Hyperthermia for Treating Breast Cancer in Dogs
- Understanding Canine Mammary Tumors
- The Science Behind Hyperthermia Therapy
- Types of Hyperthermia Treatments in Veterinary Oncology
- Benefits of Hyperthermia in Treating Canine Breast Cancer
- Preparing a Dog for Hyperthermia Treatment
- The Hyperthermia Procedure: Step-by-Step
- Combining Hyperthermia with Other Cancer Therapies
- Risks and Side Effects of Hyperthermia in Dogs
- Monitoring Progress During Hyperthermia Treatment
- Expected Outcomes and Prognosis
- Cost Considerations and Accessibility
- Post-Treatment Care and Quality of Life
- Case Studies: Successful Use of Hyperthermia in Dogs
- When Hyperthermia Is Not Recommended
- Current Research and Future Directions
- Owner Experiences and Testimonials
- Ethical Considerations in Cancer Treatment for Dogs
- Integrating Hyperthermia into Veterinary Oncology Practice
- Alternatives to Hyperthermia for Mammary Cancer in Dogs
- Long-Term Follow-Up and Monitoring
- FAQ

Understanding Canine Mammary Tumors
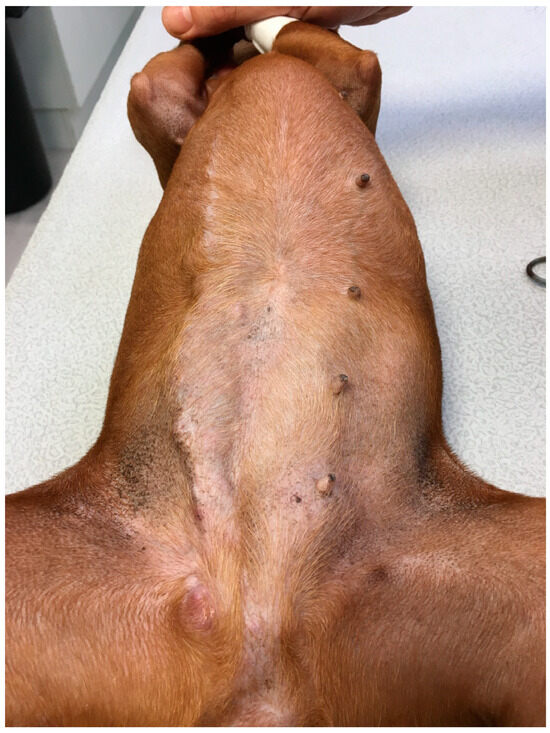
Canine mammary tumors are among the most prevalent neoplasms in female dogs, particularly those unspayed or spayed later in life. These tumors can be benign or malignant, with approximately 50% being malignant. Early detection and accurate diagnosis are crucial for effective treatment.
The development of mammary tumors is influenced by hormonal factors, especially estrogen and progesterone. Spaying a female dog before her first heat cycle significantly reduces the risk of developing these tumors. Obesity and certain breeds, such as Poodles, Spaniels, and Dachshunds, are also associated with a higher incidence.
Clinically, these tumors often present as palpable masses along the mammary chain. Diagnostic evaluation includes physical examination, imaging (such as ultrasound or mammography), and cytological or histopathological analysis through fine-needle aspiration or biopsy. Staging the tumor is essential to determine the extent of disease and guide treatment planning.
The Science Behind Hyperthermia Therapy
Hyperthermia therapy involves the controlled application of heat to tumor tissues, typically raising temperatures to 40–45°C. This elevation in temperature can directly damage cancer cells and enhance the effectiveness of other treatments like chemotherapy and radiation.
The biological rationale for hyperthermia includes increased tumor blood flow, improved oxygenation, and heightened sensitivity of cancer cells to other therapies. Additionally, hyperthermia can disrupt the repair mechanisms of cancer cells, leading to increased cell death.
Various methods are employed to deliver hyperthermia, including microwave, radiofrequency, ultrasound, and infrared energy. The choice of method depends on tumor location, size, and depth. Precise temperature monitoring is critical to ensure therapeutic efficacy while minimizing damage to surrounding healthy tissues.
Types of Hyperthermia Treatments in Veterinary Oncology
In veterinary oncology, hyperthermia treatments are categorized based on the area of application:
- Localized Hyperthermia: Targets a specific tumor site, suitable for superficial or accessible tumors.
- Regional Hyperthermia: Applies heat to a larger area or entire limb, often used when multiple tumors are present in a region.
- Whole-Body Hyperthermia: Involves raising the temperature of the entire body, considered for metastatic or systemic cancers.
