Managing Heart Skipping Beats and Protecting Heart Rhythm
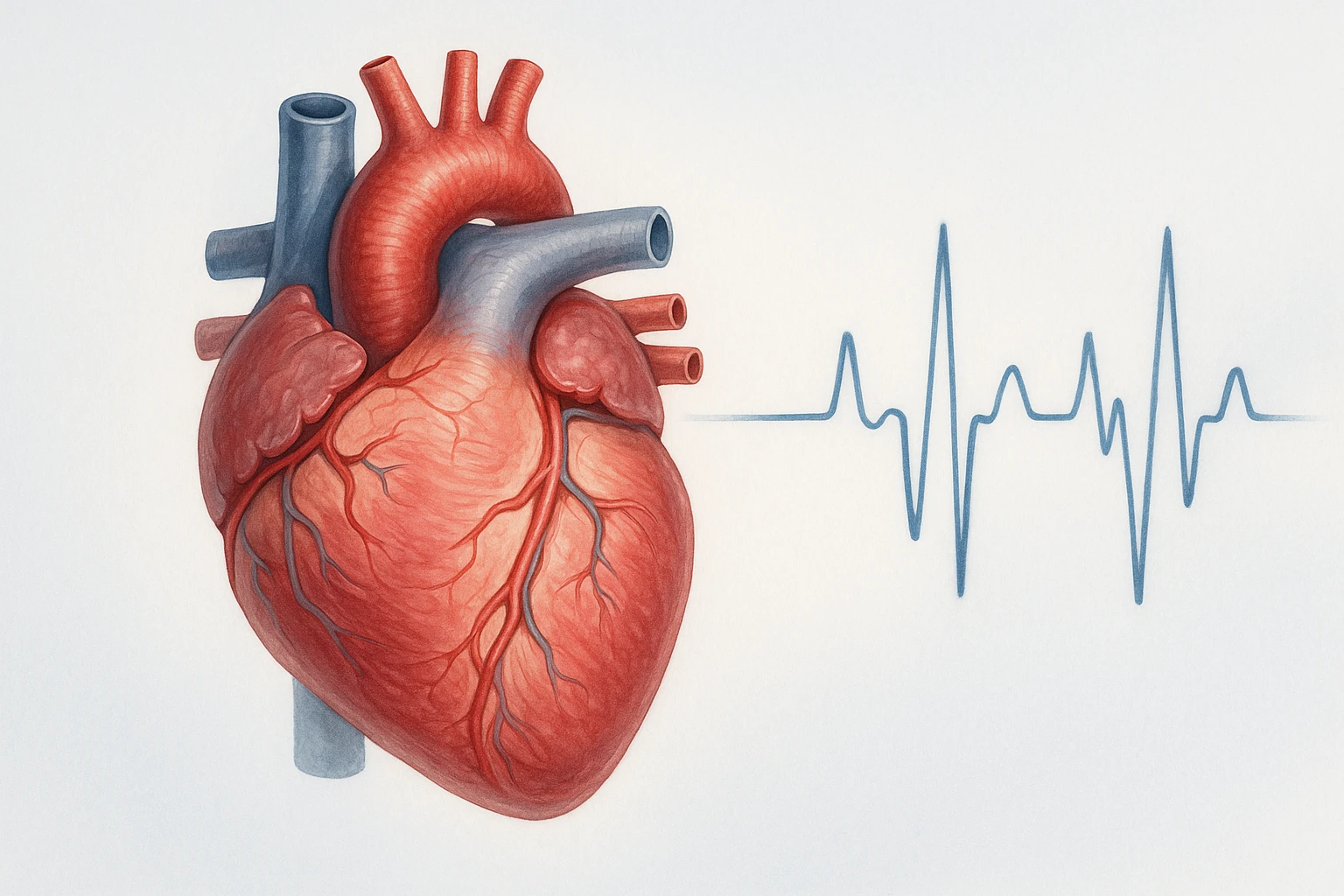
When the Heart Skips a Beat
The sensation that the heart has “skipped a beat” is a common and often unsettling experience. In most cases, it reflects a premature contraction of the heart-either from the atria or the ventricles-followed by a brief pause and then a stronger beat. This transient irregularity is typically benign and represents a momentary disruption in the normal cardiac rhythm rather than a sustained arrhythmia.
