Metaplastic Carcinoma: A Rare and Aggressive Breast Cancer Type
Foreword
Being diagnosed with any form of breast cancer is overwhelming, but when that diagnosis comes with the words “metaplastic carcinoma”, it can feel even more confusing and daunting. Metaplastic carcinoma is a rare and aggressive form of breast cancer that may not be as widely recognized, yet its impact can be profound. If you or a loved one is facing this diagnosis, it’s completely natural to feel unsure, frightened, or even isolated. But let me assure you, you are not alone.
This article aims to provide clarity and guidance during what can feel like an uncertain and challenging time. Metaplastic carcinoma may be rare, but it is treatable. Understanding this cancer and how it differs from other breast cancer types is the first step toward navigating your treatment options and ensuring you’re not just another diagnosis in a medical chart, but a person with a unique path forward.
Throughout this article, we’ll break down what metaplastic carcinoma is, how it differs from more common forms of breast cancer, what you might experience physically and emotionally, and what treatment options are available to you. We’ll also address what you can expect in terms of prognosis and survival rates, along with helpful guidance on coping with the emotional and psychological impact of a rare cancer diagnosis.
It’s important to remember that while metaplastic carcinoma can be aggressive, there are treatment options available, and new research is continuously changing the landscape of how we fight this cancer. Whether you’re learning about this condition for the first time, supporting a loved one, or navigating your own journey, this article will help you understand the steps ahead. You are taking control by seeking knowledge, and that is a powerful first step in your journey.
Let’s explore the details of metaplastic carcinoma — because knowledge, compassion, and informed decisions are the tools that will help you face this challenge with confidence and strength.
Part 1: What Is Metaplastic Carcinoma?
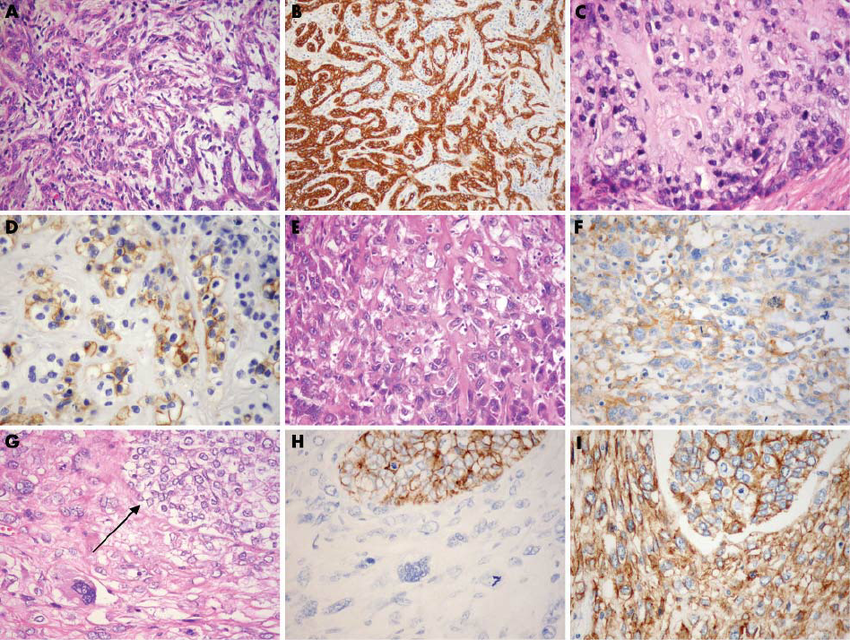
Metaplastic carcinoma is a rare and aggressive form of breast cancer that behaves differently from more common types. It is characterized by a mix of abnormal cells, which can include a combination of epithelial, mesenchymal, and sometimes even cartilage or bone tissue. This diversity of cell types makes metaplastic carcinoma distinct and more difficult to treat. Unlike typical breast cancer, which is mostly made up of ductal or lobular cells, metaplastic carcinoma’s cellular varietycan present challenges in both diagnosis and treatment.
