The Metabolic Approach to Cancer: A Guide to Terrain-Based Healing
- Foreword
- 1. Introduction to Cancer Metabolism
- 2. Core Principles of the Metabolic Approach
- 3. Deep Dive into the Ten Elements
- From Framework to Function
- 4. Nutritional Strategies
- 5. Integrative Therapies
- 6. Case Studies and Testimonials
- 7. Comparing Conventional and Metabolic Approaches
- 8. Future Directions in Cancer Metabolism
- 9. Frequently Asked Questions (FAQs)
- Closing Thought
Foreword
What if everything you thought you knew about cancer was only part of the picture?
It’s a question worth asking—not because conventional oncology is irrelevant or misguided, but because the war on cancer has, for all its weapons, yielded too many casualties. Despite multi-billion-dollar research campaigns, revolutionary drugs, and powerful imaging technologies, cancer continues to evade, recur, and kill. Patients often emerge from treatment burned out and bewildered, handed a “clean scan” yet offered no roadmap to staying well. Why does this happen? What are we missing?
That’s where the metabolic approach enters the conversation—and perhaps redefines it altogether.
Rooted in systems biology and revived from some of the earliest 20th-century hypotheses about cancer’s origins, this approach invites us to stop viewing tumors as foreign invaders to be eliminated at all costs and instead to ask: What conditions within the body allowed these cells to thrive in the first place? What if cancer isn’t just a genetic disease, but a metabolic one—one that takes root in a terrain we might be able to change?
This article is your final stop for understanding that possibility. Whether you’ve read The Metabolic Approach to Cancerby Dr. Nasha Winters and Jess Higgins Kelley, are curious about the science behind metabolic therapies, or are just looking for a comprehensive breakdown of this integrative model, you’re in the right place. We’re going to break it all down—its origins, its logic, its pillars, and yes, its limitations.
You’re not just a passive reader here. This is your health, your mind, your body—your terrain. And you deserve to understand how it works.
Introduction to Cancer Metabolism
Cancer. Even the word has gravity. For over a century, it’s been at the center of some of the most intense medical research, with billions invested and innumerable lives touched. The prevailing view—reinforced through textbooks, white coats, and treatment protocols—is that cancer is, fundamentally, a genetic disease. DNA mutates, cells divide out of control, and tumors emerge as a result. That narrative has shaped not just public understanding, but also the core of oncology: cut, burn, poison—the triumvirate of surgery, radiation, and chemotherapy.
But what if there’s more to the story?
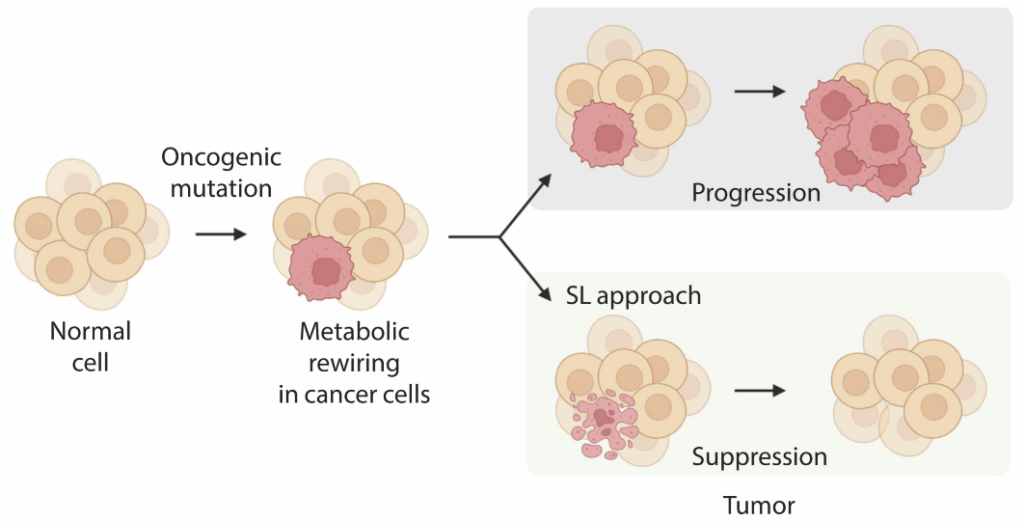
A growing chorus of researchers, clinicians, and survivors is asking us to reconsider the roots of cancer—not to reject the genetic model entirely, but to expand it. They’re suggesting we look not just at what went wrong inside a single cell, but at the broader environment—the internal “soil” in which that cell took root and grew. In this model, cancer is not simply a malfunctioning cell; it’s a disease of context. The question shifts from “What mutation caused this?” to “What conditions allowed this?”
This perspective isn’t new. In fact, one of the earliest and most significant insights into cancer’s unique metabolism came nearly a century ago from Otto Warburg, a German physiologist who won the Nobel Prize in 1931. Warburg observed that cancer cells consume glucose at an abnormally high rate, even when oxygen is plentiful. Instead of using efficient, oxygen-driven pathways to produce energy, they ferment glucose into lactate—a primitive and inefficient process. This preference for glycolysis in the presence of oxygen became known as the Warburg effect, and for decades, it was a scientific curiosity. Interesting, yes. Clinically useful? Not yet.
Fast forward to the 21st century. The genetic model has become dominant. We’ve mapped cancer genomes, identified driver mutations, and developed targeted drugs that aim to block malfunctioning receptors or signaling cascades. Yet, perplexingly, many tumors share common behaviors—metabolic ones—regardless of their genetic profile. And patients with the same mutation may experience vastly different outcomes. One might go into remission, another relapses. Why? Why do tumors so consistently demonstrate metabolic similarities, regardless of their origin or mutation load?