Physiologic Mechanism
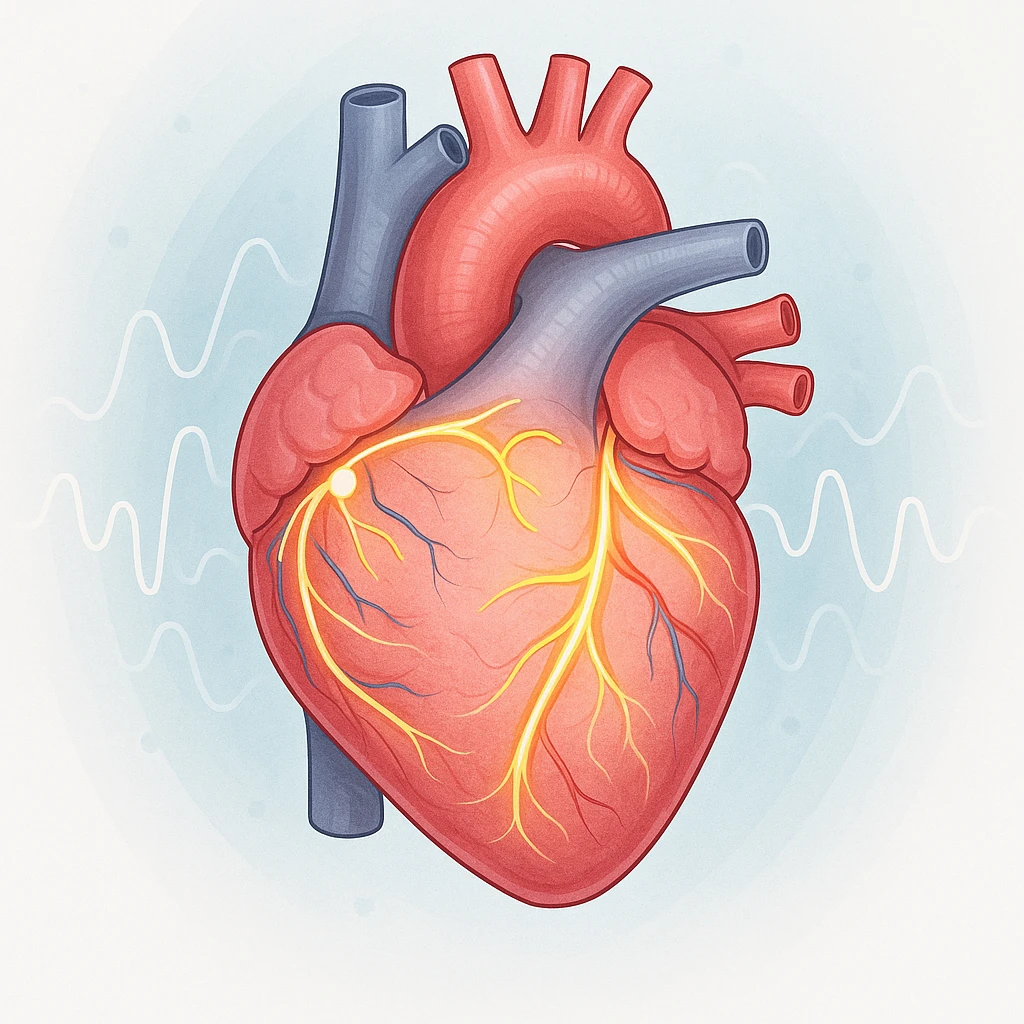
When a premature atrial or ventricular contraction occurs, the electrical impulse arises earlier than expected in the cardiac cycle. This early depolarization causes a brief pause before the next scheduled heartbeat. During the pause, the ventricles have more time to fill with blood, and the subsequent contraction is felt as a stronger or more forceful beat. Patients often interpret this sequence-a pause followed by a thump-as a skipped or missed beat, though the heart has in fact generated an extra contraction.