Understanding Metaplastic Carcinoma
Metaplastic carcinoma is a form of breast cancer where the cancerous cells are significantly altered. These cells don’t look like normal breast tissue; instead, they take on characteristics from other types of tissues, like bone or cartilage, which is why it’s called “metaplastic.” The exact cause of this transformation is still being studied, but what is clear is that these cancers tend to grow more aggressively than other types and often spread faster.
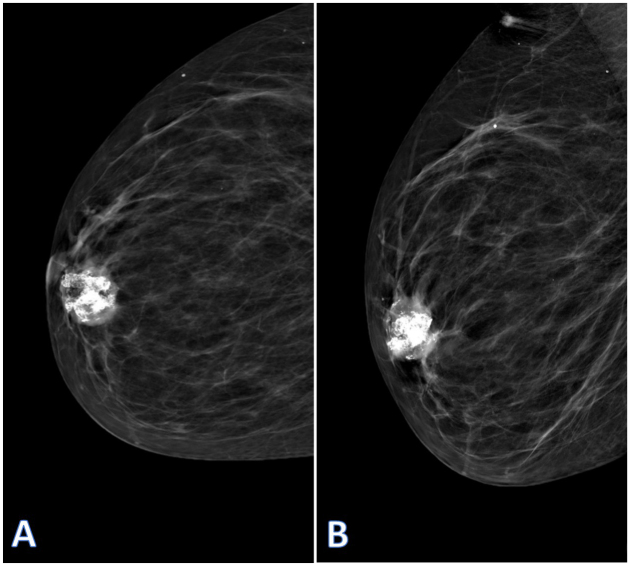
This type of cancer is typically diagnosed in later stages, as it may not form a distinct lump like more common breast cancers. Instead, the tumor can present as a firm, irregular mass or solid mass, which might not show up as clearly on early mammograms or ultrasounds. It’s also often confused with other types of tumors because of its unusual cell types.
The Various Types of Metaplastic Carcinoma
Metaplastic carcinoma is not a single disease but rather a group of related cancers that share some common features. Within this group, you’ll find several subtypes, each behaving differently in terms of treatment response and aggressiveness.
One of the subtypes is spindle cell carcinoma, where the cancerous cells take on a spindle-shaped appearance. This subtype is often one of the more aggressive forms of metaplastic carcinoma, resembling sarcoma (a cancer of the connective tissue) in its behavior. Another common subtype is squamous cell carcinoma, in which the cancer cells are flattened and resemble skin cells. These types are harder to treat than more typical forms of breast cancer because they don’t respond well to hormonal therapies or HER2-targeted treatments, which are effective in other types of breast cancer.
Then there is adenosquamous carcinoma, which is a combination of glandular and squamous cells. It’s a less common subtype, but its treatment and prognosis can vary significantly depending on its presentation and stage at diagnosis.
The Aggressive Nature of Metaplastic Carcinoma
What sets metaplastic carcinoma apart is its aggressive nature. Because it is made up of different cell types, it can be harder to treat with the standard therapies that are effective for other breast cancers. For example, hormonal treatments that target estrogen or progesterone receptors typically aren’t effective in metaplastic carcinoma, nor are therapies targeting HER2, since the cancer cells do not express these common breast cancer markers.
Moreover, metaplastic carcinoma tends to grow quickly and can spread to surrounding tissues or distant organs faster than typical breast cancer. This rapid growth and tendency to metastasize lead to a worse prognosis, especially if it is not diagnosed early.
Despite the challenges, there is hope, as ongoing research into personalized treatment plans and targeted therapies is opening new doors for patients diagnosed with this rare form of breast cancer. With the right treatment, it is still possible to manage symptoms, extend survival, and improve the quality of life.
Part 2: Symptoms of Metaplastic Carcinoma
Metaplastic carcinoma presents with a range of symptoms, some of which are common to other types of breast cancer, while others are more specific to its rare and aggressive nature. Early detection can be tricky, especially since the tumor doesn’t always manifest with the usual signs seen in more typical breast cancers. In this section, we’ll explore the symptoms that patients may experience, how they relate to the disease’s progression, and why prompt medical attention is crucial.
