Living With Acid Reflux: Prevention and Proven Treatment Options
What Is Acid Reflux and GERD
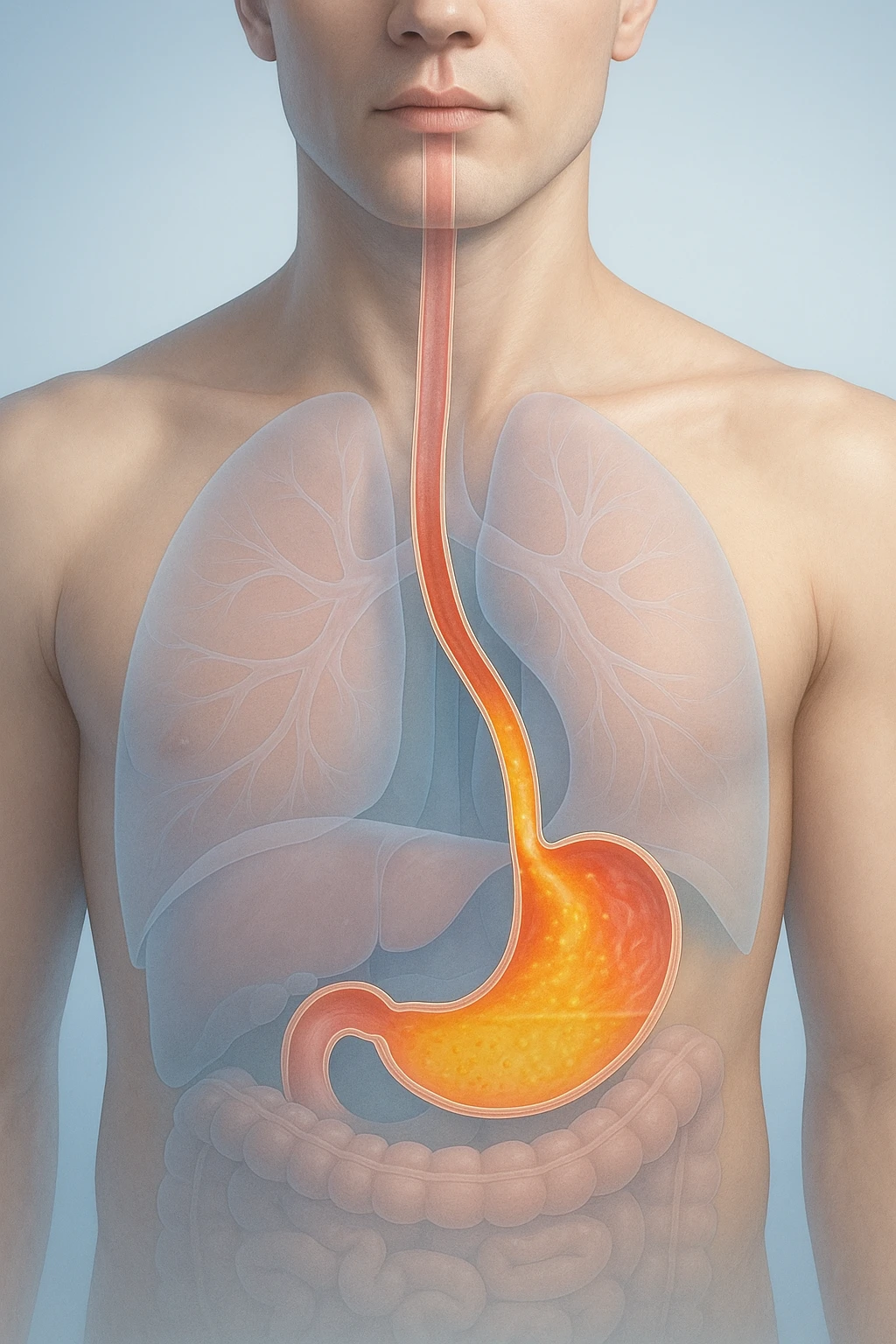
Acid reflux occurs when stomach contents flow backward into the esophagus, the tube connecting the mouth and stomach. This backward flow, or reflux, happens when the natural barrier that keeps acid in the stomach does not function properly. While occasional reflux is common and often harmless, frequent or persistent episodes can lead to a chronic condition called gastroesophageal reflux disease (GERD).
