Ovarian Cancer MRI
Ovarian Cancer MRI: A Complete Beginner’s Guide
- What Is an Ovarian Cancer MRI?
- When Is MRI Recommended for Ovarian Cancer?
- How MRI Detects and Characterizes Ovarian Tumors
- Comparing MRI with Other Imaging Modalities
- How to Prepare for an Ovarian MRI Scan
- Understanding Ovarian MRI Scan Results
- Role of MRI in Surgical Planning for Ovarian Cancer
- Limitations of MRI in Ovarian Cancer Diagnosis
- MRI vs CT in Ovarian Cancer Staging
- Using MRI to Detect Ovarian Cancer Recurrence
- MRI Appearance of Different Ovarian Cancer Subtypes
- Special MRI Considerations for Young Women and Pregnancy
- Cost and Accessibility of MRI for Ovarian Cancer
- MRI for Monitoring Treatment Response in Ovarian Cancer
- Multidisciplinary Use of MRI in Cancer Care
- Emerging Research and Future Directions
- FAQ: 15 Key Questions About Ovarian Cancer MRI Not Covered Above
What Is an Ovarian Cancer MRI?
MRI (Magnetic Resonance Imaging) for ovarian cancer is a non-invasive imaging technique that uses magnetic fields and radio waves to create detailed images of the ovaries, fallopian tubes, uterus, and surrounding tissues. It plays a critical role in identifying suspicious masses, evaluating their structure, and determining whether a tumor is likely benign or malignant.
MRI does not use radiation, which makes it especially suitable for younger women or those needing frequent follow-ups. It offers superior soft tissue contrast compared to CT scans and ultrasound, making it ideal for characterizing ovarian lesions and planning surgery.
In oncology settings, MRI is often used in conjunction with other diagnostics such as transvaginal ultrasound or CA-125 blood tests to improve diagnostic accuracy.
When Is MRI Recommended for Ovarian Cancer?
MRI is not always the first imaging tool used. Most initial evaluations begin with ultrasound. However, MRI is highly recommended in several situations, especially when results from other tests are inconclusive.
| Clinical Scenario | Why MRI Is Useful |
| Indeterminate ovarian mass on ultrasound | MRI helps differentiate benign from malignant tumors |
| Suspected spread beyond ovaries | MRI maps pelvic and abdominal involvement |
| Pre-surgical planning | Detailed imaging helps plan extent of surgery |
| Monitoring during or after treatment | MRI tracks tumor response or detects recurrence |
| Patients unable to undergo CT (e.g. allergies) | MRI offers alternative without contrast risks |
MRI is also preferred for women with dense tissue or when detailed visualization of soft tissues and lymph nodes is necessary.
How MRI Detects and Characterizes Ovarian Tumors
MRI is especially skilled at tissue differentiation, helping radiologists assess the tumor’s structure, content, and surrounding environment. Ovarian tumors vary widely—from fluid-filled cysts to solid malignant growths—and MRI’s contrast helps define each component with clarity.
Infographic: Tumor Characterization on MRI
- Cystic Lesions: Appear with clear fluid and thin walls
- Solid Tumors: Show irregular, enhancing tissue
- Complex Masses: Contain both solid and cystic components
- Hemorrhagic Cysts: Display blood content and internal shading
- Fat-containing Lesions (e.g., dermoids): Show fat signal on T1-weighted images
MRI also evaluates lymph node involvement and peritoneal spread, crucial for staging and treatment planning.
Comparing MRI with Other Imaging Modalities
Each imaging modality has strengths and limitations. The role of MRI must be evaluated in context with ultrasound and CT scans.
| Feature | Ultrasound | CT Scan | MRI |
| Radiation Exposure | None | Uses radiation | No radiation |
| Tissue Differentiation | Moderate | Moderate | Excellent for soft tissues |
| Accessibility | Widely available | Widely available | Less common, specialized centers |
| Best For | Initial mass detection | Staging, metastasis | Characterizing complex masses |
| Use of Contrast | Sometimes | Yes (iodine-based) | Yes (gadolinium, safer for kidneys) |
MRI is often the “tie-breaker” when ultrasound and CT offer conflicting data or when more anatomical detail is necessary.