1. Physical Symptoms
Lumps and Masses
Like other types of breast cancer, metaplastic carcinoma often begins as a lump or mass in the breast. However, unlike the more well-defined, smooth, round lumps seen in many other breast cancer types, a metaplastic tumor may present as a firm, irregular mass that may feel hard or uneven. The shape and texture of the lump might make it difficult to differentiate from a benign growth or another form of cancer, leading to a delay in diagnosis.
Some patients may not notice a lump at all, especially in the early stages of the cancer when it might be too small or deep within the breast tissue to be detected through self-examination. This highlights the importance of regular screenings, especially for women at higher risk of breast cancer.
Pain and Swelling
Pain is another common symptom, though it’s not always present. The pain can range from mild discomfort to sharp, persistent sensations, often depending on the size and location of the tumor. The pain tends to be localized to the area around the tumor, and it may worsen as the tumor grows or presses against surrounding tissues. Swelling can occur around the tumor, leading to painful inflammation in the breast or the underarm area where lymph nodes might be affected.
In some cases, swelling can be significant enough to change the shape of the breast, making it appear more swollen or asymmetrical compared to the other side. This could be due to the tumor itself or the surrounding tissue reacting to the growing mass.
Skin Changes
As the tumor progresses, it may cause skin changes over the affected area. This includes redness, thickening, or even the appearance of dimpling on the skin of the breast. In more advanced cases, the skin may become ulcerated, leading to open wounds that can be painful and susceptible to infection. These changes are more common in advanced stages of metaplastic carcinoma, when the cancer has spread beyond the primary tumor site and started affecting surrounding tissues.
2. Psychological and Emotional Impact
Anxiety and Emotional Strain
Receiving a diagnosis of metaplastic carcinoma can be emotionally overwhelming, especially since it is a rare and aggressive form of breast cancer. The fear of the unknown, combined with the challenges of living with an uncommon cancer, can take a significant toll on a patient’s mental and emotional health.
Patients may experience feelings of anxiety, uncertainty, and even grief as they try to navigate a path forward. Questions about the future, treatment options, and the effectiveness of therapies are common, and it’s understandable for patients to feel a deep sense of worry about their prognosis. The psychological stress of having to manage both the physical symptoms and the emotional burden of a rare diagnosis can be overwhelming.
Impact on Body Image and Self-Esteem
The visible changes brought on by a metaplastic carcinoma, particularly in advanced stages, can have a major impact on a patient’s body image and self-esteem. As the tumor grows and changes the shape of the breast, some patients may feel self-conscious or ashamed of their appearance. This emotional strain can lead to social withdrawal, as patients may feel uncomfortable or embarrassed by the physical changes.
The pain and discomfort, coupled with the visible changes in the breast or skin, can also make it difficult to feel confident in one’s appearance. It’s important for patients to know that this is a natural reaction, and seeking help from a psychologist, oncology counselor, or support group can help navigate these feelings and regain a sense of self-worth.
3. Late-Stage Symptoms
In the later stages of metaplastic carcinoma, when the cancer has spread to other areas, more serious symptoms may develop. These can include:
- Breast or nipple discharge, which may be bloody or clear, depending on the nature of the tumor.
- Difficulty breathing or coughing up blood if the cancer has spread to the lungs.
- Pain in the bones, especially if the cancer has spread to the bones, leading to painful fractures or discomfort when moving.
At this stage, managing symptoms becomes a critical part of the treatment plan, with a strong focus on palliative care to improve the patient’s comfort and quality of life.
4. Challenges in Early Detection
One of the challenges in dealing with metaplastic carcinoma is that it often presents differently than more common forms of breast cancer. Its heterogeneous cellular makeup (with mixed types of cells) means it can sometimes evade detection in standard mammograms or ultrasounds. This makes early detection harder, and patients may not notice symptoms until the tumor is more advanced.
Patients at high risk of breast cancer or those with a family history should be diligent about regular screenings and seek medical attention if they notice any changes, even if they don’t experience the typical symptoms associated with more common forms of breast cancer.