These questions have led to a resurgence of interest in cancer metabolism—not as a relic of pre-genomic thinking, but as a dynamic lens that may explain what genetics alone cannot. The metabolic model suggests that a tumor’s ability to grow is intricately tied to the bioenergetic state of the body. It’s about fuel availability, mitochondrial dysfunction, inflammation, and immune evasion. And when these systems are unbalanced, cancer not only emerges—it finds a fertile environment in which to thrive.
This doesn’t mean genes don’t matter. It means they don’t act alone. Genes may load the gun, as the saying goes, but the environment pulls the trigger. And metabolism is the medium in which that environment operates. A person’s diet, sleep rhythms, exposure to toxins, stress levels, microbial health, and glycemic control—these all feed into the metabolic terrain. It’s the ecosystem that governs cellular behavior.
And yet, this terrain—the body’s deep, dynamic background—has been largely ignored in mainstream oncology. The focus has stayed on the tumor itself, as if it exists in a vacuum. But tumors are not isolated islands. They are fed by blood, shaped by hormones, influenced by immune signals, and sustained—or undermined—by the metabolic state of the host.
The metabolic approach doesn’t reject conventional treatment. It reframes the goal. Instead of merely killing cancer cells, it asks: what happens next? If chemotherapy works, what terrain remains for your body to rebuild on? If surgery removes the tumor, what conditions allowed it to appear in the first place—and are those still present? These aren’t theoretical questions. They’re central to recurrence, remission, and long-term survival.
In short, this isn’t about abandoning one model in favor of another. It’s about integration. A tumor-centric approach can reduce tumor load. A terrain-centric approach may prevent its return. And the metabolic model offers something that is often missing from conventional oncology: a way to understand and influence the environment in which healing—or disease—takes place.
Once you start to see cancer as a metabolic disease, as well as a genetic one, everything changes. The patient is no longer a passive recipient of treatment but an active participant in shaping the conditions that influence outcome. From what they eat, to how they sleep, to how they manage stress and support detoxification—all of these become therapeutic tools.
That is the promise of the metabolic model. Not certainty. Not perfection. But agency. A return to the idea that biology is not fate, and that healing is not just a matter of targeting disease, but cultivating health.
Thinking beyond conventional oncology? A useful contrast can be drawn with dense dose chemotherapy, which takes the opposite — ultra-interventionist — route.
And so, if we agree that the terrain matters—and that it can be changed—the next logical step is to define its core elements. What exactly makes up this internal ecosystem? How do we assess it, support it, and shift it toward resilience? That’s where we go next.
The Book That Shaped the Movement
Much of what we’ve explored so far—the emphasis on terrain, the ten foundational elements, the integration of nutrition, lifestyle, and biology—draws inspiration from The Metabolic Approach to Cancer, co-authored by Dr. Nasha Winters and Jess Higgins Kelley. More than a guide, the book is a synthesis of decades of clinical experience, scientific insight, and lived wisdom. It presents the “Optimal Terrain Ten Protocol” as a personalized roadmap for restoring balance, strengthening immunity, and shifting the body’s internal conditions away from cancer-promoting patterns.
What makes the book uniquely impactful is its focus on empowerment. Rather than proposing a one-size-fits-all protocol, it encourages readers to assess their own metabolic terrain—glucose control, immune function, toxic exposures, circadian rhythms, emotional stress—and then make targeted, sustainable changes. The authors emphasize that cancer isn’t just a local problem to be surgically removed or chemically suppressed; it’s a systemic response to internal imbalance.
The book also introduces therapeutic tools such as the ketogenic diet, mistletoe therapy, detoxification, and mitochondrial support—not as “alternatives” to conventional care, but as deeply integrative strategies. These tools are woven into real case studies and practical guidance, helping readers understand not just what to do, but why it matters biologically.
For many patients and practitioners, this book has become the cornerstone of a more thoughtful, terrain-based oncology—one that respects both the science of tumors and the wisdom of systems.
Deep Dive into the Ten Elements
Epigenetics: Updating the Code Without Changing the Genes
Epigenetics is the art of cellular storytelling—the way your genes are expressed based not just on heredity, but on experience. You may carry a gene that predisposes you to cancer, but whether or not that gene is “turned on” is shaped by how your body receives and processes environmental signals. This includes everything from nutrient intake and stress to sleep, toxin exposure, and even emotional trauma. Unlike the genome, which is largely fixed, the epigenome is fluid, dynamic, and deeply responsive to the terrain you create through your choices and surroundings.
| Terrain Element | Focus Area | Why It Matters |
|---|---|---|
| Epigenetics | Gene expression regulation | Modulates tumor suppressors and oncogenes; links lifestyle to cellular behavior |
| Blood Sugar Balance | Glycemic control | Reduces insulin and IGF-1 driven tumor growth; stabilizes metabolic signaling |
| Immune Function | Immune surveillance | Enables detection and elimination of abnormal cells before tumors develop |
| Inflammation | Chronic and acute inflammatory load | Chronic inflammation promotes DNA damage, angiogenesis, and immune suppression |
| Detoxification | Liver, kidneys, lymph, skin | Supports removal of carcinogens, hormone metabolites, and therapy byproducts |
| Hormone Balance | Estrogen, insulin, cortisol, etc. | Hormonal imbalances can fuel hormonally driven cancers and weaken immunity |
| Microbiome Health | Gut bacteria and diversity | A healthy microbiome regulates immunity, nutrient absorption, and detoxification |
| Circadian Rhythm | Sleep-wake cycles and melatonin | Disruption impairs DNA repair, increases cortisol, and reduces melatonin |
| Mental/Emotional Health | Stress, trauma, belief systems | Chronic stress alters immunity, inflammation, and metabolic tone |
| Oxygenation | Mitochondrial efficiency and breath | Poor oxygenation promotes anaerobic metabolism, favoring cancer cell survival |
Assessing epigenetic resilience often involves looking at methylation patterns, detox pathways, and nutrient status, especially around folate, B12, and other methyl donors. This isn’t about fearfully decoding your DNA, but rather learning how to communicate with your genes—through food, light, movement, and mindset—in ways that encourage healing and cellular harmony.