- Premature Atrial Contractions (PACs): Extra beats originating in the atria.
- Premature Ventricular Complexes (PVCs): Extra beats originating in the ventricles.
These isolated events are commonly detected in routine cardiac monitoring. They can occur in otherwise healthy individuals and are often asymptomatic aside from the transient perception of irregularity.
How Common Are Skipped Beats?
Premature beats are a frequent finding in clinical practice and during ambulatory electrocardiographic monitoring. Isolated PVCs, for example, are detected in a substantial proportion of healthy adults, even in the absence of structural heart disease. Their frequency tends to rise with advancing age and with the accumulation of cardiovascular risk factors such as hypertension or ischemic heart disease. Despite their prevalence, most incidental PVCs in structurally normal hearts do not progress to significant arrhythmia or cause long-term harm.
- Common in healthy individuals.
- Increase with age and cardiovascular risk factors.
- Usually benign when no structural heart disease is present.
This high prevalence underscores the importance of distinguishing between benign, isolated ectopic beats and rhythm disturbances that require further evaluation. For many patients, reassurance based on appropriate diagnostic assessment is sufficient.
Differentiating Benign Palpitations from Arrhythmias
While isolated ectopic beats are typically harmless, sustained or frequent irregularities may indicate a more significant rhythm disorder. Benign palpitations are generally brief and occur without associated symptoms such as syncope, chest pain, or shortness of breath. In contrast, arrhythmias involving prolonged irregular rhythm or hemodynamic compromise warrant further investigation. Understanding this distinction helps clinicians reassure patients experiencing benign ectopy while remaining alert to patterns suggestive of underlying pathology.
| Feature | Benign Palpitations | Concerning Arrhythmias |
|---|---|---|
| Duration | Brief, self-limited | Prolonged or recurrent |
| Associated symptoms | None or mild awareness | Syncope, chest pain, dyspnea |
| Hemodynamic effect | Minimal | Possible compromise |
Causes and Triggers of Heart Skipping Beats
Skipped or irregular heartbeats, often perceived as a flutter or pause, can originate from a variety of physiological and pathological factors. In many individuals, premature ectopic beats occur even when the heart is structurally normal. However, in others, underlying cardiac or systemic conditions can contribute to more frequent or symptomatic episodes. Understanding these mechanisms helps distinguish benign triggers from those linked to cardiac disease.
Cardiac and Structural Factors
Certain forms of heart disease can predispose to premature beats by altering the electrical or mechanical function of the myocardium. Structural heart abnormalities, including cardiomyopathies or ventricular hypertrophy, may create areas of irritability where spontaneous depolarizations occur. Myocardial ischemia can also disrupt normal conduction pathways, increasing the likelihood of ectopic activity. In these cases, premature contractions are not isolated findings but reflect an altered cardiac substrate that facilitates abnormal automaticity or reentry circuits.
- Cardiomyopathies or ventricular hypertrophy may increase electrical irritability.
- Ischemic injury can interfere with normal conduction pathways.
- Frequent or multifocal ectopic beats may signal structural heart disease.
Although these structural causes are less common in otherwise healthy individuals, recognizing them is important since the frequency or complexity of ectopy may rise in their presence. The detection of frequent or multifocal ectopic beats should prompt evaluation for underlying heart disease to determine whether structural or ischemic changes are contributing to the arrhythmic tendency.
Lifestyle and Metabolic Triggers
Premature beats are frequently provoked by reversible or external influences. Heightened sympathetic tone-caused by stress, anxiety, or exertion-can stimulate the heart’s conduction system and make ectopic discharges more likely. Common stimulants such as caffeine, nicotine, and certain over-the-counter medications can have a similar effect. Endocrine and metabolic factors, including thyroid imbalance or electrolyte disturbances, may also disrupt normal cardiac excitability. Identifying and addressing these modifiable triggers can often reduce the occurrence of heart skipping beats in otherwise normal hearts.