Part 3: Treatment Options for Metaplastic Carcinoma
Metaplastic carcinoma can be a tough diagnosis to face, and you might be wondering, “What now?” The treatment for metaplastic carcinoma isn’t the same as it is for the more common types of breast cancer. Because of its rare and aggressive nature, metaplastic carcinoma doesn’t always respond to the standard treatments that work for other breast cancers. But that doesn’t mean there aren’t treatment options available. Let’s walk through the most common strategies you’ll encounter, and how they fit into the fight against this challenging cancer.
1. Surgical Treatment
If you’ve been diagnosed with metaplastic carcinoma, surgery is often the first treatment on the table. It’s usually the most effective way to remove the tumor and ensure you’re starting from the best possible position for the next steps in your treatment. There are a few different options depending on your specific situation.
Mastectomy
For many patients, a mastectomy (removal of the entire breast) is the recommended approach, especially if the tumor is large, locally advanced, or involves multiple areas of the breast. This can feel like a huge step, but it often provides the best opportunity to eliminate the cancer and prevent it from spreading.
While this procedure might feel overwhelming, keep in mind that breast reconstruction is available if you choose to go that route afterward. It’s also important to discuss your emotional needs with your care team — they can connect you with support resources to help with the mental toll of the surgery.
Lumpectomy
If the tumor is smaller and hasn’t spread extensively, a lumpectomy (removal of just the tumor) might be an option. However, metaplastic carcinoma is known for being more aggressive, and in some cases, lumpectomy may not be the best choice. Your healthcare provider will assess whether this is feasible based on the tumor’s size, location, and other factors.
After a lumpectomy, radiation therapy is usually recommended to ensure that any remaining cancer cells are eradicated, minimizing the risk of recurrence.
2. Chemotherapy
Here’s where things get a little different. Metaplastic carcinoma often resists traditional treatments, like hormone therapy or HER2-targeted therapies. This means that chemotherapy is the primary treatment option for most patients. It’s used to shrink the tumor, destroy cancer cells, and stop them from spreading.
Chemotherapy Regimens
Chemotherapy typically involves a combination of powerful drugs, including:
- Doxorubicin (often called Adriamycin)
- Cyclophosphamide
- Taxanes, like Paclitaxel or Docetaxel
- Carboplatin
These medications work by attacking rapidly dividing cells, which is what cancer cells do. But the drugs don’t just target cancer — they affect all rapidly dividing cells, which can lead to the side effects you’ve likely heard about, such as fatigue, nausea, and hair loss. Even though chemotherapy can be tough, it’s one of the best tools to manage aggressive cancers like metaplastic carcinoma.
3. Radiation Therapy
Following surgery, radiation therapy might be suggested. It uses high-energy rays to target and kill any remaining cancer cells that may have been missed during the surgery. If you’re dealing with advanced metaplastic carcinoma, radiation might also be used to shrink the tumor before surgery to make it easier to remove.
Radiation can also be an option if you experience pain, swelling, or other symptoms that affect your daily life. For instance, if the tumor is pressing on certain nerves or causing discomfort, radiation can help reduce the size and alleviate some of these challenges. It’s one of the key tools to make sure you’re as comfortable as possible throughout treatment.
4. Immunotherapy and Targeted Therapies
Now, this is where things are getting exciting. Because metaplastic carcinoma is so rare and aggressive, doctors are looking for new ways to treat it. Immunotherapy and targeted therapies are still being researched for this type of cancer, but they’re showing promise.
Immunotherapy
Immunotherapy helps your immune system recognize and fight cancer more effectively. Some drugs, like Pembrolizumab (Keytruda) and Atezolizumab (Tecentriq), are being used for certain types of breast cancer and might be available for metaplastic carcinoma patients through clinical trials. These drugs don’t directly attack the tumor; instead, they boost your body’s natural defenses to target cancer cells more efficiently.
Though not yet a standard treatment, immunotherapy is on the cutting edge of cancer treatment, and it holds promise for patients who may not respond well to chemotherapy or other traditional therapies.