Glycemic Control: Lowering the Fuel Supply Strategically
Cancer cells love sugar. That’s not a metaphor; it’s a metabolic fact. They rely heavily on glucose for energy and, in many cases, lack the metabolic flexibility to use other fuels like fat or ketones. This makes glycemic control a cornerstone of the metabolic approach—not as a diet trend, but as a strategic method to alter the tumor’s environment.
Monitoring fasting insulin, glucose, and real-time responses through continuous glucose monitors (CGMs) allows patients and clinicians to see how the body is handling sugar—often revealing hidden patterns of instability even in people without diabetes. Reducing glycemic variability isn’t just about diet. It’s about stabilizing the entire endocrine and metabolic signaling network. And for many cancer patients, it’s a form of metabolic therapy in its own right.
Toxic Burden: Mapping the Hidden Load
Most people carry a toxic burden they can’t see or feel—until it begins to disrupt metabolism, immune function, and cellular communication. We live amidst a silent sea of industrial chemicals, heavy metals, plasticizers, pesticides, and hormone disruptors, and while the body has systems in place to eliminate these substances, it can become overwhelmed.
Functional testing can identify key exposures, while terrain-informed strategies—like sauna therapy, liver support, binding agents, and lymphatic activation—can help lighten the body’s chemical load. Detoxification here isn’t a marketing gimmick; it’s a biological necessity. The key is individualization: supporting detox capacity without draining reserves.
Circadian Rhythm: Resynchronizing with Biology
When we think of health, time isn’t always the first dimension that comes to mind. But it should be. Every cell in the body follows a circadian rhythm, orchestrated by light, temperature, food timing, and sleep. Cancer thrives when this rhythm is disturbed. Disrupted sleep-wake cycles alter hormone secretion, immune surveillance, and even gene repair—all processes that directly influence cancer risk and recovery.
Getting back in rhythm doesn’t require a monastic lifestyle. It starts with practical shifts: minimizing blue light exposure at night, getting natural sunlight in the morning, aligning eating windows with daylight hours, and honoring a consistent sleep schedule. These seemingly simple behaviors recalibrate complex systems.
Hormonal Balance: Regaining Internal Signal Clarity
Hormones are the messengers of metabolism. When they’re in balance, your body speaks in whispers. When they’re out of balance, it shouts—and sometimes loses the ability to communicate altogether. In the context of cancer, hormonal imbalance can drive proliferation (as with estrogen dominance), suppress immune vigilance (as with chronic cortisol elevation), or create chaotic feedback loops that mask deeper dysfunction.
Thorough hormone testing—looking not just at levels but at metabolites, ratios, and rhythms—can reveal patterns that conventional screens miss. The terrain approach often includes botanical and lifestyle strategies to correct imbalances before pharmaceutical intervention becomes necessary, aiming to restore signal clarity at the root.
Immune Function: Rebuilding the Internal Army
Your immune system is your first—and last—line of defense against cancer. It’s constantly patrolling, tagging aberrant cells, deploying inflammatory messengers, and orchestrating healing. But a terrain weakened by chronic inflammation, poor nutrition, stress, or gut dysbiosis can blunt immune responses or turn them against the body itself.
Testing immune competence through markers like NK cell activity, immunoglobulin levels, cytokine profiles, and vitamin D status helps gauge readiness. Supporting the immune system means more than popping supplements. It means tending to the inputs that nourish its regulatory balance: gut health, sleep, microbial diversity, and psycho-emotional peace.
Inflammation: Cooling the Chronic Fire
Inflammation is often seen as a villain, but it’s really a responder—one that’s meant to be sharp, precise, and temporary. The problem isn’t inflammation itself, but the failure to resolve it. When the body’s inflammatory pathways get stuck in a low-grade, simmering state, they feed the cancer terrain—encouraging angiogenesis, DNA damage, and immune suppression.
Reducing this chronic fire starts with understanding the source. It could be an imbalanced microbiome, untreated infection, unresolved trauma, or even dietary patterns high in omega-6 fats and refined carbohydrates. Anti-inflammatory protocols aren’t about silencing the fire alarm; they’re about putting out the fire and fixing the faulty wiring that keeps triggering it.
Angiogenesis: Cutting the Cancer Supply Lines
Once a tumor grows past a certain size, it needs its own blood supply to continue expanding. This process—angiogenesis—is how cancer secures its survival. Targeting this mechanism doesn’t just slow growth; it can starve the tumor of essential nutrients and oxygen.
While pharmaceutical angiogenesis inhibitors exist, the terrain approach leans into nature’s pharmacy: compounds in foods like turmeric, green tea, berries, and garlic have been shown to regulate angiogenesis gently, without the side effects of more aggressive agents. The goal isn’t to block blood vessels across the board, but to create a vascular environment that favors healthy tissue over malignant ones.
Microbiome: Cultivating a Cancer-Resistant Ecosystem
We’re beginning to understand that our gut microbiota function almost like an endocrine organ—producing hormones, modulating the immune system, influencing inflammation, and affecting how we metabolize nutrients and even drugs. When this microbial community is out of balance, it doesn’t just lead to digestive issues—it reshapes the terrain in ways that can promote or protect against cancer.
