Lower Eyelid Cancer: Comprehensive Guide to Diagnosis, Treatment, and Recovery
- Understanding Lower Eyelid Cancer
- Recognizing Early Symptoms
- Diagnostic Procedures
- Treatment Options
- Stages of Lower Eyelid Cancer
- Histological Subtypes of Lower Eyelid Cancer
- Lower Eyelid Cancer Pictures
- Importance of Multidisciplinary Management
- Postoperative Recovery and Rehabilitation
- Long-Term Follow-Up and Risk of Recurrence
- Prognosis and Survival Outlook
- Psychological Impact and Cosmetic Concerns
- Prevention and Sun Protection Strategies
- Global Perspectives on Lower Eyelid Cancer Care
- Innovations in Reconstructive Techniques
- Vigilance, Precision, and Patient-Centered Care
- FAQ

Understanding Lower Eyelid Cancer
Lower eyelid cancer encompasses various malignancies that originate in the tissues of the lower eyelid. The most common types include basal cell carcinoma, squamous cell carcinoma, sebaceous gland carcinoma, and, less frequently, melanoma. Basal cell carcinoma is the most prevalent, often linked to prolonged sun exposure, and typically presents as a pearly nodule or ulcerated lesion. Squamous cell carcinoma may appear as a scaly or crusted patch, while sebaceous gland carcinoma often masquerades as benign conditions like chalazion, leading to delayed diagnosis. Melanoma, though rare in the eyelid, is aggressive and requires prompt attention.
The thin skin and unique anatomy of the eyelid make it particularly susceptible to UV damage, a significant risk factor for these cancers. Other risk factors include fair skin, advanced age, immunosuppression, and previous radiation exposure. Understanding these factors is essential for early detection and prevention strategies.
Recognizing Early Symptoms
Early detection of lower eyelid cancer significantly improves treatment outcomes. Common early signs include persistent redness, swelling, or a lump on the eyelid that doesn’t resolve. Patients may notice changes in eyelid appearance, such as thickening, loss of eyelashes, or a sore that bleeds or doesn’t heal. In some cases, the lesion may resemble benign conditions, leading to misdiagnosis. Therefore, any persistent or unusual changes in the eyelid should prompt evaluation by a healthcare professional.
It’s worth noting that certain non-invasive treatments, like microcurrent therapy, have been discussed in the context of their potential effects on cellular activity. While there’s no direct evidence linking such therapies to cancer development, it’s essential to approach new treatments with caution and consult medical professionals regarding their safety and efficacy.

Diagnostic Procedures
Accurate diagnosis of lower eyelid cancer involves a combination of clinical evaluation and diagnostic tests. A thorough physical examination by an ophthalmologist or dermatologist is the first step, focusing on the lesion’s characteristics and any associated symptoms. If cancer is suspected, a biopsy is performed to obtain a tissue sample for histopathological analysis, confirming the diagnosis and identifying the cancer type.
Imaging studies, such as MRI or CT scans, may be utilized to assess the extent of the tumor and its involvement with surrounding structures. These imaging modalities are crucial for staging the cancer and planning appropriate treatment strategies. In cases where sebaceous gland carcinoma is suspected, additional evaluations, including sentinel lymph node biopsy, may be necessary due to its potential for regional spread.
Treatment Options
Treatment of lower eyelid cancer is tailored to the cancer type, size, location, and patient’s overall health. Surgical excision remains the primary treatment modality, aiming to remove the tumor entirely while preserving as much healthy tissue as possible. Mohs micrographic surgery is often employed for its precision in excising cancerous cells while sparing healthy tissue, making it ideal for the delicate eyelid area.
In cases where surgery may not be feasible or as an adjunct to surgery, radiation therapy is considered. This modality uses high-energy rays to target and destroy cancer cells, often employed when tumors are large, recurrent, or in patients who cannot undergo surgery. Chemotherapy is less commonly used but may be indicated in advanced cases or specific cancer types like sebaceous gland carcinoma.
Reconstructive surgery is often necessary following tumor excision to restore eyelid function and appearance. Techniques vary based on the defect’s size and location, ranging from local flaps to skin grafts. The goal is to achieve optimal functional and cosmetic outcomes, ensuring the patient’s quality of life is maintained.
Stages of Lower Eyelid Cancer
Staging eyelid cancer helps determine the tumor’s severity, spread, and appropriate treatment path. The most widely used system is the AJCC (American Joint Committee on Cancer) TNM classification. “T” describes the size and extent of the primary tumor, “N” reflects whether nearby lymph nodes are affected, and “M” identifies the presence of distant metastasis.