Targeted Therapies
Targeted therapies are designed to target specific molecules or pathways that help cancer cells grow and survive. For instance, some patients with metaplastic carcinoma may benefit from PARP inhibitors or PI3K inhibitors, which are still being studied in clinical trials. These therapies are tailored to the specific mutations in cancer cells and can sometimes offer a more effective treatment with fewer side effects than standard chemotherapy.
While these therapies aren’t yet common practice for metaplastic carcinoma, the research is ongoing, and they’re part of a growing field of personalized medicine that could one day provide more effective treatment options.
5. Palliative Care
Palliative care is all about symptom management and improving quality of life. For advanced metaplastic carcinoma, this type of care can be incredibly valuable. The goal isn’t to cure the cancer, but to keep you as comfortable and pain-free as possible while managing other symptoms like fatigue, nausea, or emotional distress.
Palliative care includes:
- Pain management: Medications, nerve blocks, and other strategies to control pain.
- Nutritional support: Ensuring you get the nutrients you need during treatment.
- Psychological support: Helping you manage the emotional toll that cancer takes.
- Symptom relief: Offering ways to reduce discomfort and improve your overall well-being.
The goal is to provide you with the support you need to live as fully as possible during your treatment.
Part 4: Prognosis and Outlook
When diagnosed with metaplastic carcinoma, it’s natural to wonder what the outlook is and what to expect in terms of survival and quality of life. While it’s important to recognize that metaplastic carcinoma is considered a rare and aggressive form of breast cancer, many factors contribute to an individual’s prognosis. With advancements in treatmentand ongoing research, it’s possible to approach this diagnosis with a sense of hope, knowing that better outcomes are achievable with personalized care.
1. Survival Rates and Prognosis
As with any form of cancer, the prognosis for metaplastic carcinoma depends on several factors, including the stage of cancer at diagnosis, the size and location of the tumor, and how well the cancer responds to treatment.
Survival Rates
Metaplastic carcinoma generally has a lower survival rate than more common forms of breast cancer. However, the survival rates can vary depending on the stage at which the cancer is diagnosed and the patient’s response to treatment. Early-stage metaplastic carcinoma, when caught and treated early, offers a better chance for long-term survival.
However, metaplastic carcinoma is often diagnosed at a more advanced stage, which can make treatment more challenging. The 5-year survival rate for patients with early-stage breast cancer can range from 80% to 90% or higher, but for patients with advanced or metastatic metaplastic carcinoma, the survival rate drops significantly. The key to improving survival is early detection and aggressive treatment.
Factors That Impact Prognosis
Several factors influence the prognosis of metaplastic carcinoma:
- Tumor size and spread: Larger tumors and those that have spread to nearby lymph nodes or distant organs (such as the liver, lungs, or bones) often have a worse prognosis.
- Tumor grade: Metaplastic carcinoma tumors are typically high-grade (meaning the cells are poorly differentiated), which means they tend to grow faster and spread more quickly than low-grade tumors.
- Response to treatment: How well the cancer responds to treatment, particularly chemotherapy and radiation, plays a crucial role in prognosis. Metaplastic carcinoma can be chemoresistant, meaning it may not respond well to chemotherapy, but personalized approaches and clinical trials are offering new hope.
- Age and overall health: A person’s age and general health play a role in how well they tolerate treatments and recover from surgery. Younger, healthier patients tend to have better outcomes than older patients or those with underlying health issues.
2. Challenges in Treatment and Response
The challenge with metaplastic carcinoma lies in its resistance to standard therapies, such as hormonal therapy and HER2-targeted treatments. Unlike other types of breast cancer, which can be treated effectively with drugs that target estrogen receptors, progesterone receptors, or HER2 proteins, metaplastic carcinoma does not typically respond to these treatments.
This makes the cancer more difficult to treat and results in a higher rate of recurrence or metastasis. However, despite these challenges, chemotherapy remains the cornerstone of treatment, and radiation therapy can help improve quality of life for those dealing with larger tumors or pain.