Restoring microbial balance means moving beyond simplistic probiotic fixes. It requires feeding beneficial bacteria with fiber, polyphenols, and prebiotics; removing pathogens and overgrowths; and restoring mucosal immunity. Personalized stool testing helps tailor the process, making microbiome support a central pillar of metabolic cancer care.
Mental and Emotional Health: The Terrain of Experience
No terrain can be fully assessed without touching the invisible forces of belief, emotion, memory, and meaning. Chronic stress, unresolved grief, and emotional suppression don’t just weigh on the mind—they alter biology. They elevate cortisol, shrink telomeres, increase gut permeability, and modulate immune signaling in ways that subtly but powerfully shape the terrain.
This isn’t about “positive thinking” or bypassing pain. It’s about honoring the body-mind connection as a real and potent influence on health. Healing may involve therapy, mindfulness, body-based trauma work, or simply finding ways to feel safe again. Whatever the modality, the goal is integration: to bring coherence back to a system that’s fragmented by fear or pain.
Each of these ten terrain elements is a gateway. Not every patient will need to focus equally on all ten at once, and the metabolic approach doesn’t demand perfection. It demands attention—to patterns, to causes, to interconnected systems that speak a language of balance or distress.
The terrain-based model also intersects with lifestyle factors, and some theories have been explored in pieces like Can Rebounding Spread Cancer?.
The more fluently we learn to read that language, the more precisely we can act—not with one-size-fits-all solutions, but with terrain-aware interventions that move the body toward healing. And there’s no better place to begin that intervention than with the most foundational metabolic input of all: nutrition.
That’s where we’ll turn next.
Nutritional Strategies
If there’s one aspect of health that every patient feels empowered to engage with, it’s food. We eat daily. We make choices about what to put in our bodies. But when it comes to cancer, nutrition is no longer just about general wellness—it becomes therapeutic. Within the metabolic approach, nutrition is not a backdrop; it’s a central strategy. Yet this isn’t about following a trendy plan or obsessively cutting carbs. It’s about understanding what your food is doing at a metabolic level—and how that impacts your terrain.
| Dietary Strategy | Metabolic Target | Terrain Benefit |
|---|---|---|
| Ketogenic Diet | Glucose restriction | Starves glycolytic tumor cells |
| Intermittent Fasting | Insulin modulation | Enhances autophagy, reduces inflammation |
| Mediterranean Diet | Anti-inflammatory phytochemicals | Supports microbiome, lowers oxidative stress |
Why Nutrition Matters in Cancer Metabolism
Food isn’t just fuel. It’s information. Every bite you take delivers biochemical instructions: to raise or lower inflammation, to activate or silence genes, to spike or stabilize insulin. And when it comes to cancer, many of these messages matter far more than calories or macronutrient ratios.
Metabolic nutrition aims to create an internal environment where cancer cells struggle to thrive, while healthy cells are supported and nourished. This is about shifting the terrain in real, measurable ways—lowering insulin, reducing oxidative stress, promoting mitochondrial function, and modulating immune activity.
The Strategic Role of Ketogenic Nutrition
One of the most studied nutritional strategies in metabolic oncology is the ketogenic diet—a high-fat, low-carbohydrate approach that shifts the body’s primary fuel source from glucose to ketones. This is especially relevant given what we know about the Warburg effect: many cancer cells are heavily dependent on glucose and exhibit a diminished ability to metabolize ketones.

The goal of a therapeutic ketogenic diet isn’t weight loss or lifestyle branding. It’s metabolic intervention. By reducing glucose availability and insulin signaling, this dietary approach puts cancer cells under pressure—while providing healthy tissues with an alternative fuel that may actually protect them from treatment-induced damage.
However, ketosis isn’t universally appropriate. It’s not for every cancer type, nor for every patient. Cachexia, adrenal fatigue, thyroid dysfunction, and certain treatment contexts may require modified or cyclical approaches. This is where terrain testing becomes essential—tracking blood glucose, ketones, insulin, and inflammatory markers to personalize the protocol.
Fasting and Time-Restricted Eating
Fasting may be one of the oldest healing practices known to humanity, but modern science is rapidly catching up to its power. Intermittent fasting, extended fasts, and time-restricted feeding (e.g. eating within a 10-hour daylight window) are increasingly studied for their ability to induce autophagy, regulate insulin sensitivity, and reduce systemic inflammation—all of which impact the cancer terrain.
In some cancer protocols, fasting is used around chemotherapy to reduce side effects and protect healthy cells, a concept known as differential stress resistance. In others, time-restricted eating is a daily rhythm that reinforces circadian biology and stabilizes metabolic signals.
That said, fasting isn’t a universal tool. In patients who are underweight, nutritionally depleted, or metabolically fragile, fasting can backfire. As with all aspects of the metabolic model, context is everything.
Food as Signaling Molecule: The Power of Phytonutrients
While macro-level decisions about fats, carbs, and protein get the most attention, the metabolic model places equal—if not greater—emphasis on micronutrients and phytochemicals. These compounds, found in richly pigmented vegetables, herbs, and spices, have profound metabolic effects. They can downregulate inflammatory genes, inhibit angiogenesis, support detoxification, and enhance mitochondrial function.
Cruciferous vegetables, for example, provide sulforaphane—a potent epigenetic regulator. Green tea offers EGCG, which can reduce oxidative stress and inhibit tumor growth pathways. Berries, turmeric, pomegranate, garlic—these are not garnish in this model. They’re molecular messengers.
