Irregular Periods in Pituitary Tumors
Irregular Periods in Pituitary Tumors: Medical Insights and Management
- How Pituitary Tumors Affect the Menstrual Cycle
- Understanding the Mechanism: Hormonal Disruption at the Source
- How Often Does It Occur in Pituitary Tumor Patients?
- Clinical Observations and Staging Correlations
- Why These Changes Happen: Causes Behind Irregular Periods in Pituitary Tumors
- When You Should Be Concerned: Signs Not to Ignore
- How Doctors Diagnose the Cause
- How to Manage the Symptom: Relieving Irregular Periods
- Can This Be Prevented in High-Risk Patients?
- Do Irregular Periods Resolve Over Time or Persist?
- What Experts Say: Insights from Oncologists and Endocrinologists
- 15+ Questions to Ask Your Doctor
How Pituitary Tumors Affect the Menstrual Cycle
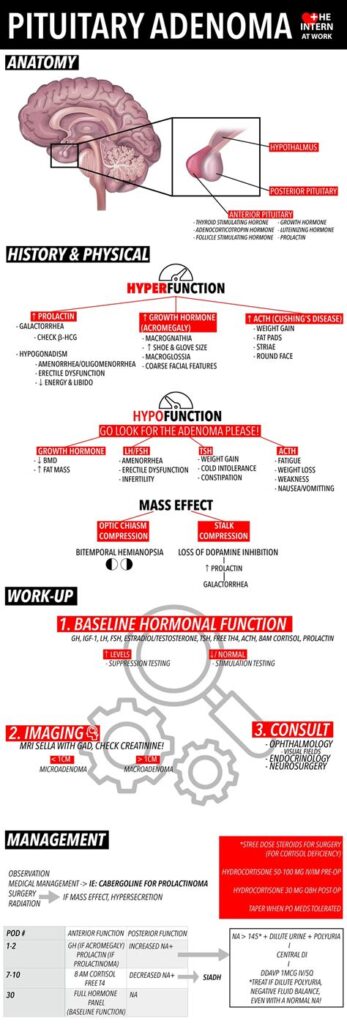
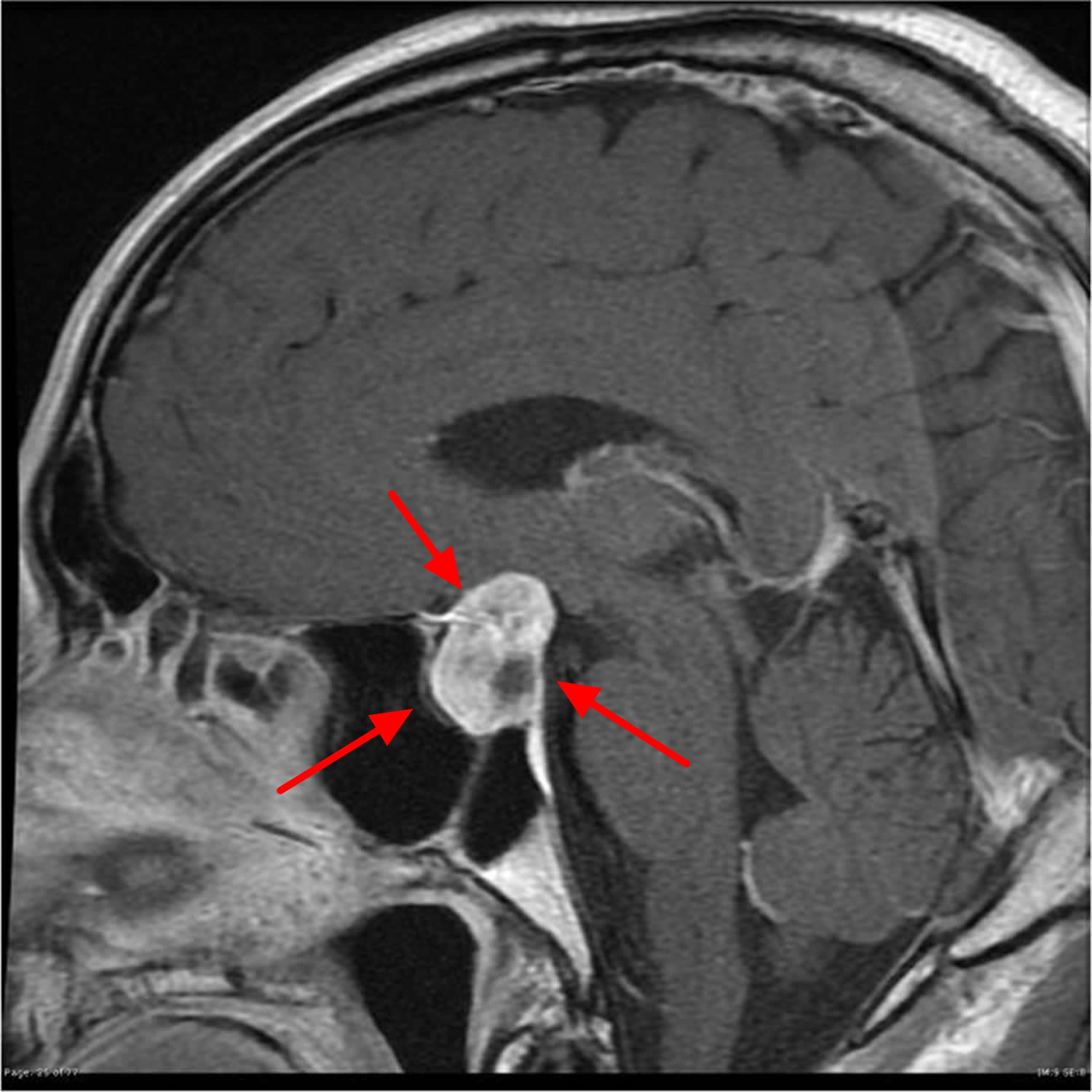
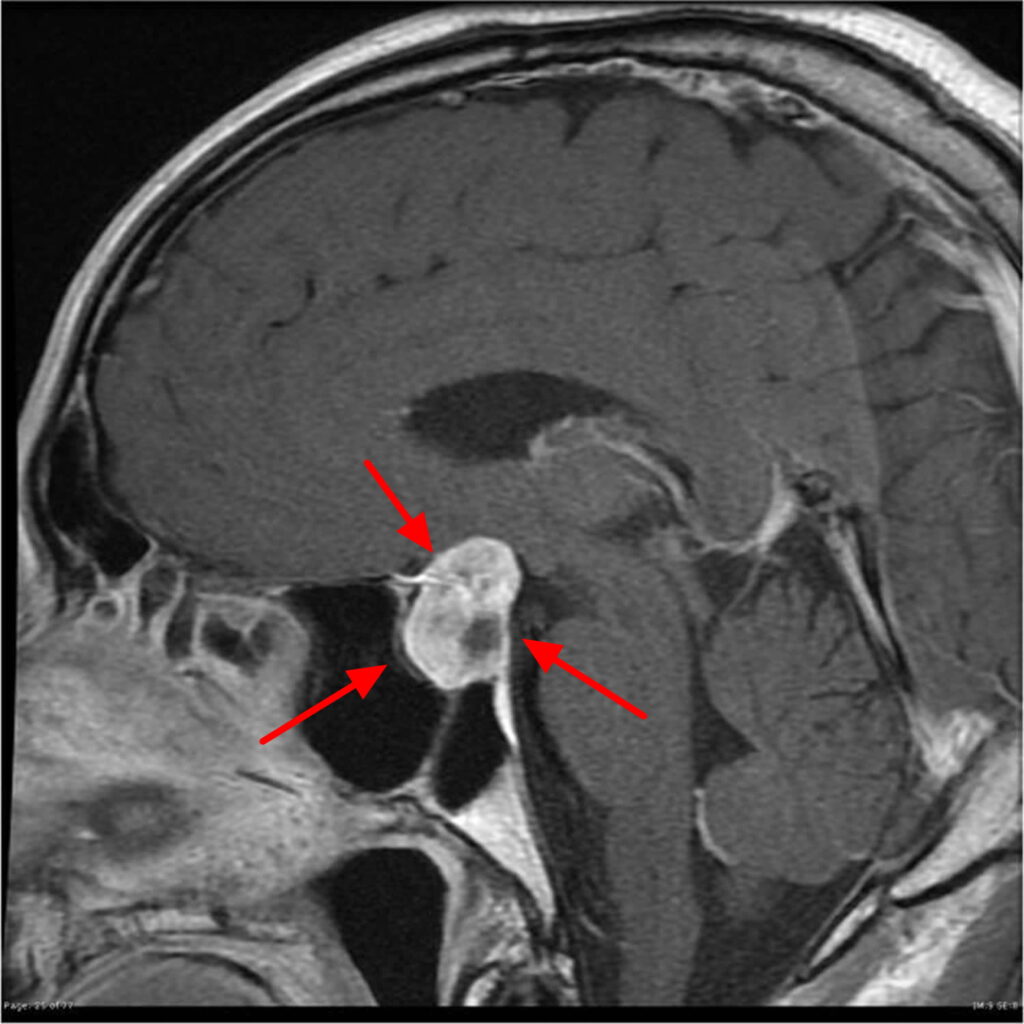
Pituitary tumors can interfere with the body’s hormonal balance, particularly affecting the menstrual cycle. These tumors, usually benign adenomas, develop in the pituitary gland, a small but crucial endocrine organ located at the base of the brain. It regulates multiple hormones, including those responsible for ovulation and menstruation—like luteinizing hormone (LH), follicle-stimulating hormone (FSH), and prolactin.