- Increased sympathetic activity (stress, anxiety, exertion).
- Stimulant use (caffeine, nicotine, certain medications).
- Endocrine or metabolic imbalances (thyroid, electrolytes).
Because these triggers act through transient physiologic mechanisms rather than permanent damage to the heart, their effects are typically reversible once the precipitating factor is corrected or minimized. This distinction highlights the importance of a comprehensive review of lifestyle and metabolic contributors when assessing patients with palpitations.
Premature Atrial vs. Ventricular Contractions
Ectopic beats can arise from different regions within the heart, and their site of origin determines their classification. Premature atrial contractions (PACs) originate in the atria, while premature ventricular complexes (PVCs) arise from the ventricles. Both types may cause the sensation of a skipped beat, but PVCs are often associated with a more forceful post-ectopic contraction because of the longer compensatory pause that follows. In most healthy individuals, either form of ectopy is benign, though frequent or complex PVCs may warrant closer evaluation, especially if structural abnormalities are present.
| Type of Ectopic Beat | Origin | Typical Sensation |
|---|---|---|
| Premature Atrial Contraction (PAC) | Atria | Mild flutter or pause |
| Premature Ventricular Complex (PVC) | Ventricles | Stronger thump after a longer pause |
Myths vs Facts About Heart Skipping Beats
- Myth: All skipped beats indicate serious heart disease.
Fact: Many skipped beats occur in healthy individuals without structural abnormalities and are not dangerous. - Myth: Skipped beats only happen because of stress or anxiety.
Fact: While stress can trigger them, other factors such as stimulants, medications, and metabolic changes also play a role.
Evaluating Patients with Heart Skipping Beats
The evaluation of a patient who reports a sensation of skipped or irregular heartbeats requires a systematic approach that distinguishes benign ectopy from clinically significant arrhythmias. This process integrates history, examination, and appropriate diagnostic testing to clarify the underlying rhythm disturbance and assess potential structural or systemic contributors.
Initial Clinical Assessment
The first step in evaluation is a thorough history focused on symptom description, onset, duration, and associated features such as dizziness, chest discomfort, or exertional intolerance. Contextual factors-including stimulant intake, stress, or medication use-should also be explored. A detailed cardiovascular examination may reveal signs of structural heart disease or abnormal hemodynamics that guide further testing.
- Assess symptom characteristics and triggers (timing, frequency, duration).
- Review stimulant intake, stress levels, and medication use.
- Perform cardiovascular examination to detect murmurs, gallops, or signs of structural disease.
A standard 12-lead electrocardiogram (ECG) remains the cornerstone of initial assessment. It can document premature atrial or ventricular complexes, evaluate for underlying conduction abnormalities, and identify repolarization changes suggestive of ischemia or structural pathology. Even a normal ECG, however, does not exclude intermittent ectopy, underscoring the importance of correlating findings with the clinical history.
Ambulatory and Advanced Monitoring
When symptoms are infrequent or not captured on an initial ECG, ambulatory rhythm monitoring provides valuable diagnostic information. A 24- or 48-hour Holter monitor is useful when symptoms occur daily, while extended event recorders or patch monitors can capture less frequent episodes over several weeks. These devices correlate symptoms with documented rhythm disturbances, helping to distinguish benign premature beats from sustained arrhythmias.
| Monitoring Method | Duration | Best For |
|---|---|---|
| Holter Monitor | 24-48 hours | Daily or frequent symptoms |
| Event Recorder | 1-4 weeks | Intermittent episodes |
| Patch Monitor | Up to 2 weeks | Less frequent palpitations |
Emerging wearable technologies and smartphone-based ECG tools can supplement conventional monitoring, particularly when episodes are sporadic or brief. Regardless of the modality, the goal is to obtain rhythm documentation that aligns with the patient’s reported symptoms to support accurate diagnosis and management.
