Niacinamide for Skin Cancer
Niacinamide for Skin Cancer: Understanding Its Role in Prevention and Care
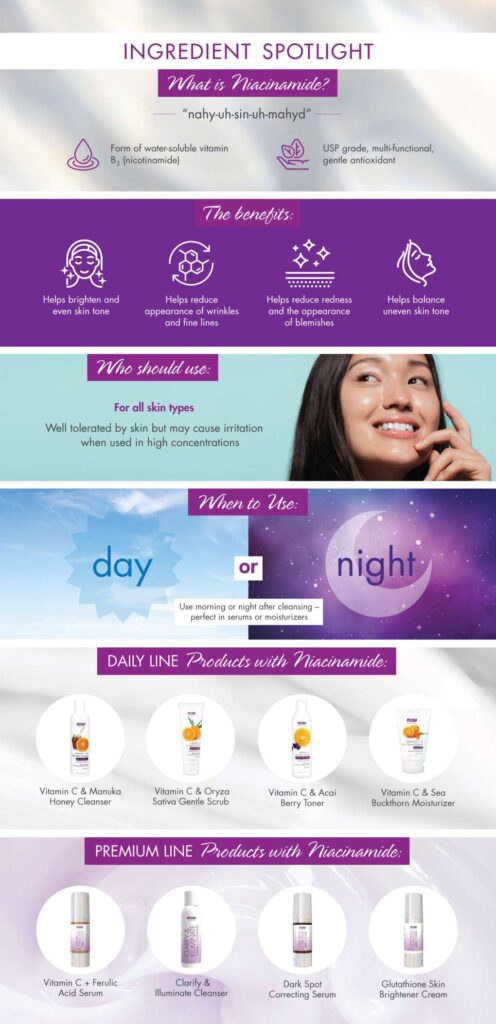
- What Is Niacinamide and How Does It Work in the Skin?
- The Scientific Connection Between Niacinamide and Skin Cancer
- Types of Skin Cancer Most Impacted by Niacinamide
- Topical vs. Oral Niacinamide: Which Is More Effective?
- Does Niacinamide Reduce Risk of Basal and Squamous Cell Carcinoma?
- Can Niacinamide Be Used Alongside Conventional Cancer Therapies?
- How Niacinamide Supports Immune Function in the Skin
- Comparing Niacinamide With Other Preventive Strategies
- Topical vs. Oral Niacinamide: What’s More Effective?
- Recommended Dosage and Duration for Skin Cancer Prevention
- Can Niacinamide Prevent Melanoma?
- Is Niacinamide Safe for Long-Term Use?
- Who Should Consider Niacinamide for Skin Cancer Prevention?
- Interactions with Other Supplements or Medications
- Is Niacinamide Effective Without Sunscreen?
- Summary: Should You Take Niacinamide?
- FAQ: Niacinamide and Skin Cancer – 15 Key Questions Answered
What Is Niacinamide and How Does It Work in the Skin?

Niacinamide, also known as nicotinamide, is a form of vitamin B3 that plays a crucial role in skin cell health. It supports cellular energy production and helps repair DNA damage caused by ultraviolet (UV) radiation—one of the main risk factors for skin cancer. Unlike some topical agents that only work on the skin’s surface, niacinamide penetrates deeply to enhance barrier function, reduce inflammation, and improve immunity.
In dermatology, niacinamide is prized for its multitasking capabilities: it reduces redness, repairs skin, minimizes pigmentation, and increases the skin’s resilience. Importantly, these effects contribute to a defense against carcinogenic changes in cells triggered by sun exposure and oxidative stress.
The Scientific Connection Between Niacinamide and Skin Cancer
Multiple peer-reviewed studies have investigated the preventive role of niacinamide in skin cancer, particularly in nonmelanoma types such as basal cell carcinoma (BCC) and squamous cell carcinoma (SCC). In a landmark 2015 clinical trial conducted in Australia, patients with a history of nonmelanoma skin cancers were given 500 mg of oral niacinamide twice daily for 12 months. The results showed a 23% reduction in new skin cancers compared to the placebo group.