Each approach requires careful consideration of the dog’s overall health, tumor characteristics, and treatment goals. Localized hyperthermia is commonly used for canine mammary tumors due to its precision and reduced systemic effects.

Benefits of Hyperthermia in Treating Canine Breast Cancer
Hyperthermia offers several advantages in managing canine breast cancer:
- Enhanced Treatment Efficacy: When combined with chemotherapy or radiation, hyperthermia can increase the sensitivity of cancer cells, leading to improved outcomes.
- Minimally Invasive: Hyperthermia is less invasive compared to surgical options, reducing recovery time and associated risks.
- Targeted Therapy: The ability to focus heat precisely minimizes damage to surrounding healthy tissues.
- Potential for Immune Activation: Heat can stimulate an immune response against tumor cells, contributing to systemic anti-cancer effects.
These benefits make hyperthermia a valuable component of a multimodal treatment strategy for canine breast cancer.
Preparing a Dog for Hyperthermia Treatment
Prior to initiating hyperthermia, a full diagnostic workup is essential to ensure the dog is a suitable candidate. This includes complete blood counts, biochemistry panels, thoracic imaging (to check for metastases), and abdominal ultrasound. Only after confirming localized disease or stable systemic involvement can hyperthermia be considered.
The dog must be in stable general health, with cardiac and respiratory systems able to tolerate sedation or anesthesia, which is commonly required for accurate positioning during treatment. Hydration status and electrolyte balance are also addressed before therapy.
Owner preparation is just as crucial. Veterinarians must explain potential side effects, the treatment schedule (usually requiring several sessions), and post-treatment care. Consent forms are signed, and logistical planning for multiple visits is arranged.
The Hyperthermia Procedure: Step-by-Step
The procedure itself is methodical and highly controlled. Here’s how a typical localized hyperthermia session proceeds:
| Step | Description |
| Patient Sedation | Light sedation or general anesthesia is induced to prevent movement and stress. |
| Positioning | The dog is carefully positioned for optimal access to the tumor area. |
| Device Calibration | Equipment is set to the correct parameters based on tumor depth and size. |
| Temperature Monitoring | Thermocouples or probes are placed in and around the tumor to monitor temperature in real time. |
| Heat Application | Heat is delivered using microwave, ultrasound, or radiofrequency energy. Target temperature is typically 42–43°C for 30–60 minutes. |
| Cooling Measures | Adjacent healthy tissues may be cooled simultaneously to avoid thermal damage. |
| Post-Treatment Check | The dog’s vitals are monitored during recovery, and the treatment area is inspected for skin changes or burns. |
Each session is usually repeated one to two times per week over several weeks, depending on the protocol.
Combining Hyperthermia with Other Cancer Therapies
One of the most powerful aspects of hyperthermia is its ability to enhance the effect of other treatments, particularly radiation therapy and chemotherapy.
When combined with radiation, hyperthermia can increase DNA damage in tumor cells by impairing their ability to repair after irradiation. This synergistic effect allows for lower doses of radiation, reducing the risk of side effects to nearby tissues.
In chemotherapy, hyperthermia improves drug delivery by increasing blood flow to the tumor and making cell membranes more permeable. It also reduces multidrug resistance in some tumors, making previously ineffective drugs more potent.
Careful scheduling is critical: hyperthermia is often applied within 30 to 60 minutes after radiation or chemotherapy for maximum synergy. Protocols are tailored to the tumor type, location, and dog’s health status.
Risks and Side Effects of Hyperthermia in Dogs
Despite its many benefits, hyperthermia therapy is not without risks. Most complications are mild and manageable but require close monitoring.
Local skin irritation or burns can occur if temperatures rise too high or aren’t distributed evenly. This is why precise thermal monitoring is essential during every session.
Pain or inflammation at the treatment site may be seen, especially in deeper tumors. Anti-inflammatory medications and mild analgesics are typically sufficient.
Fatigue and lethargy may appear post-session, particularly if sedation is used. These symptoms usually resolve within 12 to 24 hours.
Overheating of internal tissues, while rare, is a more serious concern and may require discontinuation of treatment. Veterinarians should always weigh risks against benefits based on tumor accessibility and patient condition.
Monitoring Progress During Hyperthermia Treatment
Continuous monitoring is essential to evaluate how well the dog is responding to hyperthermia. After each session, veterinarians assess tumor size, texture, and temperature response. Changes in blood flow or inflammation in the treatment zone may indicate early biological activity.
Follow-up imaging, such as ultrasound or thermography, helps determine the extent of tumor shrinkage or necrosis. For tumors treated in combination with chemotherapy or radiation, the full effect may take several weeks to manifest. Blood tests may also be repeated to monitor organ function and screen for systemic reactions.