Stage 0 represents carcinoma in situ — a precancerous change limited to the surface epithelium. Stage I indicates a small tumor confined to the eyelid without invasion. As stages progress (II–IV), tumors may involve deeper tissues, orbit structures, or regional lymph nodes. Advanced stages carry a higher risk of recurrence and require more aggressive treatment, often combining surgery, radiation, and systemic therapies.
Accurate staging is crucial for planning surgery, selecting appropriate adjuvant therapy, and predicting outcomes. Just like in prostate cancer, where the survival rate drastically changes based on Gleason score and tumor stage, lower eyelid cancer staging directly correlates with prognosis. The need for timely and precise evaluation echoes what we see with PI-RADS 4 lesions in prostate cancer patients, where early interpretation changes survival trajectory.
Histological Subtypes of Lower Eyelid Cancer
| Cancer Type | Common Appearance | Risk of Recurrence | Aggressiveness | Notes |
| Basal Cell Carcinoma (BCC) | Pearly nodule, ulcer with rolled edges | Moderate | Low to medium | Most common, rarely metastasizes |
| Squamous Cell Carcinoma | Crusty plaque or ulcer, may bleed | Higher than BCC | Medium to high | Can metastasize locally or regionally |
| Sebaceous Gland Carcinoma | Yellowish lesion or chronic eyelid swelling | High | High | Mimics benign lesions, often delayed |
| Melanoma | Pigmented lesion, may ulcerate | Variable | Very high | Rare but aggressive |
Understanding the type of cancer is essential because each subtype behaves differently in terms of recurrence, invasiveness, and need for follow-up. For example, sebaceous gland carcinoma is notorious for masquerading as a benign chalazion and spreading microscopically, requiring wide excision and sometimes systemic chemotherapy.

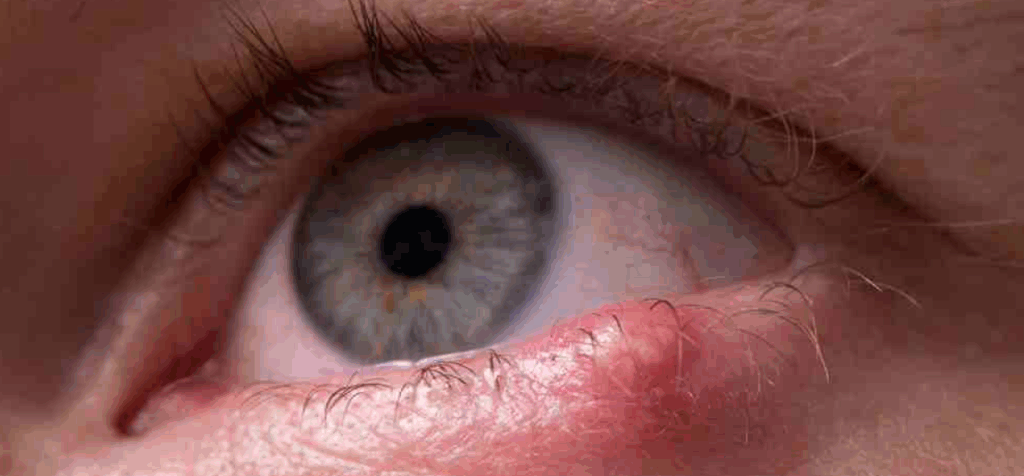
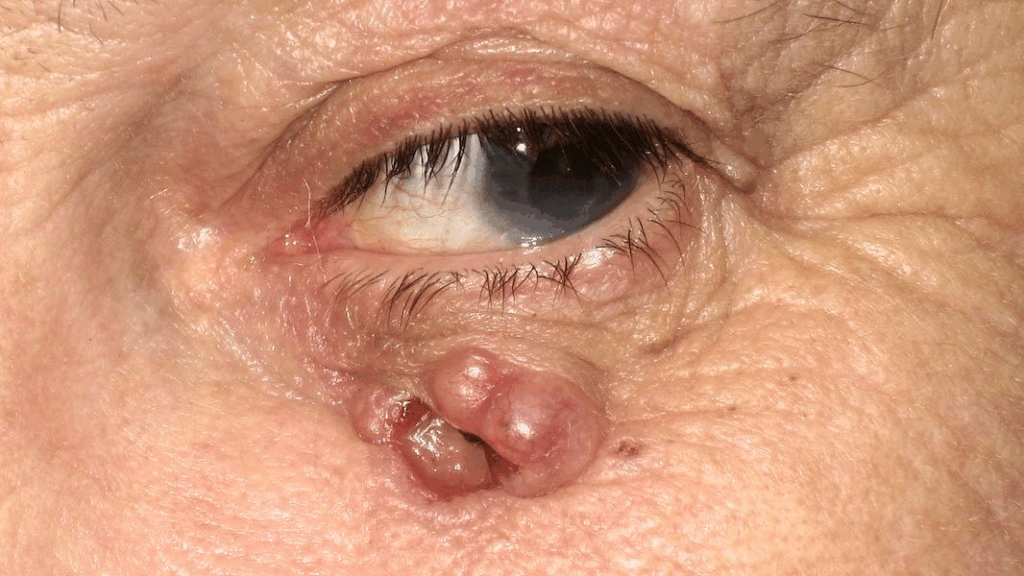
Lower Eyelid Cancer Pictures
Images play a critical role in medical education and patient awareness, especially when cancers mimic common benign conditions. Lower eyelid cancer may resemble a persistent stye, chronic blepharitis, or chalazion. Visual documentation helps differentiate these and fosters early recognition.