How to Prepare for an Ovarian MRI Scan
Preparing for an ovarian MRI involves several basic steps to ensure image clarity and patient comfort. Most patients are not required to follow a strict diet before the scan, but some facilities may request fasting for a few hours. A contrast-enhancing agent (gadolinium) is often injected during the scan to improve visualization of blood supply to tissues.
| Preparation Step | Purpose |
| Wear metal-free clothing | Prevent magnetic interference |
| Empty bladder (or follow clinic protocol) | Avoid image distortion |
| Inform about implants/pacemakers | MRI safety check |
| Contrast injection preparation | Used unless contraindicated (e.g. allergy, pregnancy) |
| Anxiety or claustrophobia | May require sedation or open MRI |
Patients should inform technicians of any history of kidney problems, as contrast agents are processed via the kidneys. Pregnant women, especially in the first trimester, are evaluated carefully before proceeding.
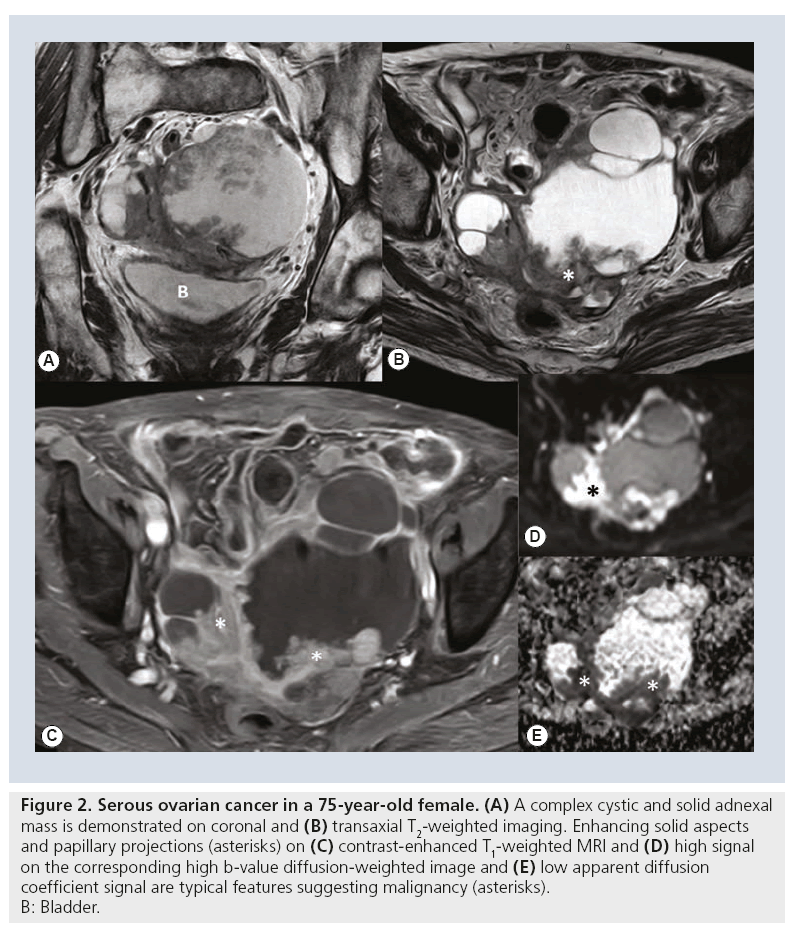
Understanding Ovarian MRI Scan Results
After the MRI scan is complete, radiologists analyze the images using specific sequences and contrast effects. Reports include descriptions of lesion size, shape, borders, contents (solid, cystic, mixed), and any enhancement patterns post-contrast.
Infographic: Key Terms in an MRI Report
- “T1-weighted” / “T2-weighted” — refer to MRI sequences with different contrasts
- “Hyperintense” — area appears brighter than normal tissue
- “Hypointense” — area appears darker
- “Enhancement” — region absorbs contrast, indicating blood flow
- “Septation” — internal divisions within a cyst, can suggest malignancy
- “Restricted diffusion” — limited water movement, often seen in cancer
These technical terms help determine whether a mass is likely benign, borderline, or malignant. Surgeons and oncologists use this data to make informed decisions about next steps.