Building a phytonutrient-dense diet doesn’t mean eliminating all animal foods, nor does it mean raw salads three times a day. It means color, variety, and diversity—with meals that deliver not just sustenance, but terrain-altering information.
Metabolic Flexibility Over Dietary Dogma
One of the traps in any therapeutic nutrition model is rigidity. The metabolic approach warns against this. The goal isn’t perpetual ketosis or eternal carb restriction. The goal is flexibility: to be able to switch efficiently between fuel sources, respond to environmental and internal cues, and adapt dietary inputs based on terrain shifts.
Some patients may thrive on low-carb protocols for months or years; others may benefit from targeted carbohydrate reintroduction to support thyroid or adrenal function. There is no one-size-fits-all answer here. What matters is metabolic resilience—your body’s capacity to respond intelligently to its needs.
Tools like CGMs, ketone meters, food logs, and symptom tracking allow for informed adjustments rather than blind adherence. This isn’t about diet rules. It’s about metabolic literacy.
Protein: A Double-Edged Sword
Protein occupies a nuanced place in the metabolic terrain. On one hand, it supports muscle mass, tissue repair, and immune resilience—all vital during and after cancer treatment. On the other, certain amino acids, when overconsumed or poorly metabolized, can activate pathways like IGF-1 that may promote tumor growth under specific conditions.
Again, context matters. For someone in a cachectic state, insufficient protein is a far greater risk than IGF signaling. For someone in remission, managing protein quality and quantity becomes a way of keeping metabolic signals in check. The type of protein also matters—grass-fed meats, collagen-rich bone broth, fermented legumes, and wild-caught fish support the terrain far more constructively than processed meats or synthetic isolates.
Supplements: Support, Not Substitution
Supplements in the metabolic model serve to fine-tune—not to override poor foundations. A supplement may support a specific pathway (say, curcumin for inflammation, berberine for glucose control, or PQQ for mitochondrial biogenesis), but it won’t correct a terrain shaped by chronic stress, poor sleep, and a processed diet.
That said, in the hands of skilled practitioners, supplements can be powerful. Especially during treatment recovery or terrain rebuilding phases, they can bridge gaps and accelerate healing. What’s essential is precision: testing before guessing, understanding interactions, and adjusting as the terrain changes.
Food Patterns Disguised as “Healthy”
One of the more eye-opening aspects of metabolic nutrition is discovering how many people believe they are eating healthfully—while inadvertently feeding the cancer terrain. Frequent snacking, “clean” packaged foods, sugar-laden smoothies, and overreliance on fruit can all spike insulin and blood sugar despite their natural branding.
This isn’t about guilt—it’s about clarity. Metabolic nutrition asks not just what you’re eating, but how your body is responding. One person’s salad might lower inflammation. Another’s might trigger bloating and fatigue due to oxalate sensitivity or poor digestion. Data and dialogue—between patient, practitioner, and body—are the way forward.
Integrative Therapies
While nutrition is the most foundational tool in the metabolic approach to cancer, it is far from the only one. Food changes the terrain, yes—but cancer is a complex, adaptive disease, and terrain restoration often requires more than dietary intervention. This is where integrative therapies come into play—not as fringe alternatives, but as scientifically grounded, biologically supportive tools that can complement and enhance the healing process.
What distinguishes these therapies is their non-toxic nature and their focus on bolstering the body’s innate capacity for regulation, detoxification, and resilience. They are neither substitutes for conventional oncology nor placebos to make patients feel proactive. Done right, they are evidence-informed adjuncts that support recovery, reduce side effects, and help shift the internal environment in ways that may profoundly influence outcomes.
Hyperbaric Oxygen Therapy (HBOT)
Oxygen is life. But cancer, paradoxically, often thrives in low-oxygen environments. Tumors frequently contain hypoxic regions—areas where blood flow is poor and oxygen levels drop. These pockets of low oxygen not only support tumor growth and metastasis but can also make cancers more resistant to radiation and chemotherapy.
Hyperbaric oxygen therapy addresses this directly. By delivering oxygen under pressure in a specialized chamber, HBOT saturates the body’s tissues—including those poorly perfused tumor regions—with oxygen. This can inhibit cancer’s metabolic advantage while simultaneously improving wound healing, tissue regeneration, and post-treatment recovery. In integrative protocols, HBOT is often paired strategically with other interventions, especially for patients undergoing radiation or recovering from surgery.
Intravenous Vitamin C
At standard doses, vitamin C acts as an antioxidant. But at high intravenous concentrations, it shifts roles and becomes a pro-oxidant—a paradoxical move that cancer cells are poorly equipped to handle. In this form, vitamin C generates hydrogen peroxide in tissues, selectively damaging cancer cells while sparing healthy ones.
Research into IV vitamin C has shown it may enhance quality of life, reduce treatment-related side effects, and even boost the effectiveness of certain chemotherapies. It’s not about replacing chemo with vitamins—it’s about intelligently pairing therapies that work on different levels of the terrain. By improving mitochondrial function, modulating immune responses, and supporting detox pathways, high-dose vitamin C becomes a multipurpose terrain enhancer.
Mistletoe Therapy
Less known in North America but widely used in Europe, mistletoe extract is a botanical therapy with deep roots in integrative oncology. It’s used to modulate immune function, reduce chemotherapy side effects, and improve energy and mood during treatment.
Mistletoe does more than merely “stimulate” the immune system. It helps recalibrate it. It supports natural killer cell activity and can improve the innate immune system’s ability to recognize and respond to tumor cells. Subcutaneous mistletoe injections are common, but intravenous formulations are also used in more advanced protocols. For many patients, mistletoe is a gentle yet potent therapy that helps the immune terrain recover its lost clarity.