This effect is attributed to niacinamide’s ability to enhance DNA repair in keratinocytes, the main cell type in the epidermis. It also inhibits immunosuppression caused by UV radiation, allowing the immune system to better identify and eliminate abnormal cells. These combined effects offer a non-invasive, affordable, and safe prevention strategy—especially for individuals with high sun exposure or a family history of skin cancers.
Types of Skin Cancer Most Impacted by Niacinamide
Although niacinamide is not a cure or treatment for existing malignancies, it shows promise in preventing specific types of skin cancer, particularly nonmelanoma forms. Below is a table outlining the common types and how niacinamide may influence them:
| Skin Cancer Type | Effect of Niacinamide | Notes |
| Basal Cell Carcinoma (BCC) | May reduce occurrence by promoting DNA repair and reducing inflammation | See related topic: Basal Cell Skin Cancer |
| Squamous Cell Carcinoma | Strongest evidence of reduced risk, especially in high-risk populations | Supported by clinical trials |
| Melanoma | No significant evidence for prevention or treatment | Melanoma requires more aggressive surveillance |
The strongest evidence of niacinamide’s benefit is found in actinic keratoses, which are considered precancerous lesions that often precede SCC. Regular use has been shown to reduce the number and severity of these lesions.
Topical vs. Oral Niacinamide: Which Is More Effective?
The method of administration significantly affects niacinamide’s bioavailability and utility in cancer prevention. While topical creams and serums are effective for improving skin tone and hydration, the systemic benefits—especially those related to DNA repair—are primarily seen with oral supplementation.
| Form | Use Case | Cancer Prevention Benefit |
| Oral Capsule | Systemic protection, high UV exposure, medical history | Best for reducing new cancer formation |
| Topical Cream | Cosmetic use, local barrier support | Limited data on cancer-related benefits |
From the research available, oral niacinamide at a dose of 500 mg twice daily appears to provide the most consistent benefit in reducing new cancer formations, particularly in older adults and immunocompromised individuals.
Does Niacinamide Reduce Risk of Basal and Squamous Cell Carcinoma?
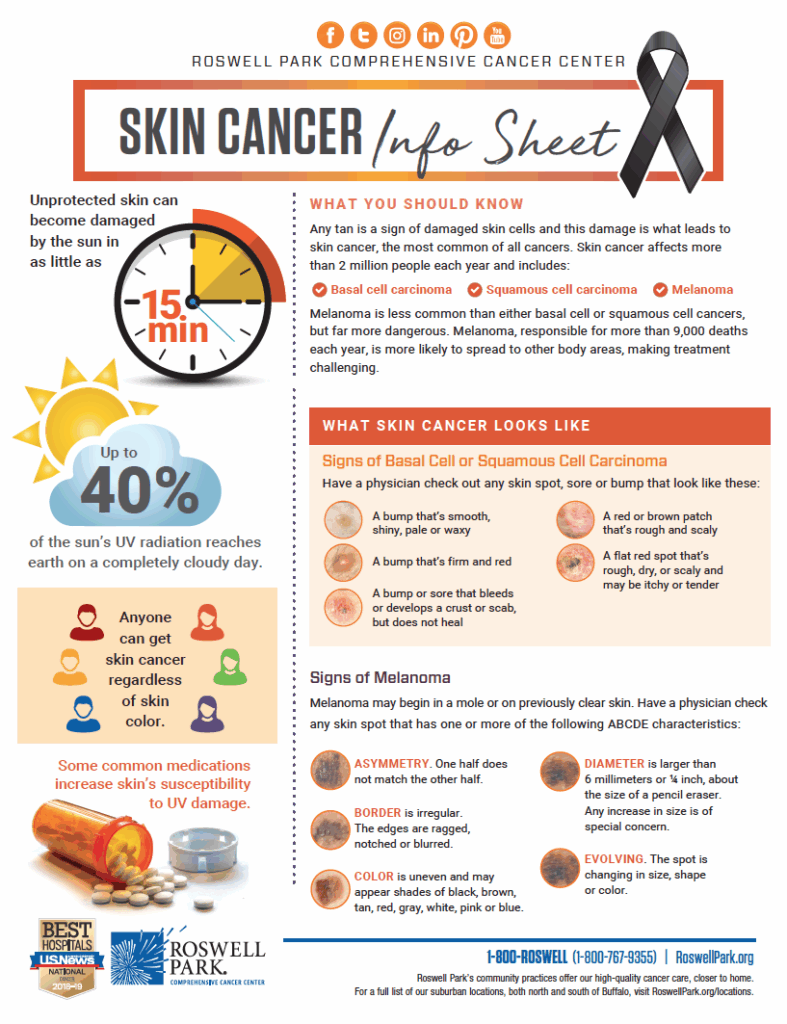
Both basal cell carcinoma (BCC) and squamous cell carcinoma (SCC) are categorized as nonmelanoma skin cancers, and they make up the majority of diagnosed skin cancers worldwide. BCC tends to grow slowly and rarely spreads, while SCC can be more aggressive and may metastasize if untreated.