GERD is a long-term digestive disorder that develops when acid reflux causes repeated irritation or inflammation of the esophagus. It results from a breakdown of the normal anti-reflux barrier located at the junction between the esophagus and the stomach. Over time, this failure of the barrier can lead to symptoms that interfere with daily life and, in some cases, complications if left unmanaged. Despite its prevalence, GERD is highly treatable with lifestyle changes, medications, or other medical approaches.
Definition and Mechanism
Under normal circumstances, a ring of muscle known as the lower esophageal sphincter acts like a valve, tightening after food passes into the stomach to prevent contents from moving upward. In people with acid reflux or GERD, this sphincter may relax inappropriately or lose strength, allowing acidic material to escape into the esophagus. Because the lining of the esophagus is not designed to handle acid, this contact causes irritation and the familiar burning sensation known as heartburn.
Repeated exposure to acid can inflame the esophageal lining and lead to discomfort or more persistent damage. The severity and frequency of reflux vary among individuals, depending on factors such as body weight, meal patterns, and sphincter strength.
GERD vs. Occasional Heartburn
Many people experience occasional heartburn, especially after large or spicy meals. This isolated symptom does not necessarily indicate GERD. The condition is diagnosed when reflux episodes occur frequently enough to cause troublesome symptoms or when they lead to visible injury in the esophagus. In GERD, the reflux process tends to be recurrent and relapsing, with symptoms that may worsen over time if untreated.
GERD is a very common condition worldwide and can significantly affect quality of life, particularly in regions with high dietary and lifestyle risk factors. Recognizing that GERD is both manageable and common can help patients seek timely medical evaluation and effective treatment to protect esophageal health.
Causes and Risk Factors of Acid Reflux
Acid reflux usually results from a combination of physiological and lifestyle factors that allow stomach acid to escape into the esophagus. Understanding these mechanisms helps explain why some people experience reflux more frequently and highlights which factors can be modified to reduce symptoms.
Physiological Causes
The main physical cause of acid reflux is dysfunction of the lower esophageal sphincter, a muscular ring between the esophagus and stomach. Normally, it stays closed except when swallowing, acting as a barrier that keeps stomach contents in place. When its tone weakens or it relaxes inappropriately, acid and partially digested food can move upward, irritating the esophagus and causing heartburn.
A hiatal hernia can worsen reflux by allowing part of the stomach to move upward through the diaphragm, reducing the diaphragm’s support for the sphincter. This makes it easier for stomach acid to reach the esophagus and contributes to more frequent or severe symptoms. Both sphincter dysfunction and hiatal hernia disrupt the body’s natural anti-reflux barrier, promoting persistent reflux episodes.

Lifestyle and Environmental Factors
Certain habits and external conditions can increase reflux risk by raising abdominal pressure or slowing digestion. Obesity is one of the strongest known risk factors, as excess abdominal weight increases pressure that promotes backflow of stomach contents. Pregnancy can have a similar effect, especially in later stages.
- Medications that relax smooth muscle or slow digestion
- Smoking and alcohol consumption
- Large or high-fat meals
- Eating close to bedtime or lying down soon after meals
These factors can further weaken the sphincter or delay stomach emptying. Recognizing and modifying these risks can significantly reduce reflux frequency and intensity.
Recognizing and Diagnosing Acid Reflux
Identifying acid reflux and distinguishing it from other digestive or cardiac conditions requires recognizing its characteristic symptoms and understanding how physicians confirm the diagnosis. While many cases are straightforward, others need additional evaluation to rule out complications or overlapping disorders.
Common and Atypical Symptoms
The hallmark symptoms of GERD are heartburn and acid regurgitation. Heartburn describes a burning sensation behind the breastbone that may rise toward the throat, while regurgitation refers to sour-tasting fluid moving upward from the stomach into the mouth or throat. These symptoms often worsen after eating or when lying down and may improve temporarily with antacids.