Role of MRI in Surgical Planning for Ovarian Cancer
MRI provides highly detailed information that helps gynecologic oncologists determine how extensive surgery needs to be. The imaging helps identify tumor boundaries, involvement of adjacent organs, and potential spread to lymph nodes or peritoneal surfaces.
| Surgical Factor | How MRI Helps |
| Tumor size and origin | Distinguishes between ovarian, uterine, or gastrointestinal tumors |
| Spread to uterus or bladder | Assesses need for multi-organ resection |
| Lymph node involvement | Guides staging surgery and lymphadenectomy |
| Peritoneal metastasis | Determines need for cytoreductive surgery or HIPEC |
MRI findings may also help predict whether optimal debulking is achievable or if neoadjuvant chemotherapy should be considered before surgery.
Limitations of MRI in Ovarian Cancer Diagnosis
Despite its many strengths, MRI has several limitations when used for ovarian cancer assessment. It is not typically used as a screening tool for asymptomatic women and cannot detect microscopic metastases or early peritoneal implants.
| Limitation | Explanation |
| Low specificity for some masses | Certain benign tumors may mimic malignancy on MRI |
| High cost and limited access | MRI is more expensive and less available than ultrasound |
| Not effective for micrometastasis | May miss very small peritoneal or lymph node metastases |
| Requires expertise for interpretation | Misinterpretation possible in non-specialist settings |
This underscores the need to combine MRI with clinical data, tumor markers, and other imaging for a comprehensive diagnosis. In some patients, especially those with overlapping symptoms like cervical involvement, a differential analysis is important — Cervical Cancer vs. Ovarian Cancer Comparison
MRI vs CT in Ovarian Cancer Staging
Both MRI and CT scans play roles in ovarian cancer staging, but their use depends on the clinical question, tumor type, and institutional preference. CT scans are generally preferred for detecting distant metastases, while MRI is more useful for detailed pelvic anatomy and tissue characterization.
| Criteria | MRI Strength | CT Strength |
| Soft tissue definition | Excellent — distinguishes tissue types | Moderate — limited pelvic detail |
| Distant metastasis detection | Moderate — less effective in upper abdomen | Strong — visualizes lungs, liver, peritoneum |
| Radiation exposure | None | Uses ionizing radiation |
| Pre-surgical pelvic mapping | Superior pelvic resolution | Useful for surgical logistics, not anatomy |
| Lymph node assessment | Good but operator-dependent | Readily identifies enlarged nodes |
While CT is often used to assess overall disease burden, MRI’s accuracy in distinguishing malignant from benign pelvic masses makes it indispensable in many cases.
Using MRI to Detect Ovarian Cancer Recurrence
MRI is frequently used to monitor for recurrence after treatment, especially in patients with elevated CA-125 or nonspecific symptoms. It helps differentiate scar tissue from active disease, which is often difficult with CT or ultrasound.
Infographic: Signs of Recurrence Visible on MRI
- New or enlarging masses in pelvis or abdomen
- Peritoneal implants with contrast enhancement
- Ascites (fluid buildup) not previously seen
- Lymph node enlargement near iliac or para-aortic chains
- Restricted diffusion indicating aggressive tissue growth
MRI may detect subtle disease in areas like the rectovaginal septum or pelvic sidewall — locations often missed by other scans. For patients also undergoing prostate monitoring or comorbidities, it’s essential to distinguish findings from other sources Prostate Cancer.