Mind-Body Practices
One of the most underappreciated tools in cancer care is also one of the most accessible: the power of the mind to influence the terrain. We now know that chronic stress, unresolved trauma, and emotional suppression can dysregulate the HPA (hypothalamic-pituitary-adrenal) axis, impair immune function, disrupt digestion, and fuel systemic inflammation—all of which set the stage for terrain breakdown.
Mind-body practices aren’t just feel-good add-ons. They’re terrain interventions. Techniques like meditation, breathwork, yoga, biofeedback, somatic therapy, and even contemplative journaling can recalibrate stress physiology, reduce cortisol, and promote parasympathetic dominance—a state in which healing can occur. For patients in active treatment, these tools help modulate fear and restore a sense of agency. For those in remission, they become practices of integration and prevention.
Detoxification Support
Detox, as a concept, has been badly abused in the wellness world—reduced to fads, fasting gimmicks, and overpriced powders. But in the metabolic model, detoxification is neither marketing nor mystery—it’s biochemistry. The liver, kidneys, skin, lymph, and gut are all detox organs, and when burdened by ongoing exposure or impaired by inflammation, they struggle to clear waste efficiently.
Supporting detox involves several strategies: improving bile flow, using binding agents to capture toxins in the gut, sweating (via sauna or exercise), and supporting the liver’s enzymatic pathways with nutrients like NAC, glutathione, and milk thistle. Castor oil packs, dry brushing, and hydrotherapy may also be used to stimulate lymphatic drainage.
When applied intelligently—based on real data, not assumptions—detoxification becomes a powerful tool to reduce immune confusion, ease inflammation, and support mitochondrial repair.
Therapies That Work with, Not Against
A common concern for patients—and sometimes even their oncologists—is whether these therapies might interfere with standard cancer treatments. The short answer: they can, if used recklessly or without supervision. But when guided by trained professionals who understand both conventional and integrative oncology, these therapies are typically designed to work in harmony with standard care—not against it.
In fact, many integrative therapies may help reduce the side effects of chemotherapy or radiation, protect healthy tissues, and even enhance therapeutic efficacy. That said, timing matters. Dosing matters. And individualized terrain matters most of all.
This is not about “alternative” medicine. It’s about intelligent integration—adding tools to the toolkit, not throwing away the proven ones.
Choosing the Right Tools for the Right Terrain
Not every patient needs every therapy. The point of terrain-based care is not to do everything at once, but to assess where the body is most imbalanced and support that system with the most appropriate, least invasive, most effective intervention.
Some patients may need immune recalibration. Others need mitochondrial repair. Some need deep emotional integration. Others require detox support after decades of silent exposure. No two terrains are the same. And that’s exactly the point.
These integrative therapies are not fringe—they’re forward-thinking. They bring us closer to the kind of personalized, systems-oriented medicine that cancer demands and patients deserve.
Next, we’ll turn to the real-world application of this entire model: what it looks like when people use these principles not just in theory, but in the lived reality of treatment and healing.
It’s not just about humans, either. Terrain strategies are increasingly discussed in pet care too, like in Supplements for Dogs with Cancer.
Let’s move into case studies and clinical insights.
7. Comparing Conventional and Metabolic Approaches
By now, you’ve explored the metabolic approach from theory through practice, heard real stories, and begun to see how terrain matters. But here’s a question that’s probably on your mind—maybe even a sticking point:
How does this metabolic approach fit with conventional cancer care?
Are they at odds? Is one right and the other wrong?
Or can they actually complement each other?
Let’s unpack this—because understanding the relationship between these paradigms is key to making informed choices, whether you’re a patient, caregiver, or clinician.
▸ Conventional Oncology: The Frontline Fighter
Traditional cancer treatment focuses on directly attacking cancer cells. Surgery removes tumors, chemotherapy poisons rapidly dividing cells, radiation beams damage DNA to stop proliferation, and increasingly, targeted therapies and immunotherapies seek specific molecular vulnerabilities.
This approach is often aggressive—because cancer is aggressive. And it can be lifesaving. For many, conventional treatments have extended survival and sometimes delivered cures.
But here’s the paradox: these therapies can also be harsh on the very terrain—the body’s internal ecosystem—that supports recovery and resilience.
Side effects like fatigue, immune suppression, neuropathy, and gut damage are common. What’s more, conventional approaches often view cancer as a singular “enemy” to eradicate, focusing less on why the cancer emerged or how to prevent recurrence.
▸ The Metabolic Approach: The Terrain Strategist
The metabolic approach, by contrast, zooms out to look around the tumor, not just at it.
Instead of aiming solely at the cancer cells, it asks: What conditions within the body allowed these cells to grow unchecked? How can we change the internal environment to make cancer less hospitable?
It’s a paradigm grounded in systems biology, recognizing the complex interplay of metabolism, immunity, hormones, inflammation, and more.
▸ Are these approaches mutually exclusive?
Absolutely not. The best cancer care often involves integrating both.
Think of conventional oncology as the frontline infantry, directly confronting the tumor. The metabolic approach is the logistics and intelligence unit, ensuring the body’s systems are strong, well-nourished, and capable of supporting that fight—and importantly, preventing future battles.
Many integrative oncologists emphasize that metabolic therapies enhance the efficacy and reduce the toxicity of conventional treatments. For example:
- Ketogenic diets may sensitize tumors to radiation or chemotherapy.
- Detoxification protocols may help clear chemotherapy byproducts more efficiently.
- Immune-supporting therapies may improve response rates to immunotherapy.
▸ Why is metabolic care still not mainstream?
That’s a layered question.