When to Escalate Testing
Further evaluation is warranted when initial assessment suggests structural heart disease or when red flags are present. Indications for additional testing include a high burden of ectopy, multifocal premature ventricular complexes, or symptoms such as syncope, exertional dyspnea, or chest pain. Transthoracic echocardiography is typically the next step to assess cardiac structure and function, including ventricular size, wall motion, and ejection fraction.
- High ectopic burden or complex ventricular patterns.
- Syncope, exertional symptoms, or chest discomfort.
- Abnormal baseline ECG or suspected cardiomyopathy.
In selected cases, more advanced investigations-such as stress testing, cardiac MRI, or referral for electrophysiologic consultation-may be appropriate to evaluate arrhythmia mechanisms or identify underlying myocardial disease. These escalated steps are guided by clinical suspicion and the overall risk profile, ensuring a patient-centered, evidence-based diagnostic process.
Assessing Risk and Prognosis in Heart Skipping Beats
Evaluating the clinical significance of premature ventricular complexes (PVCs) requires a careful assessment of the patient’s cardiac structure, frequency of ectopy, and symptom burden. While occasional PVCs are frequently benign, certain patterns or associated findings may indicate increased risk for adverse outcomes or progressive myocardial dysfunction. Risk stratification therefore centers on distinguishing harmless ectopy from arrhythmias that may lead to structural or functional deterioration.
Benign vs. Pathologic Ectopy
In individuals with normal cardiac anatomy and no evidence of underlying heart disease, PVCs and other forms of ectopy are generally benign. These patients typically exhibit a low frequency of premature beats, normal left ventricular function, and absence of concerning symptoms such as syncope or exertional dyspnea. The prognosis in this group is excellent, and most do not experience progression to sustained arrhythmia or cardiac dysfunction.
- Features of benign ectopy: Normal cardiac structure, low PVC frequency, absence of worrisome symptoms.
- Features of pathologic ectopy: Structural abnormalities, ischemic heart disease, or conduction disturbances increasing arrhythmia risk.
In contrast, pathologic ectopy is characterized by its association with structural abnormalities or significant conduction disturbances. PVCs arising in patients with cardiomyopathy, ischemic heart disease, or prior myocardial injury carry a higher likelihood of malignant ventricular arrhythmias. In such contexts, ectopic activity may serve as a marker of myocardial irritability or electrical instability, warranting closer surveillance and targeted management.
PVC Burden and Structural Heart Disease
The frequency, or burden, of PVCs has important prognostic implications. A very high PVC burden over time can contribute to left ventricular dysfunction and the development of PVC-induced cardiomyopathy. This condition is often reversible if the ectopic activity is reduced, either through medical therapy or catheter ablation. Recognition of this link emphasizes the importance of quantifying ectopy in patients with unexplained reductions in ventricular function.
| Clinical Context | Associated Risk | Prognosis |
|---|---|---|
| Normal heart structure, low PVC frequency | Low | Generally benign |
| High PVC burden, normal heart | Moderate | Possible reversible cardiomyopathy if untreated |
| Structural heart disease with frequent PVCs | High | Increased risk of malignant arrhythmia and heart failure |
When PVCs occur against the background of established structural heart disease, the risk of adverse outcomes increases substantially. These patients are more susceptible to malignant ventricular arrhythmias and heart failure progression. Conversely, in individuals with structurally normal hearts and modest ectopic activity, the long-term prognosis remains favorable. Differentiating between these risk groups guides both the intensity of follow-up and the need for intervention.
Management, Red Flags, and Emerging Frontiers in Heart Skipping Beats
The management of heart skipping beats, also known as skipped or premature heartbeats, focuses on identifying underlying causes, alleviating symptoms, and preventing potential complications. While many cases are benign, recognizing when intervention is warranted is crucial for ensuring patient safety and optimizing outcomes.
Management Approach
For asymptomatic individuals with benign ectopy and no structural heart disease, observation and reassurance are often sufficient. Routine follow-up rather than aggressive intervention is appropriate in this context. For patients with identifiable triggers, management begins with lifestyle and environmental modification.
- Reduce stimulant intake such as caffeine and nicotine.