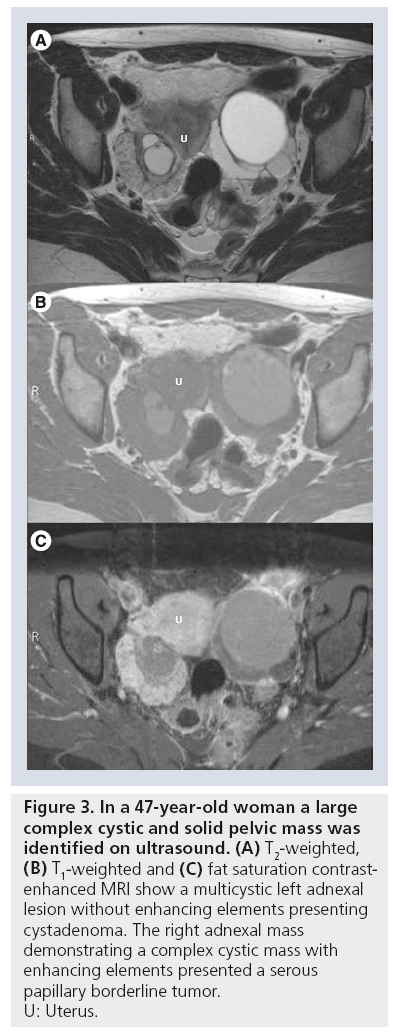
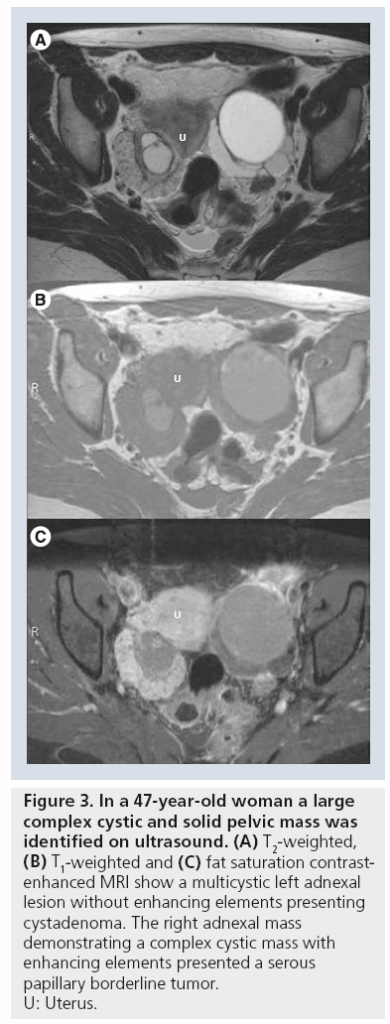
MRI Appearance of Different Ovarian Cancer Subtypes
Different histological subtypes of ovarian cancer present differently on MRI. Recognizing these variations can help radiologists suggest the likely tumor type even before biopsy.
| Subtype | MRI Characteristics |
| Serous carcinoma | Bilateral, solid-cystic, papillary projections, ascites |
| Mucinous carcinoma | Large unilateral multilocular mass with thick septations |
| Endometrioid carcinoma | Solid or mixed mass, may resemble endometriosis |
| Clear cell carcinoma | Hyperintense cystic areas, hemorrhagic features |
| Germ cell tumors | Fat and calcification components (e.g., in teratomas) |
These MRI patterns guide further testing and can help avoid unnecessary surgery in cases where a tumor appears clearly benign or classic for a specific subtype.
Special MRI Considerations for Young Women and Pregnancy
MRI is especially useful for assessing ovarian masses in younger women, including adolescents and pregnant patients, due to its safety and precision without radiation exposure.
| Patient Type | MRI Benefit |
| Adolescents | Characterizes congenital or rare ovarian tumors |
| Pregnant patients | No ionizing radiation; safe after first trimester |
| Fertility preservation candidates | MRI helps guide surgery that preserves ovarian tissue |
| Women with PCOS or cysts | Differentiates benign cysts from early neoplasms |
In pregnancy, MRI is typically reserved for complex masses or when ultrasound findings are inconclusive. Sedation is usually avoided, and contrast agents are only used if absolutely necessary.
Cost and Accessibility of MRI for Ovarian Cancer
MRI scans are more expensive than ultrasound and CT, and their availability is limited in some regions. Cost varies depending on geography, insurance coverage, type of facility, and whether contrast is used.
| Factor | Typical Range / Consideration |
| Cost without insurance | $800 – $2,500 per scan (USA data) |
| With insurance | Often partially or fully covered with oncologist referral |
| Wait time in public hospitals | May range from days to weeks |
| Accessibility in rural areas | Often requires travel to major centers |
| Alternative imaging options | May be used if MRI is unavailable |
Patients are encouraged to discuss cost with providers and insurers. Many hospitals offer financial assistance or tiered payment plans.
MRI for Monitoring Treatment Response in Ovarian Cancer
MRI plays a key role during and after treatment to evaluate how well tumors are responding to chemotherapy, radiation, or targeted therapies. This is especially helpful in borderline resectable or advanced-stage cases.
Infographic: Treatment Monitoring via MRI
- Tumor shrinkage: decrease in volume and contrast uptake
- Tissue necrosis: loss of blood flow in tumor center
- Cyst resolution: reabsorption of fluid components
- Lymph node changes: reduction in size or normalization
- Reduced ascites: less fluid accumulation in pelvis/abdomen
MRI allows doctors to distinguish between active tumor and fibrotic tissue, which is vital for deciding on continued treatment vs. surgical intervention.