Typical early-stage basal cell carcinoma may appear as a shiny, translucent bump with visible blood vessels. More advanced lesions can ulcerate, forming crusty or bleeding surfaces. Squamous cell carcinoma may form a scaly or wart-like lesion that grows over weeks or months. Sebaceous gland carcinoma often causes eyelid thickening or a slowly enlarging mass beneath the skin, occasionally leading to misdiagnosis and delayed treatment.
Images should be interpreted in clinical context, and any concerning lesion should prompt medical evaluation. Never rely on pictures for self-diagnosis — only a trained specialist with biopsy confirmation can distinguish malignancy from harmless skin changes.
Importance of Multidisciplinary Management
Effective treatment of lower eyelid cancer requires collaboration between ophthalmologists, dermatologic surgeons, oncologists, pathologists, and reconstructive specialists. Initial evaluation is often performed by an ophthalmologist trained in ocular oncology or a dermatologic surgeon familiar with periocular anatomy.
If cancer is confirmed, surgical planning must balance complete tumor removal with functional and aesthetic preservation. Reconstructive specialists may be involved even before excision, especially for tumors expected to involve large portions of the lid or tear drainage system.
Pathologists ensure complete margin evaluation, particularly during Mohs surgery, while oncologists may advise on radiation or chemotherapy for aggressive subtypes. Regular follow-up and coordination reduce recurrence risk and support better long-term outcomes.
This team-based model mirrors how other complex cancers — such as prostate and ovarian — are managed in modern cancer care, where integrated teams ensure that no clinical aspect is overlooked.
Postoperative Recovery and Rehabilitation
Recovery after surgery for lower eyelid cancer depends on the extent of excision and the type of reconstruction performed. In minor cases where the tumor is removed with minimal tissue sacrifice, patients may resume normal activities within a week. However, more extensive resections involving full-thickness eyelid removal or orbital tissues require longer recovery and careful postoperative management.
Initial healing focuses on wound closure, swelling reduction, and infection prevention. Eye lubrication with ointments or drops is common to prevent exposure-related dryness if eyelid closure is incomplete. Sutures are usually removed within a week, though in complex reconstructions, absorbable stitches may be used.
Functionality — particularly the ability to blink, maintain corneal protection, and manage tear drainage — is closely monitored. Cosmetic results are also assessed, and revisions are sometimes needed months later for symmetry or eyelid contour refinement. Physical and emotional rehabilitation, including psychological support, is encouraged in cases of visible scarring or anxiety.
It’s essential to remember that even non-invasive aesthetic technologies, such as low-level electrical therapies, should be approached with caution postoperatively. Concerns about subtle bioelectrical effects on tissue recovery — as discussed in Can Microcurrent Cause Cancer — remain relevant in sensitive anatomical areas like the periocular zone.
Long-Term Follow-Up and Risk of Recurrence
Patients treated for lower eyelid cancer require structured follow-up for years after surgery. The risk of local recurrence or the development of new skin cancers on adjacent facial areas is real, especially in those with fair skin, a history of sun damage, or immunosuppression.
In the first year post-treatment, follow-up visits every three months are recommended to inspect the surgical site and check for suspicious changes. Annual full-body skin exams are advisable, as patients with eyelid skin cancer have an increased lifetime risk of developing basal or squamous cell carcinoma elsewhere.
Particular attention is paid to cases involving sebaceous gland carcinoma, which may recur at a microscopic level and metastasize to lymph nodes. These patients often undergo sentinel node biopsies and regional lymphatic imaging during follow-up.
Interestingly, this vigilance parallels the need for continued monitoring in hormonally influenced cancers — such as ovarian cancer — where early symptoms can be subtle and recurrent disease may manifest long after remission. The importance of sustained awareness is emphasized in our article on First Symptoms of Ovarian Cancer.