New approaches like immunotherapy and targeted therapies offer hope for future treatments and may provide patients with better outcomes than traditional chemotherapy alone. The use of clinical trials is also an option for patients seeking innovative treatments that may not yet be widely available.
3. Improving Quality of Life
While the prognosis for metaplastic carcinoma can be serious, it’s important to focus on improving quality of lifethroughout the treatment journey. Palliative care plays a key role in managing symptoms such as pain, fatigue, and nausea, ensuring that patients feel supported both physically and emotionally.
Symptom Management
The use of pain relief medications, wound care, and radiation can help patients manage the symptoms associated with metaplastic carcinoma. Advances in palliative care are also helping to alleviate some of the more distressing side effects, including the odor from fungating tumors or nausea from chemotherapy. Emotional support from counselors or support groups is equally important in ensuring a positive mental outlook during treatment.
Social Support and Counseling
Facing an advanced cancer diagnosis can be isolating, but you don’t have to go through it alone. Social support from family, friends, and loved ones is vital to staying emotionally healthy. In addition, connecting with others who understand your journey through support groups or counseling can provide much-needed comfort and understanding. Emotional well-being is just as important as physical health, and seeking help is a sign of strength.
4. Hope for the Future
While metaplastic carcinoma presents unique challenges, research into breast cancer treatment is evolving rapidly. The future holds promise in terms of personalized medicine, immunotherapies, and targeted therapies that could significantly improve outcomes for patients with this rare and aggressive cancer.
Ongoing studies and clinical trials are exploring how genetic profiling and biomarker testing can be used to tailor treatments to an individual’s specific cancer characteristics, offering a more effective and less invasive approach to managing the disease.
Part 5: FAQs About Metaplastic Carcinoma
When dealing with a rare and aggressive cancer like metaplastic carcinoma, many questions naturally arise. It’s essential to address these concerns head-on to ensure that you feel informed and empowered. Below are some of the most frequently asked questions about metaplastic carcinoma, covering everything from diagnosis to treatment options, prognosis, and emotional well-being.
1. What makes metaplastic carcinoma different from other types of breast cancer?
Metaplastic carcinoma is unique because it is made up of different cell types. While most breast cancers consist of cells that resemble the tissues of the breast, metaplastic carcinoma includes a mixture of epithelial cells (like those found in the ducts), mesenchymal cells (like those found in connective tissues), and sometimes even cartilage or bone. This makes it harder to treat because it doesn’t respond to the typical hormonal therapies or HER2-targeted treatments that are effective for other breast cancers. It also tends to grow faster and spread more aggressively.
2. Is metaplastic carcinoma hereditary?
While genetic factors can influence the development of any form of breast cancer, metaplastic carcinoma is not typically classified as a hereditary cancer. That said, genetic mutations, such as those found in the BRCA1 or BRCA2 genes, can increase the risk of developing breast cancer in general, including metaplastic carcinoma. If you have a family history of breast cancer or genetic mutations, it’s important to discuss your risk with a genetic counselor or your doctor to determine the best approach for screening and prevention.
3. Can metaplastic carcinoma be treated with hormonal therapy?
No, unfortunately, hormonal therapy is not typically effective for metaplastic carcinoma. Unlike other breast cancer types that are hormone receptor-positive, meaning they respond to treatments that block estrogen or progesterone, metaplastic carcinoma tends to be hormone receptor-negative. This means that therapies like tamoxifen or aromatase inhibitors, which are commonly used to treat hormone-sensitive cancers, usually don’t work for this type of cancer. Instead, chemotherapy remains the primary treatment for metaplastic carcinoma.
4. What are the survival rates for patients with metaplastic carcinoma?
Survival rates for metaplastic carcinoma can vary widely depending on factors like the stage at diagnosis, the size and location of the tumor, and how the cancer responds to treatment. In general, because metaplastic carcinoma is an aggressive and often chemoresistant cancer, the survival rates tend to be lower compared to more common forms of breast cancer. However, early detection and effective treatment can improve the prognosis. It’s important to remember that survival rates are just statistics, and individual experiences can differ greatly depending on personal health, treatment response, and other factors.