When a pituitary tumor alters the secretion of these hormones, it can cause irregular, delayed, or even absent menstrual periods (amenorrhea). In some women, this may be one of the earliest signs of pituitary dysfunction, especially if paired with symptoms like galactorrhea (unexpected milk production), fatigue, or vision changes. The menstrual disruption may resemble the irregularities observed in conditions like PCOS or early menopause, but the underlying endocrine origin sets pituitary tumors apart.
Understanding the Mechanism: Hormonal Disruption at the Source
The pituitary gland acts as a hormonal control center. When a tumor grows in this region, it can secrete excess prolactin (prolactinoma) or compress normal pituitary tissue, leading to underproduction of gonadotropins. Elevated prolactin suppresses the hypothalamic release of GnRH (gonadotropin-releasing hormone), which in turn suppresses LH and FSH. The result is a disrupted ovarian cycle.
Additionally, if the tumor impairs thyroid-stimulating hormone (TSH) or adrenocorticotropic hormone (ACTH) levels, this broader hormonal imbalance can further compound menstrual irregularities. This mechanism is especially relevant in Cancer Tumor Markers analysis, where hormonal feedback loops are assessed for tumor activity.
How Often Does It Occur in Pituitary Tumor Patients?
Menstrual irregularities are reported in over 75% of women with functioning pituitary adenomas, especially prolactinomas. Non-functioning tumors may also cause menstrual disturbances due to pressure on normal pituitary tissue, though at a slightly lower frequency.
In women with macroadenomas (tumors larger than 10 mm), menstrual disruption is more common due to the tumor’s mass effect. Microadenomas may also cause changes but are often discovered earlier due to the hormonal symptoms. Age, tumor type, and tumor activity (hormone-secreting or non-functional) all influence the frequency of menstrual impact.
Clinical studies show that Cancer patients undergoing cranial radiation or long-term corticosteroid therapy may also experience secondary pituitary dysfunction, adding another layer of menstrual instability, especially in cases where cancer treatments overlap with endocrine pathways.
Clinical Observations and Staging Correlations
From a clinical standpoint, irregular menstruation tends to correlate with both tumor size and hormone type. In women with large prolactin-secreting tumors, amenorrhea is the dominant presentation. In contrast, tumors causing panhypopituitarism may lead to complex menstrual suppression alongside fatigue, low libido, and metabolic slowing.
The staging of the tumor (size and local invasion) influences the symptom profile. Pituitary tumors are not staged like Fungating Breast Tumors or systemic cancers, but classification into microadenomas vs. macroadenomas or invasive vs. non-invasive forms helps guide prognosis and treatment.