In clinical trials, niacinamide has demonstrated significant efficacy in reducing the rate of new BCC and SCC occurrences, particularly among individuals who previously had these cancers. The mechanism includes:
- Enhanced repair of UV-induced DNA damage in keratinocytes
- Suppression of UV-related immune suppression
- Stabilization of cellular function under oxidative stress
For patients with a history of multiple nonmelanoma skin cancers, dermatologists may recommend niacinamide supplements as a preventative measure. Its accessibility, affordability, and lack of serious side effects make it a viable adjunct therapy.
Can Niacinamide Be Used Alongside Conventional Cancer Therapies?
Niacinamide is not a standalone cancer therapy, but it can complement conventional treatments such as surgery, chemotherapy, and radiation in a supportive role. Its benefits include mitigating skin irritation, boosting immune repair, and improving skin resilience—especially after sun exposure or radiation therapy.
However, patients undergoing active cancer treatment should consult their oncologist before introducing any new supplement, including vitamins. There is no evidence that niacinamide interferes with chemotherapy agents, but high doses may influence nutrient metabolism in certain settings. When used under medical supervision, niacinamide can be part of an integrative care approach.
Additionally, in the context of radiation-induced dermatitis, topical niacinamide may help reduce inflammation and speed up skin recovery, making it an appealing adjunct to post-treatment skincare regimens.
How Niacinamide Supports Immune Function in the Skin
A key contributor to cancer prevention is the immune system’s ability to detect and destroy mutated or abnormal cells. Chronic sun exposure can suppress this defense, allowing pre-cancerous cells to proliferate unnoticed.
Niacinamide has been shown to:
- Enhance local skin immunity
- Prevent UV-induced immunosuppression
- Support natural killer (NK) cell function in skin tissue
This immune-boosting effect is especially valuable in older individuals or those who are immunocompromised. For instance, transplant patients on long-term immunosuppressants face a higher risk of developing SCC. For these populations, oral niacinamide can play a protective role.
Recent data also show a synergistic benefit when niacinamide is used in combination with regular skin screening and sun protection, amplifying the overall protective effect.
Comparing Niacinamide With Other Preventive Strategies
Niacinamide is just one of several options available for reducing skin cancer risk. How does it compare with more traditional preventive tools like sunscreen, retinoids, or antioxidants? The table below outlines key comparisons:
| Strategy | Primary Mechanism | Cancer Prevention Role |
| Sunscreen (SPF 30+) | UV-blocking agent | Essential first-line defense |
| Retinoids (e.g., tretinoin) | Promote skin cell turnover | May reduce actinic keratoses |
| Niacinamide | DNA repair and immune modulation | Reduces recurrence in high-risk patients |
| Antioxidants (vitamin C/E) | Scavenge free radicals | Adjunct role, less robust in clinical data |
Niacinamide stands out for its dual role: it doesn’t just protect from future damage—it also helps repair damage that’s already occurred. Its role is best viewed as complementary, not competitive, to other preventive approaches.
Also worth noting: individuals with sensitive skin who can’t tolerate retinoids often find niacinamide a gentler yet effective alternative.
Topical vs. Oral Niacinamide: What’s More Effective?
Niacinamide is available in both topical formulations (creams, serums) and oral supplements. Each has distinct advantages depending on the context:
- Topical niacinamide is widely used in skincare for its anti-inflammatory, anti-aging, and barrier-supporting effects. It is especially helpful for patients managing actinic damage or recovering from dermatological procedures.