Prognosis and Survival Outlook
The prognosis of lower eyelid cancer is generally favorable, especially when diagnosed early and treated completely. For basal cell carcinoma, the five-year cure rate exceeds 95% with Mohs surgery. Squamous cell carcinoma has a slightly higher risk of recurrence and spread but still offers good survival with prompt intervention.
Sebaceous gland carcinoma carries a more guarded prognosis due to delayed diagnosis and its potential for microscopic spread. Early excision with clear margins and lymph node evaluation improves survival outcomes. Eyelid melanoma, though rare, behaves similarly to melanoma elsewhere on the body and depends on thickness, ulceration, and mitotic rate.
Prognosis also depends on patient factors such as age, immune status, and adherence to follow-up care. Prompt detection and multidisciplinary treatment remain the strongest predictors of long-term disease-free survival.
Psychological Impact and Cosmetic Concerns
Beyond the clinical aspects of treatment, many patients experience significant emotional and psychological effects due to visible facial changes. The eyes are a central feature in social interaction, and deformities or scarring — even if medically necessary — can alter self-esteem, confidence, and interpersonal comfort.
Body image disturbance is especially common in younger patients or individuals in public-facing professions. Feelings of embarrassment, anxiety, or withdrawal can surface during recovery. For this reason, counseling and mental health support should be offered from the start, particularly in cases requiring disfiguring or staged reconstructions.
Aesthetic revision surgery is sometimes pursued not out of necessity, but to help the patient reclaim control and feel whole again. This patient-centered philosophy is shared across many areas of oncology — including prostate cancer survivorship, as detailed in our article on pi-rads 4 prostate cancer survival rate — where quality of life becomes just as important as clinical cure.
Prevention and Sun Protection Strategies
The most effective strategy against lower eyelid cancer is prevention, especially since the majority of cases are linked to cumulative ultraviolet (UV) exposure. The delicate skin of the eyelids is particularly vulnerable to sun damage, yet it’s often neglected when applying sunscreen. Daily use of broad-spectrum SPF 30+ sunscreen on the entire face, including the periocular region, is essential even on cloudy days or during winter.
UV-protective sunglasses offer a dual benefit: they shield the eyelids from direct sunlight and reduce ocular damage. Wide-brimmed hats further reduce facial exposure and should be part of routine outdoor wear. Patients with previous eyelid cancer should be particularly diligent, as recurrence or new primary lesions can appear in adjacent sun-damaged skin.
Sun avoidance during peak hours (10 a.m. to 4 p.m.) and the use of mineral sunscreens with zinc oxide or titanium dioxide are especially helpful around the eyes, where chemical sunscreens may irritate. Just as regular skin checks are standard for melanoma survivors, eyelid cancer patients should practice lifelong photoprotection.
Global Perspectives on Lower Eyelid Cancer Care
Access to specialized care for eyelid malignancies varies widely across countries and healthcare systems. In high-resource regions, patients typically receive multidisciplinary evaluation including oculoplastic surgery, dermatopathology, and radiation oncology input. Advanced imaging, Mohs surgery, and reconstructive expertise are readily available.
Conversely, in lower-resource settings, diagnosis may rely on clinical observation without imaging or histological confirmation. Standard excision with variable margins is more common, and reconstructive techniques may be limited. This leads to increased rates of incomplete excision, delayed recovery, and suboptimal cosmetic outcomes.
Global collaboration is needed to address these disparities, particularly in training general practitioners and ophthalmologists to recognize suspicious lesions early. Educational campaigns promoting sun protection and early detection — similar to those used in campaigns for breast or prostate cancer awareness — can play a transformative role in low- and middle-income countries.
Innovations in Reconstructive Techniques
Reconstructive surgery has evolved dramatically, with techniques now focused on both restoring function and preserving natural appearance. For small to moderate defects, advancement or rotational flaps offer excellent contour match. For more extensive resections, full-thickness grafts or tarsoconjunctival flaps may be used to rebuild the posterior lamella and eyelid margin.
Recent innovations include the use of bioengineered skin scaffolds and amniotic membrane grafts to accelerate healing and minimize scarring. 3D surgical planning is also emerging, particularly in tertiary care centers, to optimize flap orientation and predict postoperative results.
These advances mirror progress in other fields of cancer care where the focus has shifted toward organ-sparing, function-preserving strategies. The same principle underlies treatments for gynecologic malignancies like ovarian cancer, where staging and resection are carefully planned to minimize impact on fertility and quality of life.