A study from the Journal of Clinical Endocrinology and Metabolism found that restoration of menses occurred in 65% of women treated successfully for microadenomas and only 38% of those with macroadenomas, highlighting the importance of early detection.
Why These Changes Happen: Causes Behind Irregular Periods in Pituitary Tumors
The hormonal imbalance caused by pituitary tumors is the central mechanism behind irregular periods. These tumors can be either hormone-secreting or non-functional, each leading to menstrual disruption in different ways:
| Type of Tumor | Hormonal Impact | Menstrual Effect |
| Prolactinoma | Overproduction of prolactin | Inhibits LH/FSH → amenorrhea |
| Non-functioning adenoma | Compression of normal pituitary tissue | Reduces all pituitary hormones |
| ACTH-secreting tumor | Increases cortisol (Cushing’s disease) | Secondary suppression of gonadotropins |
| TSH-secreting tumor | Affects thyroid hormones | Indirect disruption of cycle |
Additional causes include:
- Medication-related effects: Dopamine antagonists and high-dose steroids used in cancer therapy can elevate prolactin levels.
- Radiation damage: Radiation to the brain or pituitary region in cancers like gliomas or nasopharyngeal tumors can impair the hypothalamic-pituitary axis.
- Systemic illness: Severe illness or malnutrition caused by Cancer may lead to hypothalamic suppression and disrupt ovulatory signals.
In some cases, hormone production may be partially retained, leading to sporadic bleeding, unpredictable cycles, or breakthrough spotting rather than full amenorrhea.
When You Should Be Concerned: Signs Not to Ignore
Not every missed or irregular period is alarming—but in the context of known or suspected pituitary involvement, several red flags warrant urgent attention:
- Sudden loss of menstruation for more than 3 months
- Galactorrhea in non-lactating women
- Visual disturbances (especially peripheral vision loss)
- Frequent headaches or sudden changes in headache pattern
- Fatigue, cold intolerance, or unexplained weight gain
- Signs of adrenal crisis (nausea, hypotension, dizziness)
These may indicate growing mass effect or hormonal collapse. In such cases, evaluation for tumor enlargement, pituitary apoplexy, or evolving hypopituitarism becomes crucial. Early medical attention can prevent severe outcomes like vision loss or adrenal failure.
How Doctors Diagnose the Cause
Diagnosis of menstrual irregularity due to pituitary tumor involves both hormone testing and imaging:
| Diagnostic Tool | Purpose |
| Serum Prolactin | To identify hyperprolactinemia |
| LH, FSH, Estradiol | Evaluate ovarian function and pituitary signaling |
| TSH, Free T4 | Assess thyroid status (can mimic menstrual irregularity) |
| ACTH, Cortisol | Rule out adrenal insufficiency or Cushing’s syndrome |
| MRI of the pituitary | Visualize tumor size, shape, and local invasion |
| Visual field testing | Check for optic chiasm compression |
If imaging confirms a pituitary lesion and labs reveal hormonal disruption, a diagnosis of pituitary adenoma with menstrual impact is made. Some patients may require additional endocrine stimulation tests to clarify the level of dysfunction.
How to Manage the Symptom: Relieving Irregular Periods
Treatment is based on the tumor’s type, size, and effect on hormone levels. Medical therapy is often the first-line approach for prolactinomas:
| Treatment Option | Mechanism / Goal |
| Dopamine agonists (e.g., cabergoline) | Lowers prolactin → restores ovulation |
| Hormone replacement therapy | Corrects estrogen/progesterone imbalance |
| Transsphenoidal surgery | Removes macroadenomas causing mass effect |
| Radiotherapy | Used for residual or recurrent tumor |
| Stress reduction / nutritional support | Supports hypothalamic function |
Multidisciplinary consultation—often involving endocrinology, neurosurgery, and gynecology—is crucial. In some cases, Cancer Tumor Markers and systemic cancer status also influence treatment decisions, especially if the patient is undergoing broader oncologic care.
Can This Be Prevented in High-Risk Patients?