- Oral niacinamide, on the other hand, has been studied for its systemic effects on skin cancer prevention. Most notable is a 2015 study published in The New England Journal of Medicine, which demonstrated a 23% reduction in new nonmelanoma skin cancers among high-risk patients who took 500 mg of niacinamide twice daily for 12 months.
While both routes can be beneficial, oral niacinamide has more robust evidence for cancer prevention. However, combining both may offer synergistic benefits for patients with chronic photodamage.
Recommended Dosage and Duration for Skin Cancer Prevention
The optimal dosage for skin cancer prevention has been established through several clinical studies, with 500 mg taken twice daily as the most common and effective regimen. This dose is considered safe and well-tolerated by the majority of patients when taken short-term (up to 12 months).
| Factor | Recommendation |
| Dosage | 500 mg orally, twice daily |
| Treatment Duration | 6 to 12 months |
| Best Candidates | High-risk patients with past NMSC |
| Medical Supervision Needed? | Yes, especially for long-term use |
Patients with liver disease or chronic alcohol use may require additional monitoring. It is also important not to confuse niacinamide with niacin (nicotinic acid), which can cause flushing and liver toxicity at high doses.
Can Niacinamide Prevent Melanoma?
The protective effects of niacinamide have been well-documented in cases of basal and squamous cell carcinoma, but its impact on melanoma remains less clear. Melanoma arises from melanocytes rather than keratinocytes and follows a different genetic pathway.
So far, there is limited evidence that niacinamide prevents melanoma. Some early-stage lab studies suggest niacinamide may influence cellular signaling pathways that play a role in melanoma development, but these findings have not yet been confirmed in large human trials.
Therefore, niacinamide should not be relied upon as a preventive tool for melanoma. Standard prevention strategies—sun protection, skin surveillance, and early biopsy—remain critical.
However, people using niacinamide for nonmelanoma protection are encouraged to remain vigilant about skin without a rash that changes in appearance, as this may indicate a different skin condition or malignancy.
Is Niacinamide Safe for Long-Term Use?
Overall, niacinamide has an excellent safety profile. Unlike high-dose niacin, it does not typically cause flushing or liver toxicity. In doses under 1500 mg per day, it is well tolerated by most people.
However, long-term use beyond 12 months for cancer prevention has not been extensively studied. Patients should consult with their healthcare provider before extending therapy beyond the proven 12-month regimen. Side effects, while rare, can include:
- Mild gastrointestinal upset
- Fatigue or headache
- Altered liver enzyme levels (with very high doses)
For most individuals, especially those with a history of dangerous skin cancer, the benefits of niacinamide outweigh the potential risks when used appropriately.
Who Should Consider Niacinamide for Skin Cancer Prevention?

Niacinamide is not meant for everyone, but there are well-defined groups that benefit the most. These include patients with:
- A history of nonmelanoma skin cancer (especially more than two cases in the past five years)
- Actinic keratoses (precancerous skin lesions)
- Immunosuppression (e.g., organ transplant recipients)
- Chronic sun exposure with visible photodamage
Patients who fall into these categories should speak with a dermatologist about initiating niacinamide therapy. For those at average risk, standard sun protection and surveillance remain primary tools.
Recent research also explores niacinamide use in conjunction with therapies for basal cell skin cancer, especially among high-risk patients undergoing excision or Mohs surgery.
Interactions with Other Supplements or Medications
Niacinamide is generally well tolerated and does not interact significantly with most medications. However, it’s important to monitor when taken alongside:
- Statins or blood pressure meds – theoretical risk of affecting liver enzyme metabolism
- Antidiabetics – may enhance insulin sensitivity, potentially requiring dose adjustment
- Chemotherapy agents – limited research, so professional oversight is essential
Patients already taking multivitamins, especially those with high B-vitamin content, should avoid doubling up. Always consult with a healthcare provider before combining niacinamide with other treatments, particularly if undergoing cancer therapy.
Is Niacinamide Effective Without Sunscreen?
Niacinamide provides internal protection but does not replace sunscreen. Its effects are complementary, not redundant.
| Protection Method | What It Does |
| Sunscreen (SPF 30+) | Blocks or absorbs UV radiation at the skin surface |
| Niacinamide (oral) | Enhances DNA repair and reduces inflammation internally |
For best protection against skin cancer, dermatologists recommend using both — niacinamide as a supplement and sunscreen as a barrier.