Multidisciplinary Use of MRI in Cancer Care
MRI findings are not interpreted in isolation. Radiologists work closely with oncologists, gynecologic surgeons, and pathologists in a multidisciplinary tumor board setting to create patient-specific treatment plans.
| Specialist | MRI Contribution to Their Role |
| Radiologist | Interprets lesion structure, spread, and behavior |
| Gynecologic Oncologist | Plans surgical approach, assesses resectability |
| Medical Oncologist | Adjusts chemo or immunotherapy based on MRI outcomes |
| Radiation Oncologist | Evaluates areas needing radiation |
| Pathologist | Correlates tissue findings with imaging |
This integrated approach enhances treatment precision and improves survival and quality of life for patients.
Emerging Research and Future Directions

Recent innovations in MRI technology are expanding its diagnostic and prognostic capabilities in ovarian cancer. Research is focused on improving image resolution, reducing scan time, and integrating artificial intelligence (AI).
| Area of Innovation | Description |
| Diffusion-weighted imaging (DWI) | Enhances ability to detect cellular activity |
| Functional MRI | Evaluates tumor metabolism and blood flow |
| AI-powered diagnostics | Automatically classifies masses using large datasets |
| Whole-body MRI | One-scan assessment for staging without radiation |
| Radiogenomics | Links imaging features with genetic markers |
These developments may soon allow earlier, non-invasive diagnosis and better individualized treatment planning, changing the way ovarian cancer is managed worldwide.
FAQ: 15 Key Questions About Ovarian Cancer MRI Not Covered Above
1. Can MRI detect early-stage ovarian cancer?
While MRI provides excellent detail, it is not typically used for routine screening. However, it can identify early-stage tumors if imaging is performed for other reasons or after abnormal findings.
2. Is contrast always necessary for an ovarian MRI?
Most diagnostic ovarian MRIs use gadolinium contrast to enhance clarity, especially for tumor characterization. In patients with kidney issues or during pregnancy, contrast may be avoided.
3. Does an MRI replace a biopsy?
No. MRI suggests whether a tumor is likely benign or malignant, but only a biopsy provides a definitive diagnosis.
4. How long does an ovarian MRI take?
The procedure typically lasts between 30 and 60 minutes, depending on the use of contrast and the number of sequences taken.
5. Will an MRI scan show if ovarian cancer has spread?
MRI can show local and regional spread (e.g., to uterus, bladder, lymph nodes), but whole-body CT or PET/CT is more effective for detecting distant metastases.
6. Is it safe to have multiple MRI scans?
Yes. MRI uses no radiation, making it safe for repeated imaging, especially useful for long-term monitoring.
7. Can MRI be used during chemotherapy?
Yes, MRI is often used mid-treatment to evaluate tumor response and guide potential surgical planning or changes in therapy.
8. Is an MRI better than ultrasound for ovarian masses?
MRI offers superior soft tissue contrast and is better at characterizing complex or indeterminate masses seen on ultrasound.
9. Will I be exposed to radiation during MRI?
No. MRI uses magnetic fields and radio waves — there is no ionizing radiation involved.
10. Can MRI identify borderline ovarian tumors?
MRI can suggest features of borderline tumors (e.g., septations, papillary projections), but final diagnosis requires pathology.
11. Is MRI safe during menstruation?
Yes. Menstrual cycle does not interfere with MRI performance, although timing may be adjusted for certain pelvic evaluations.
12. What’s the difference between T1 and T2 in MRI?
T1 and T2 are imaging sequences. T1 shows fat as bright and fluid as dark; T2 shows fluid as bright. This contrast helps characterize tissue content.
13. Can MRI differentiate between ovarian and cervical cancer?
Yes. MRI can delineate the origin and relationship of pelvic tumors.
14. Does MRI detect tumors that blood tests miss?
Yes. Blood tests like CA-125 can miss some tumors, especially early or low-grade cancers. MRI adds critical anatomical detail.
15. Is MRI helpful in recurrent ovarian cancer after surgery?
Absolutely. MRI is one of the best tools for detecting local recurrence, especially when combined with rising CA-125 levels and clinical symptoms.