- Manage stress and address anxiety-related triggers.
- Correct reversible metabolic or endocrine abnormalities, including thyroid or electrolyte disturbances.
Pharmacologic treatment is reserved for patients with bothersome symptoms or higher arrhythmic risk. Beta-blockers are the preferred first-line agents for symptomatic ectopy, as they reduce adrenergic stimulation and ectopic firing. In select cases, other antiarrhythmic drugs may be considered under specialist supervision. For patients with a high premature ventricular complex (PVC) burden contributing to left ventricular dysfunction or refractory symptoms, catheter ablation offers a targeted and effective intervention by eliminating the ectopic focus.
Recognizing Red Flags
Although most skipped beats are benign, certain symptoms indicate a higher risk for significant arrhythmia or structural heart disease. Palpitations accompanied by syncope, presyncope, or severe dizziness require prompt evaluation, as they may signal hemodynamic compromise or ventricular tachyarrhythmia. Similarly, the presence of chest pain, shortness of breath, or exertional intolerance suggests possible ischemic or structural pathology and warrants urgent investigation.
When to See a Doctor
- New or worsening palpitations accompanied by fainting or near-fainting episodes.
- Chest pain, dyspnea, or symptoms triggered by exertion.
- Frequent or irregular skipped beats in patients with known heart disease.
New Frontiers and Common Misconceptions
Advances in ambulatory rhythm monitoring and consumer wearables have expanded the ability to capture transient arrhythmias in real time. These tools improve diagnostic accuracy when traditional methods fail to document infrequent episodes. Ongoing research continues to refine thresholds for PVC burden and explore mechanisms of reversible PVC-induced cardiomyopathy, helping clinicians tailor intervention more precisely.
Common misconceptions persist about skipped beats. Not every irregular rhythm indicates a dangerous condition, and anxiety alone is not always the cause. Most ectopy in structurally normal hearts remains benign and manageable through lifestyle adjustments. Clarifying these distinctions helps reduce unnecessary anxiety and ensures that medical attention is directed toward cases requiring true clinical intervention.
Frequently Asked Questions About Heart Skipping Beats
- Is it normal to feel like your heart skips a beat?
- Yes, many people occasionally experience skipped or extra beats. These usually result from harmless premature contractions and are not a sign of heart disease.
- Why do skipped heartbeats feel stronger afterward?
- The sensation of a stronger beat occurs because the heart briefly pauses after a premature contraction, allowing more blood to fill before the next normal beat.
- Can stress or caffeine really cause heart skipping beats?
- Yes. Stress, anxiety, caffeine, and nicotine can increase adrenaline levels, making the heart’s electrical system more excitable and prone to extra beats.
- When should skipped beats be considered a warning sign?
- Skipped beats accompanied by fainting, dizziness, chest pain, or shortness of breath may indicate a more serious rhythm disturbance and should be evaluated promptly.
- Are skipped beats dangerous for people with healthy hearts?
- In most individuals with normal heart structure, skipped beats are benign and cause no long-term harm. They often improve with stress management and reduced stimulant use.
- Can exercise trigger or worsen heart skipping beats?
- Exercise temporarily increases heart rate and adrenaline, which can make premature beats more noticeable. However, regular physical activity generally supports heart health overall.
- How do doctors test for irregular or skipped heartbeats?
- Evaluation usually includes a medical history, physical exam, and an ECG. If episodes are intermittent, a Holter or event monitor can record them over time.
- Can skipped beats be treated or prevented?
- Treatment focuses on addressing triggers like caffeine, stress, or hormonal changes. Medications such as beta-blockers or procedures like ablation are used only when symptoms persist.
- Do heart skipping beats mean you’re at risk for arrhythmia?
- Most skipped beats are isolated and harmless. However, frequent or complex premature beats, especially in people with heart disease, may warrant closer medical follow-up.
- Can wearable devices detect skipped heartbeats?
- Yes. Many modern wearables can record short ECGs or track rhythm irregularities, helping doctors document occasional episodes that might otherwise go unnoticed.