or poor warm-up. Easing back on intensity, adding mobility work, and using supportive shoes usually helps. Persistent pain despite rest deserves an evaluation.
How do I know if it’s a Baker’s cyst?
Typical clues are a soft, full feeling or visible bulge behind the knee that worsens with deep bending. Only a clinician can confirm it—often with an exam and, if needed, ultrasound. Seek care if swelling is painful or limits motion.
Can a meniscus problem cause pain at the back of the knee?
Yes. A twist or squat can irritate or tear the meniscus and produce back-of-knee pain, sometimes with catching or locking. If symptoms linger or the knee feels unstable, get checked by a specialist.
Do knee braces help with pain behind the knee?
They can—by adding gentle compression and support during activity. Braces don’t fix the underlying issue, so pair them with strengthening and gradual training. Choose type with a clinician’s advice if symptoms are ongoing.
Which home remedies actually help?
Short rest, warm-up or brief icing, light stretching, hydration, and cushioned footwear are reliable first steps. Gentle activity beats total rest for most people. Stop and seek care if pain escalates or function drops.
When should I get imaging (ultrasound, X-ray, MRI)?
Imaging is used when symptoms or exam findings suggest a specific problem—like persistent swelling, locking, or trauma. Ultrasound looks at soft tissues, X-ray at bone alignment, and MRI for cartilage/ligaments. It’s not routine for mild, improving symptoms.
Could pain behind the knee be a blood clot?
Rarely, but it’s important. Warning signs include swelling, warmth, redness, and unexplained heaviness, especially after travel or immobilization. Treat these as urgent and seek medical care immediately.
Sources / References
- Cleveland Clinic — Baker’s Cyst: Symptoms and treatment
- Johns Hopkins Medicine — Knee pain and common problems
- Arthritis Foundation — Knee pain and arthritis