- Typical symptoms: Heartburn and acid regurgitation, often after meals or when lying down.
- Atypical symptoms: Chest pain not related to the heart, difficulty swallowing (dysphagia), chronic cough, or persistent sore throat.
Because these symptoms can mimic other conditions such as asthma, sinus disease, or heart problems, medical evaluation is important to confirm whether reflux is the true cause.
Red Flags
- Trouble or pain when swallowing
- Unintentional weight loss
- Vomiting blood
- Black or tarry stools indicating possible gastrointestinal bleeding
These warning signs may suggest complications and require prompt medical attention.
Diagnostic Approach
In adults with typical reflux symptoms and no alarm features, physicians often begin with an empiric trial of acid-suppressing medication. A once-daily proton pump inhibitor (PPI) taken for about eight weeks serves both diagnostic and therapeutic purposes-symptom improvement supports the diagnosis of GERD.
When symptoms persist despite treatment, or when alarm features are present, further diagnostic testing may include:
- Upper endoscopy: To identify inflammation, ulcers, or Barrett’s esophagus.
- Ambulatory pH monitoring: To measure acid exposure in the esophagus.
- Esophageal manometry: To assess muscle function before surgical consideration.
These tests help distinguish GERD from other causes of upper digestive symptoms and guide individualized treatment plans.

Evidence-Based Treatments for Acid Reflux
Treatment for acid reflux or GERD focuses on reducing acid backflow and healing irritation in the esophagus. Management is tailored to symptom severity, response to therapy, and underlying factors. Most patients achieve relief with medication and lifestyle changes, while others may require procedural or surgical options if symptoms persist.
Medication Options
Proton pump inhibitors (PPIs) are the mainstay of GERD treatment and are most effective for healing erosive esophagitis and controlling symptoms. They reduce stomach acid production and are typically taken before meals. For milder or occasional symptoms, other medications may provide relief:
- Proton pump inhibitors (PPIs): Most effective for healing and symptom control.
- Histamine-2 receptor antagonists (H2 blockers): Helpful for milder, intermittent cases.
- Antacids and alginate-based formulations: Provide rapid, short-term relief for occasional heartburn.
Medication plans are individualized, balancing symptom control with the lowest effective long-term dose.
Lifestyle and Behavioral Strategies
Non-drug measures are key for symptom management and prevention of recurrence. Weight reduction consistently improves reflux symptoms, as excess abdominal pressure promotes acid backflow. Elevating the head of the bed can reduce nighttime reflux by using gravity to keep stomach contents in place.
- Maintain a healthy weight to reduce abdominal pressure.
- Elevate the head of the bed to lessen nighttime reflux.
- Avoid large or late meals and identify individual food triggers.
These strategies are most effective when maintained long-term alongside medical treatment.
Procedural and Surgical Interventions
When symptoms persist despite optimized medical therapy, physicians may recommend further evaluation to confirm ongoing reflux and rule out other causes. This includes checking medication adherence and, if needed, using reflux monitoring tests.
- Laparoscopic fundoplication: Reinforces the lower esophageal sphincter to prevent reflux.
- Magnetic sphincter augmentation: A less invasive device-based alternative.
- Endoscopic therapies: Used in selected patients to improve sphincter function.
These interventions are reserved for patients with persistent or PPI-dependent symptoms after comprehensive evaluation.

Long-term GERD management involves regular follow-up to ensure continued symptom control and therapy adjustment. With evidence-based care and consistent monitoring, most individuals can maintain digestive health and minimize reflux impact.