Part of it stems from the inertia of medical education and research funding. Conventional oncology is deeply entrenched, with decades of trials, protocols, and standards. The metabolic approach challenges some of those assumptions—demanding a systems-level view that’s harder to study in traditional trial frameworks.
There’s also a cultural dimension: metabolic therapies often involve lifestyle changes and holistic interventions that require time, education, and patient engagement—something that busy clinics and quick treatments don’t always accommodate.
▸ Are there risks or downsides to the metabolic approach?
Like any medical strategy, it’s not without caveats.
One concern is that patients might forego proven conventional treatments in favor of metabolic therapies alone—a choice that can be dangerous if done without guidance.
Also, metabolic therapies require personalization and monitoring. Overly restrictive diets can cause malnutrition or worsen fatigue if not carefully managed. Detox protocols done improperly can strain organs.
That’s why collaboration with knowledgeable integrative oncologists is critical. The metabolic approach is best seen as an adjunct, not a substitute, unless under very specific, carefully monitored circumstances.
▸ How can patients navigate these complex choices?
Education and communication are key.
Ask questions. Seek practitioners who are transparent about evidence, limitations, and integration. Don’t hesitate to discuss all therapies you’re considering with your oncology team. Empower yourself with knowledge but balance it with humility about what’s known and unknown.
Bringing It Together
Conventional and metabolic approaches are two sides of the same coin. One addresses the cancer cells head-on. The other builds the battleground conditions—strengthening defenses, closing supply lines, and restoring balance.
Together, they form a comprehensive, nuanced cancer care strategy—one that honors the complexity of both disease and human biology.
As you consider this balance, you might reflect: Where am I in this spectrum? What role does my terrain play in my health? How can I participate actively in my care?
In our next section, we’ll look toward the horizon with Future Directions in Cancer Metabolism—exploring emerging research, new technologies, and the exciting frontier of personalized metabolic medicine.
8. Future Directions in Cancer Metabolism
By now, the metabolic approach should feel less like a niche curiosity and more like what it truly is: a paradigm shift—one that places the body’s terrain, not just its tumors, at the center of cancer care. But if this model already feels transformative, the real question is: what’s next?
| Tool or Therapy | What It Monitors or Modulates | Stage of Use |
|---|---|---|
| Continuous Ketone Monitors | Nutritional ketosis in real time | Early clinical / pilot use |
| Metabolomic Blood Panels | Systemic metabolic fingerprint | Emerging clinical practice |
| AI-driven Terrain Risk Stratification | Predictive inflammation models | Under development |
This isn’t just an academic exercise. It’s a vital, deeply practical inquiry. Because the metabolic approach isn’t static. It’s alive. It’s evolving. Shaped by scientific breakthroughs, wearable tech, personalized data, and a growing cultural awareness that health isn’t just about defeating disease—it’s about understanding the systems that sustain or erode resilience.
So let’s turn the lens forward. What’s on the horizon? What can patients and practitioners expect as metabolic oncology continues to mature?
Where is the Research Headed?
You might be surprised to learn that cancer metabolism—despite its early prominence in the 1920s with the Warburg effect—was, for decades, sidelined in favor of genetic theories. But now, it’s roaring back into focus.
Why? Because metabolism is proving to be not just relevant, but central. And advances in metabolomics—the real-time measurement of metabolites within cells and tissues—are revolutionizing how we understand cancer behavior.
Metabolomics allows researchers to trace the actual biochemical activity of tumors: what fuels they prefer (glucose, glutamine, fatty acids), what waste they produce, how they handle oxidative stress, and how they adapt under therapeutic pressure. In other words, we’re no longer just reading the tumor’s DNA—we’re listening to its metabolic voice.
This means future care may look nothing like today’s general protocols. Instead, we’ll see precise interventions based on each tumor’s metabolic signature. A patient with a glucose-addicted tumor might respond best to ketogenic therapy, while another might benefit from glutamine restriction or mitochondrial support. The path is no longer linear—it’s dynamic, data-informed, and tailored to biology in motion.
Personalized Metabolic Medicine: Not Just a Buzzword
“Personalized medicine” often gets reduced to genomics. But in the metabolic model, it takes on a richer meaning. It’s about real-time physiology. It’s about how your terrain is behaving right now—not just what mutations your tumor carries.
Let’s be clear: two patients with the same cancer diagnosis can have entirely different metabolic environments. One may have high insulin, poor sleep, elevated cortisol, and gut dysbiosis. Another may have robust glucose control but severe mitochondrial dysfunction. Their terrain vulnerabilities—and therefore, their therapeutic needs—are completely different.
What’s coming is a model where metabolic assessments (blood sugar variability, oxygen utilization, nutrient metabolites, even emotional stress markers) guide day-to-day decisions. Diet, supplements, movement, even treatment timing will be dynamically adjusted based on your own internal feedback loop.
It’s personalized care, not based on a static profile—but on a living, breathing system.
Technology Will Be the Bridge
You’ve probably seen the rise of continuous glucose monitors (CGMs) in metabolic health circles. But that’s only the beginning.
Emerging wearable and implantable sensors will soon be capable of tracking multiple variables: inflammation markers, mitochondrial function, microbiome metabolites, cortisol rhythms, and more. These data streams, analyzed by machine learning, won’t just provide pretty dashboards—they’ll offer predictive insights.
Imagine a platform that alerts you when your immune resilience is declining. Or one that flags terrain shifts weeks before a recurrence would appear on a scan. These tools are coming—and they’ll reshape not just cancer care, but health monitoring writ large.
The real transformation lies in proactive care—intervening before crisis, guided by subtle shifts in metabolic terrain.