5. Are there any clinical trials for metaplastic carcinoma?
Yes, there are ongoing clinical trials exploring new treatments for metaplastic carcinoma. Researchers are studying immunotherapies, targeted therapies, and personalized medicine approaches to determine if they can improve outcomes for patients with this rare and difficult-to-treat cancer. If you’re interested in participating in a clinical trial, talk to your oncologist about whether one is available to you. Clinical trials can offer access to cutting-edge treatments that aren’t yet widely available and may provide additional treatment options.
6. What is the role of immunotherapy in treating metaplastic carcinoma?
Immunotherapy is an emerging treatment option for many types of cancer, including metaplastic carcinoma. Since this cancer is often resistant to traditional treatments, immunotherapy offers a potential way to help the immune systembetter recognize and attack cancer cells. Drugs like Pembrolizumab (Keytruda) and Atezolizumab (Tecentriq) have shown promise in some cases of breast cancer, and they are being tested for their efficacy in treating metaplastic carcinoma. Although immunotherapy isn’t yet standard for this cancer type, it’s an exciting area of research that could change the treatment landscape in the future.
7. What should I expect during treatment for metaplastic carcinoma?
Treatment for metaplastic carcinoma typically involves chemotherapy, surgery, and possibly radiation therapy. Depending on the stage of the cancer, treatment may be aimed at shrinking the tumor, removing it through surgery, or reducing symptoms for more advanced stages. Many patients also require palliative care to manage symptoms like pain, fatigue, and nausea. Because metaplastic carcinoma doesn’t respond to typical breast cancer therapies, you can expect a more personalized treatment plan. Your oncologist will work with you to determine the best course of action based on your unique situation.
8. Can metaplastic carcinoma be prevented?
Unfortunately, there is no known prevention for metaplastic carcinoma specifically. However, there are steps you can take to lower your risk of developing breast cancer in general. These include maintaining a healthy lifestyle, regular exercise, limiting alcohol consumption, and considering genetic counseling if you have a family history of breast cancer or other risk factors. Regular screenings, such as mammograms and breast exams, are also essential for early detection. If you have concerns or a family history of breast cancer, discuss them with your healthcare provider to ensure you’re taking the right steps for early detection.
Part 6: Final Thoughts
Receiving a diagnosis of metaplastic carcinoma is undoubtedly difficult, but it’s important to remember that you are not powerless in the face of this rare and aggressive cancer. Knowledge is one of the most powerful tools you have as you navigate your treatment journey. By understanding the unique characteristics of metaplastic carcinoma, you can take proactive steps in managing your health, making informed decisions about your treatment options, and finding supportto help you through the process.
Although this cancer type is known for its resistance to standard treatments and its aggressive nature, there is hope. The field of cancer research is constantly advancing, and personalized medicine is opening new doors for better, more effective treatments. Immunotherapy, targeted therapies, and clinical trials are all offering new possibilities that weren’t available even a few years ago. While we still have a long way to go in fully understanding how to treat metaplastic carcinoma, the progress being made is encouraging.
Through chemotherapy, surgery, radiation, and palliative care, patients have access to a range of options aimed at controlling symptoms and improving their quality of life. With the right care and support, it’s possible to manage the disease and live a meaningful, fulfilling life even in the face of a difficult diagnosis.
Never forget the importance of emotional support. Whether through support groups, counseling, or just talking to a loved one, dealing with the emotional toll of cancer is just as critical as managing the physical aspects. Your mental health is an essential part of your overall well-being, and reaching out for help is not a sign of weakness, but a sign of strength.
No matter where you are in your journey, remember this: you are not defined by your diagnosis. The path ahead might seem uncertain at times, but you have the power to take control of your treatment plan, advocate for your health, and build the support system you need to thrive.
You’ve already taken a huge step by seeking out information about your diagnosis, and that’s something to be proud of. Keep asking questions, stay informed, and continue working closely with your healthcare team. The more you know, the better equipped you’ll be to handle whatever comes next.