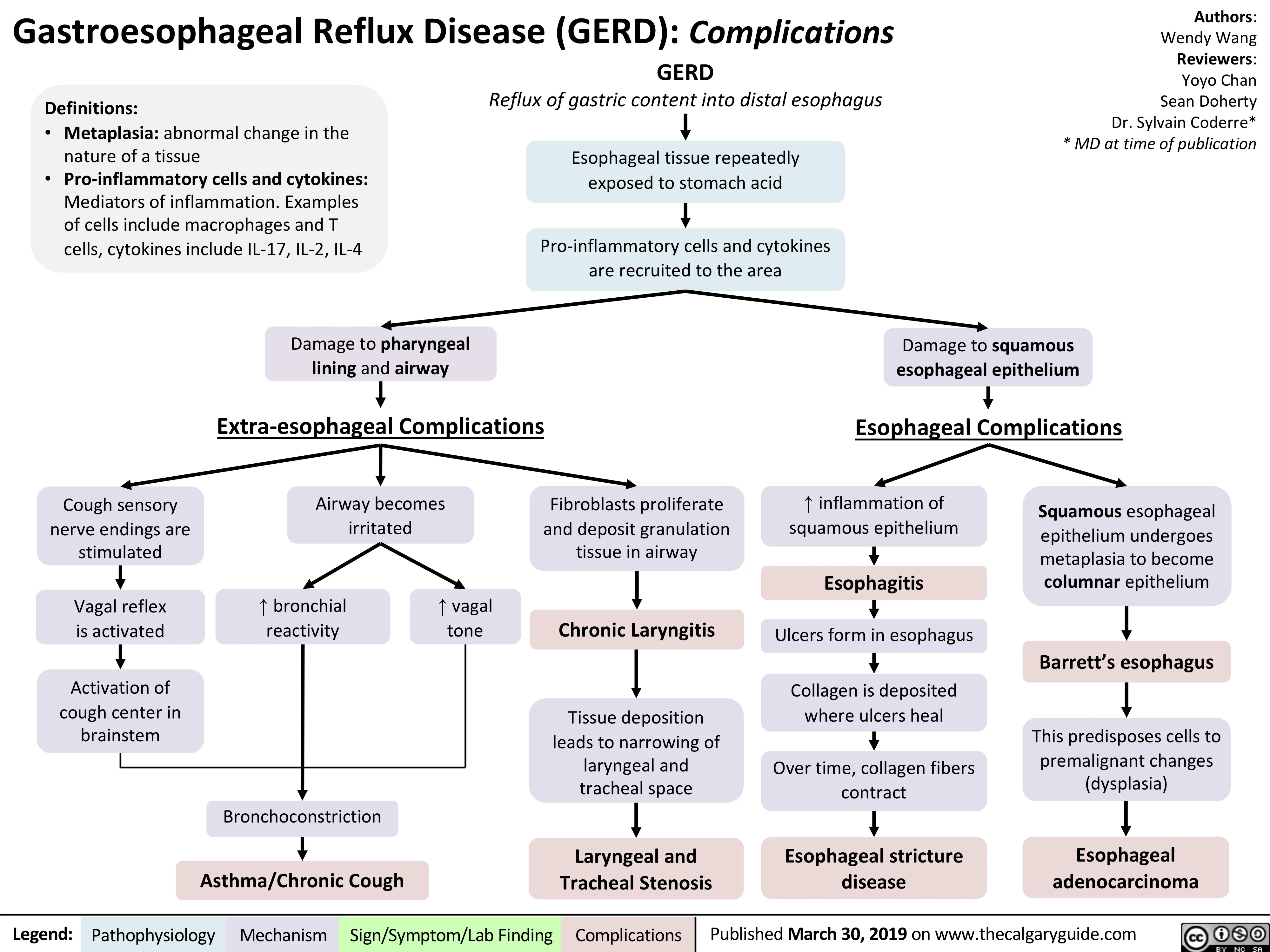
Complications, Prognosis, and Living Well with Acid Reflux
Most people with acid reflux can achieve long-term relief and prevent complications through proper treatment and lifestyle management. However, when reflux remains uncontrolled for extended periods, it can damage the lining of the esophagus and lead to more serious health problems. Understanding these risks underscores the importance of consistent management and regular medical follow-up.