Preventing irregular periods related to pituitary tumors hinges on early detection and management of the underlying tumor or its hormonal consequences. While you cannot always prevent the development of a pituitary tumor, especially if it’s spontaneous or genetically predisposed (e.g., MEN1 syndrome), some steps can minimize progression or symptom severity:
| Preventive Focus | Approach |
| Routine hormone screening | Especially in patients with visual symptoms or galactorrhea |
| MRI follow-up for known lesions | Timely imaging tracks tumor growth before symptoms emerge |
| Managing comorbid endocrine issues | Address thyroid/adrenal abnormalities promptly |
| Medication side effect monitoring | Adjust drugs that impact dopamine or hormone regulation |
| Lifestyle management | Adequate sleep, stress control, and nutrition support brain-pituitary health |
In women undergoing treatment for Cancer, especially those receiving cranial radiation or steroids, preventive monitoring of menstrual cycles and hormonal labs is advisable. This can identify disruption early and help preserve reproductive health.
Do Irregular Periods Resolve Over Time or Persist?
Whether irregular periods resolve depends on the tumor’s type, treatment effectiveness, and overall health of the hypothalamic-pituitary-ovarian axis.
| Scenario | Likelihood of Recovery |
| Microprolactinomas treated with dopamine agonists | High likelihood of menstrual normalization |
| Large macroadenomas with compression | May recover if treated early; delays can cause permanent loss |
| Post-radiation hypopituitarism | Often permanent; requires hormone replacement |
| Functional tumors in remission | Partial or full recovery possible with stable hormone levels |
| Advanced Cancer or systemic illness | Often prolonged or persistent disruption |
Recovery of regular periods is not always the primary goal in cancer-related pituitary disorders but can be a meaningful marker of hormonal stabilization and overall wellness.
What Experts Say: Insights from Oncologists and Endocrinologists
Oncology-endocrinology collaboration is crucial in managing pituitary tumor-related menstrual issues. Here’s what practicing doctors emphasize:
- “In prolactinoma cases, 90% of women regain menstrual cycles within months of dopamine agonist therapy.”
- “Delayed diagnosis of non-functioning adenomas can result in complete anterior pituitary failure—timing is critical.”
- “In cancer patients, we closely monitor hormone axes if cranial radiation or checkpoint inhibitors are involved, as they can trigger hypophysitis.”
- “Menstrual irregularities should not be ignored—they’re often early signs of systemic dysfunction, even in non-gynecological cancers like Cancer.”
The consensus is that menstrual health offers a window into broader pituitary health and should be routinely assessed, especially in at-risk patients.
15+ Questions to Ask Your Doctor
1. Could my irregular periods be caused by a pituitary tumor or cancer-related treatment?
Ask for clarity on hormonal and imaging work-up.
2. What hormones will you test to evaluate my cycle issues?
Understanding lab plans helps you track your own progress.
3. Do I need an MRI scan of my pituitary gland?
This is a key step in confirming structural causes.
4. Can my medications be contributing to the problem?
Discuss all current drugs, including psychiatric or steroid use.
5. Is there a risk of permanent infertility from this?
Clarify prognosis, especially if you plan to conceive.
6. Will my periods return if the tumor is treated?
Recovery is case-dependent—your doctor can explain.
7. Do I need to see a reproductive endocrinologist or fertility specialist?
Useful in long-term treatment planning.
8. What are the risks if I delay treatment?
Some tumors can progress silently—early action matters.
9. Should I consider hormone replacement therapy?
This may be necessary if estrogen levels are persistently low.
10. How will we monitor changes in my hormonal levels over time?
Regular labs and follow-ups are vital.
11. Could this affect my thyroid or adrenal glands too?
Multiaxis dysfunction is common in pituitary disorders.
12. Are there lifestyle changes that can help restore balance?
Include questions about stress, sleep, and diet.
13. Can I still go through menopause naturally later on?
Important if you’re near perimenopausal age.
14. Are there clinical trials or newer treatments for pituitary tumors?
Stay informed about all possible options.
15. How does this tie into my overall cancer care plan?
Keep all your treatments integrated for the best outcomes.