This dual approach is especially important for those with underlying risk factors, such as skin damage from immunosuppression, chronic UV exposure, or early signs of skin disease.
Summary: Should You Take Niacinamide?
Niacinamide has emerged as a promising preventive option for patients with a history of skin cancer. It supports DNA repair, reduces inflammation, and lowers the recurrence of nonmelanoma cancers — all with minimal side effects.
While not a cure or substitute for regular dermatological exams, niacinamide can be an accessible, affordable layer of protection when used correctly.
Its potential role in future preventive care is expanding, especially as research explores how it may intersect with immunotherapy, radiation recovery, and other supportive treatments for patients with complex cancer histories — including those experiencing skin complications from breast cancer metastasis.
FAQ: Niacinamide and Skin Cancer – 15 Key Questions Answered
1. Can niacinamide reverse existing skin cancer
No, niacinamide is not a treatment for active skin cancer. It may reduce the risk of new lesions and support skin repair, but it cannot eliminate existing cancer cells. Surgery, radiation, or topical treatments remain primary for confirmed cases.
2. Is it safe to take niacinamide long-term?
Yes, clinical studies have shown that 500 mg twice daily is safe for up to 12 months in adults. However, ongoing monitoring is important, especially for liver function in those taking other medications.
3. What is the difference between niacinamide and niacin?
Niacinamide is the non-flushing form of vitamin B3, preferred for skin health. Niacin (nicotinic acid) can cause flushing and is more commonly used for cholesterol management. They are not interchangeable in cancer prevention.
4. Can topical niacinamide help prevent skin cancer too?
Topical formulations support skin barrier repair and reduce pigmentation, but they do not show the same preventive cancer effects as oral niacinamide. Oral use is recommended for cancer-related protocols.
5. Are there side effects of niacinamide in elderly people?
Older adults generally tolerate niacinamide well, but some may experience mild nausea or stomach discomfort. Dividing the dose or taking it with food can help reduce side effects.
6. Is niacinamide helpful after Mohs surgery?
Yes, it may reduce the recurrence of nonmelanoma skin cancers post-surgery. Some dermatologists recommend starting niacinamide a few weeks after wound healing is complete.
7. Can pregnant women take niacinamide for skin cancer prevention?
There is limited data on high-dose niacinamide in pregnancy. While small amounts in prenatal vitamins are safe, doses above 35 mg daily should be avoided unless prescribed.
8. Will niacinamide lighten skin tone?
At cosmetic doses, topical niacinamide can reduce hyperpigmentation. Oral niacinamide’s effect on skin tone is not well established and is not a focus in cancer prevention.
9. Can children or teenagers use niacinamide for prevention?
Routine use in children or adolescents is not recommended for cancer prevention unless there’s a specific medical condition under physician supervision.
10. Does niacinamide work for melanoma prevention?
Most data supports its role in nonmelanoma skin cancers (BCC and SCC). Its effect on melanoma is still unclear, so it should not be relied upon for melanoma prevention alone.
11. What time of day is best to take niacinamide?
There’s no strict time, but taking it with meals — once in the morning and once in the evening — helps improve absorption and minimizes gastrointestinal effects.
12. Can niacinamide replace a skin cancer screening?
No. Annual full-body skin exams by a dermatologist remain the gold standard for early detection. Niacinamide is an adjunct, not a substitute for professional screening.
13. Are there foods high in niacinamide that can help naturally?
Yes. Foods like turkey, salmon, brown rice, and fortified cereals contain niacinamide or precursors, but therapeutic levels used in cancer prevention are typically higher than dietary intake.
14. Can niacinamide be used with retinoids or acne treatments?
Yes, niacinamide can reduce irritation associated with retinoids and is often combined in skincare routines. However, that’s a cosmetic use, unrelated to skin cancer.
15. Where can I learn more about skin cancer and vitamin B3?
Trusted sources include the American Academy of Dermatology and peer-reviewed journals. Discussing with a board-certified dermatologist is the most reliable path for personalized advice.