Can This Model Truly Integrate with Mainstream Oncology?
That’s the challenge—and the great hope.
Some integration is already happening. Pilot studies combining ketogenic diets with chemotherapy, or hyperbaric oxygen with radiation, are showing that terrain support can enhance treatment response while buffering side effects. Immunotherapy, in particular, seems to perform better when metabolic inflammation is managed and immune terrain is nourished.
But for full integration to occur, the system must change. Medical education will need to include terrain principles. Insurance will need to value prevention and systems care. Oncologists will need to see lifestyle as a central axis of therapy, not a soft afterthought.
Still, the momentum is building. Patient demand is rising. Clinical data is accumulating. And forward-thinking practitioners are beginning to ask: How do we bring the best of both worlds together?
Emerging Therapies on the Metabolic Horizon
While lifestyle remains the cornerstone of the metabolic model, research into targeted metabolic therapies is heating up.
We’re seeing drug candidates that block glycolysis, inhibit fatty acid oxidation, or interrupt glutamine pathways—all ways to deprive cancer cells of their preferred fuel. These aren’t just theoretical; many are moving into early-phase trials.
Meanwhile, natural compounds like berberine, resveratrol, and curcumin are being refined into pharmacologically active agents with multi-pathway effects. Microbiome modulators are being engineered to rebalance gut terrain and immune signaling.
Even psychedelics are entering the field—not just for psychological healing, but for their impact on neuroendocrine systems, cellular stress responses, and gene expression.
This doesn’t mean the future is drug-dominated. Rather, it will be terrain-aware, using pharmaceutical precision to enhance—not replace—foundational metabolic strategies.
What Should Patients Focus on Now?
The future is thrilling. But the present still matters most.
No AI can replace self-awareness. No wearable can override what your body is already telling you. The heart of terrain medicine is still embodiment—knowing your signals, honoring your needs, and working with practitioners who respect complexity over protocol.
If you’re navigating cancer today, or working to reduce risk for the future, here’s the enduring truth: metabolic health is a daily practice. Not perfection. Not purity. Practice.
Focus on what you can measure, what you can influence, and what supports your system in real time—whether that’s a cleaner diet, better sleep, a less stressful morning routine, or a conversation you’ve been avoiding.
You are the terrain. And the future is not separate from your body—it’s unfolding inside it, cell by cell, breath by breath.
Frequently Asked Questions (FAQs)
You’ve absorbed a lot so far, and naturally, some questions may be bubbling up. That’s exactly what this section is for — to tackle the queries, doubts, and curiosities that often arise when exploring the metabolic approach to cancer.
Let’s dive into the top questions we hear, unpack them thoughtfully, and give you clear, nuanced answers.
1. What exactly is the metabolic approach to cancer?
Great question. At its core, the metabolic approach views cancer not just as a genetic disease but as one deeply influenced by the body’s internal environment or “terrain.” It focuses on modifying metabolic factors—like blood sugar, inflammation, toxins, immune function, and hormones—that create conditions favorable to cancer growth. Instead of attacking cancer cells directly alone, it emphasizes optimizing the whole-body environment to starve, suppress, and prevent tumor proliferation.
2. How does the ketogenic diet help in cancer care?
The ketogenic diet lowers glucose availability and insulin levels, two factors cancer cells heavily rely on. By shifting metabolism to burn fat and produce ketones, it creates an environment less hospitable to many tumors. Ketones themselves may have anti-inflammatory and anti-cancer signaling effects. However, keto is not a cure-all and must be personalized and carefully monitored to avoid nutrient deficiencies or hormonal disruption.
3. Can I use the metabolic approach alongside conventional treatments?
Absolutely—and often, it’s recommended. Integrative care combines conventional oncology (surgery, chemo, radiation) with metabolic therapies that support immune function, reduce side effects, and improve overall resilience. Open communication with your oncology team is crucial to ensure therapies complement rather than conflict.
4. Is the metabolic approach effective for all types of cancer?
While promising across many cancer types, the metabolic approach’s effectiveness varies based on tumor biology, stage, and individual patient factors. Some cancers, like glioblastoma or hormone-driven breast cancer, show particular metabolic vulnerabilities. The approach is always personalized, often as an adjunct rather than a standalone therapy.
5. How do I get started with a metabolic approach?
Begin with assessment: comprehensive labs evaluating glucose metabolism, inflammation, hormones, immune markers, and toxins. Work with a practitioner experienced in metabolic oncology or integrative medicine. Dietary adjustments, sleep optimization, stress reduction, and targeted supplementation often follow. Remember, it’s a journey, not a quick fix.
6. Are there risks or downsides to ketogenic diets or fasting?
Yes—while beneficial for many, keto and fasting can be challenging for some, especially those with adrenal fatigue, thyroid issues, or advanced cancer causing weight loss. Improperly managed, they can cause fatigue, nutrient imbalances, or stress. Clinical supervision and personalized adjustments are essential.
Closing Thought
The metabolic approach to cancer reframes the disease not as a random enemy, but as a signal from a disrupted internal environment—a terrain in need of restoration. This perspective empowers patients to become active participants in their healing by focusing on metabolic, immune, hormonal, and emotional balance. While not a guaranteed cure, the approach complements conventional treatments, helping the body recover, resist recurrence, and sustain resilience.
It’s not about heroic perfection, but daily, intelligent choices—balancing blood sugar, improving sleep, reducing inflammation, and engaging meaningfully with practitioners and one’s own biology. The approach reintroduces agency, hope, and relationship into the cancer journey. Ultimately, it invites each person to ask: How do I want to engage with my health? And then to act—not from fear, but from informed courage.