Complications and Long-Term Outlook
Chronic, untreated reflux may cause inflammation of the esophageal lining, known as erosive esophagitis. Over time, repeated acid exposure can result in painful ulcers or the formation of peptic strictures-narrowed sections of the esophagus that make swallowing difficult. In a small proportion of patients, long-standing GERD can lead to changes in the esophageal lining called Barrett’s esophagus, which carries a higher risk of developing esophageal cancer. Although this progression is uncommon, it highlights why persistent symptoms should not be ignored.
- Erosive esophagitis: Inflammation and irritation of the esophageal lining.
- Esophageal ulcers: Painful sores caused by prolonged acid exposure.
- Peptic strictures: Narrowing of the esophagus due to scarring, making swallowing difficult.
- Barrett’s esophagus: Long-term change in the esophageal lining that increases cancer risk.
With early recognition and evidence-based treatment, most individuals maintain good digestive health and avoid complications. Patients with Barrett’s esophagus or severe disease require structured, long-term follow-up to monitor for changes and ensure continued symptom control. For the majority, a combination of medication, weight management, and lifestyle adjustments is sufficient to achieve lasting relief and preserve esophageal health.
When to See a Doctor
Seek medical evaluation if heartburn or regurgitation occurs frequently despite treatment, or if you develop any of the following warning signs:
- Difficulty or pain when swallowing
- Unexplained weight loss
- Vomiting blood or passing black stools
- Persistent chest pain not related to heart disease
Prompt assessment allows early intervention, reducing the risk of long-term complications from acid reflux or GERD.
Living Well with GERD
Managing acid reflux effectively involves more than medication. Simple, sustainable habits can make a significant difference in comfort and quality of life. Eating smaller, balanced meals, maintaining a healthy weight, and avoiding lying down soon after eating can help limit reflux episodes. Elevating the head of the bed, reducing alcohol and tobacco use, and identifying personal food triggers further support symptom control.
- Eat smaller, balanced meals and avoid lying down after eating.
- Maintain a healthy weight to reduce abdominal pressure.
- Elevate the head of the bed to prevent nighttime reflux.
- Limit alcohol and tobacco use.
- Identify and avoid specific food triggers.
With consistent care, most patients find their symptoms become predictable and manageable. Regular communication with healthcare providers ensures treatment remains effective over time and allows timely adjustments if symptoms return or change. Living well with GERD is achievable for nearly everyone when medical therapy and practical self-care work hand in hand.
Frequently Asked Questions About Acid Reflux
- Is acid reflux the same as GERD?
- Not always. Acid reflux describes occasional backflow of stomach contents, while GERD is a chronic form that causes frequent or persistent symptoms.
- Can acid reflux cause chest pain?
- Yes. Reflux can trigger burning or pressure in the chest known as heartburn, but chest pain should always be evaluated to rule out heart-related causes.
- What foods commonly trigger acid reflux?
- Spicy, fried, and fatty foods, along with chocolate, caffeine, citrus, and alcohol, may worsen symptoms in some people. Triggers vary by individual.
- Does stress make acid reflux worse?
- Stress does not directly cause reflux, but it can increase awareness of symptoms or influence habits such as eating quickly or consuming trigger foods.
- How is acid reflux diagnosed by doctors?
- Most diagnoses are based on symptoms and response to acid-suppressing medication. Persistent or complex cases may need endoscopy or pH monitoring.
- Can you have acid reflux without heartburn?
- Yes. Some people experience throat irritation, chronic cough, or a sour taste without classic heartburn. This is sometimes called silent reflux.
- Is long-term acid reflux dangerous?
- Chronic untreated reflux can lead to esophagitis, ulcers, strictures, or Barrett’s esophagus, which slightly increases the risk of esophageal cancer.
- What lifestyle habits help reduce reflux?
- Maintaining a healthy weight, avoiding large meals or late-night eating, and elevating the head of the bed can greatly lessen reflux episodes.
- Do over-the-counter medicines help acid reflux?
- Antacids and H2 blockers can relieve mild, occasional reflux. Persistent symptoms may require prescription-strength proton pump inhibitors under medical guidance.
- When should someone see a doctor for acid reflux?
- Seek medical advice if reflux occurs frequently, disrupts sleep, or is accompanied by warning signs like trouble swallowing, bleeding, or weight loss.