Vigilance, Precision, and Patient-Centered Care
Lower eyelid cancer, though often subtle in presentation, demands a high index of suspicion and timely, multidisciplinary management. Early symptoms can be dismissed as benign, but when recognized promptly and treated with precision, outcomes are excellent — both in terms of survival and cosmetic preservation.
With proper staging, surgical planning, and reconstructive foresight, patients can retain eyelid function and appearance without compromising oncologic control. Long-term success depends not only on technical excellence but on patient education, follow-up, and emotional support.
As with other cancers — whether prostate, ovarian, or skin-based — the most powerful tools remain awareness, early diagnosis, and tailored treatment. Lower eyelid cancer reminds us that small changes on the surface may point to serious pathology underneath, and acting early makes all the difference.
FAQ
What are the first signs of lower eyelid cancer?
The most common early signs include a persistent lump, redness, or lesion on the eyelid that doesn’t resolve with time. Loss of eyelashes, skin thickening, or an ulcer that bleeds or doesn’t heal should also raise concern. Any lesion lasting more than a few weeks should be evaluated.
Is lower eyelid cancer dangerous?
Yes, although many types such as basal cell carcinoma grow slowly and rarely metastasize, others like sebaceous gland carcinoma or melanoma can be aggressive and spread beyond the eyelid. Early detection significantly improves outcomes and lowers the risk of serious complications.
How is lower eyelid cancer diagnosed?
Diagnosis begins with a clinical examination and is confirmed through a biopsy. In some cases, imaging such as MRI or CT scans may be used to assess the extent of tumor invasion or rule out lymph node involvement. Pathology determines the cancer type and guides treatment planning.
Can lower eyelid cancer spread to the brain?
It’s rare but possible, particularly in advanced or aggressive subtypes like melanoma or squamous cell carcinoma. Most eyelid cancers remain localized if treated early, but deep orbital invasion can increase the risk of spread to nearby structures, including intracranial tissues.
What is the survival rate for lower eyelid cancer?
When detected and treated early, survival rates are excellent — often exceeding 95% for basal cell carcinoma. More aggressive types like sebaceous gland carcinoma or melanoma have lower survival, especially if diagnosed late or not fully excised.
Can it come back after treatment?
Yes, recurrence is possible, especially in high-risk subtypes or when margins are not fully clear. Regular follow-up and skin checks are crucial to detect recurrence early and address it promptly. Mohs surgery helps reduce recurrence by ensuring complete tumor removal.
What is Mohs surgery and why is it used for eyelid cancer?
Mohs micrographic surgery is a technique that removes cancer layer by layer while checking each layer under a microscope. It’s ideal for the eyelid because it maximizes tissue preservation and minimizes scarring, while ensuring complete tumor clearance.
Will I be disfigured after eyelid cancer surgery?
Modern reconstructive techniques allow most patients to heal with excellent cosmetic and functional outcomes. In some cases, a temporary change in eyelid shape or appearance may occur, but revision procedures are available if needed.
How long is recovery after surgery?
Recovery depends on the size and complexity of the surgery. Minor procedures heal in about 1–2 weeks, while extensive reconstruction may require several weeks and follow-up adjustments. Most patients resume normal activities within a few weeks post-op.
Do I need radiation therapy?
Radiation is typically reserved for cases where surgery isn’t possible, where margins are positive after excision, or when the tumor is recurrent or very aggressive. Your care team will determine if radiation is appropriate based on pathology and stage.
Can microcurrent or cosmetic treatments cause or worsen eyelid cancer?
There’s no direct evidence linking microcurrent therapy to eyelid cancer, but any stimulation of periorbital tissue should be approached cautiously, especially after cancer treatment. Consult your doctor before using such devices postoperatively or during monitoring.
Is sebaceous gland carcinoma really that serious?
Yes, it is one of the most aggressive eyelid cancers. It can mimic benign conditions like chalazion, leading to delayed diagnosis. It also has a higher risk of spreading to lymph nodes and requires careful excision and follow-up.
Should I avoid sun exposure after eyelid cancer?
Absolutely. UV radiation is a major risk factor for skin cancers. Protect your eyelids with sunglasses, hats, and broad-spectrum sunscreen. Ongoing sun protection is key to preventing recurrence or new lesions.
Can children get eyelid cancer?
Eyelid cancer is extremely rare in children. When it does occur, it’s often due to genetic predisposition or immunosuppression. Most cases affect older adults, particularly those with fair skin and chronic sun exposure.
What should I do if I suspect a lesion might be cancerous?
Schedule an appointment with a dermatologist or ophthalmologist as soon as possible. Do not try to self-treat or assume it’s benign. A biopsy is the only definitive way to diagnose or rule out cancer.