In some cases, adjustments to the treatment plan are needed — either modifying the frequency, adjusting the thermal dose, or integrating additional modalities. The goal is to maximize therapeutic results while minimizing discomfort or adverse events.
Expected Outcomes and Prognosis
The success rate of hyperthermia in canine breast cancer largely depends on early diagnosis and the ability to treat localized tumors. When used as part of a multimodal approach — combining surgery, chemotherapy, and hyperthermia — the prognosis is significantly improved.
In benign or low-grade malignancies, complete remission is possible. Even in more aggressive tumors, hyperthermia can extend survival times and improve quality of life. For dogs with inoperable or metastatic disease, this technique provides valuable palliative benefits, such as pain relief and slowing tumor growth.
Veterinary case reports and limited clinical studies suggest that dogs treated with hyperthermia experience reduced tumor burden and fewer side effects compared to radiation alone. Still, every case is individual, and prognosis should be based on tumor stage, histology, and response to initial treatments.
Cost Considerations and Accessibility
Hyperthermia treatment, while promising, is not widely available at every veterinary clinic. Specialized oncology centers or university hospitals are typically equipped to offer this advanced modality. Costs can vary depending on geographic location, number of sessions, and whether it is combined with other treatments.
Owners should expect to pay between $500 and $1,500 per session, with full treatment plans potentially ranging from $3,000 to $10,000. This includes diagnostics, sedation, post-care monitoring, and any adjunct therapies.
Many clinics offer payment plans or work with third-party veterinary financing programs. While not inexpensive, the long-term value of hyperthermia lies in its ability to improve life expectancy and reduce invasive procedures. Discussing cost and options with the veterinary oncologist early on helps ensure realistic expectations.
Post-Treatment Care and Quality of Life
After each hyperthermia session, dogs require rest, hydration, and careful observation for skin or systemic reactions. Owners should monitor the treated area for signs of redness, swelling, or blistering and report any unusual behavior or appetite loss to the vet immediately.
Nutritional support is important during recovery, especially in dogs undergoing combined therapies. High-quality, anti-inflammatory diets and adequate hydration help maintain overall resilience. Physical activity is generally reduced during the treatment period, with a gradual return to normal walks and play after the final sessions.
Emotional well-being should not be overlooked. Comfort, companionship, and pain management contribute to maintaining a high quality of life. Most dogs tolerate the procedure well and adapt quickly between sessions. Veterinarians may schedule monthly follow-ups for the first six months to monitor remission or recurrence.
Case Studies: Successful Use of Hyperthermia in Dogs
Clinical case studies provide valuable insights into how hyperthermia performs in real-world settings. For example, a 9-year-old unspayed female Cocker Spaniel with a 2.5 cm mammary tumor underwent six sessions of localized hyperthermia combined with low-dose carboplatin chemotherapy. By the fifth session, the tumor had significantly shrunk, and surgical excision was performed with clean margins. No recurrence was observed after 12 months.
In another documented case, a senior Dachshund with multiple small mammary nodules not amenable to surgery was treated with hyperthermia alone. Over the course of ten sessions, the tumors stabilized in size, pain subsided, and the dog’s mobility and behavior improved dramatically. While not curative, the therapy extended the dog’s comfort phase by nearly a year.
Such case-based evidence, while anecdotal, helps establish realistic expectations and informs clinical decision-making. They also emphasize the importance of early detection and tailored treatment strategies for each patient.
When Hyperthermia Is Not Recommended
Despite its benefits, hyperthermia is not suitable for all canine breast cancer cases. Dogs with advanced systemic metastasis often require more aggressive or palliative care approaches. Whole-body hyperthermia may be theoretically useful, but it is rarely performed in veterinary medicine due to technical complexity and risk.
Dogs that are extremely aged, in poor body condition, or have comorbidities such as severe cardiac or renal disease may not tolerate sedation or thermal stress. Additionally, tumors located too deeply within the body, or with irregular shapes, may not receive uniform heating, which limits the effectiveness of the procedure.
Veterinarians must weigh these factors carefully and may recommend alternatives like oral chemotherapy, supportive care, or palliative surgery. The goal is always to preserve the animal’s quality of life and ensure that treatments do more good than harm.
Current Research and Future Directions
Veterinary oncologic hyperthermia is still considered an emerging field, but research is growing steadily. Studies are exploring the best combinations of hyperthermia with targeted chemotherapy agents, the development of nanoparticle-assisted heating, and automated temperature-regulation technologies for safer delivery.
Recent work at veterinary teaching hospitals has focused on thermosensitive drug carriers, which release their payload only when activated by heat, ensuring localized impact and minimal systemic toxicity. Immuno-hyperthermia, where heating is combined with immune stimulants, is another promising area under review.
Regulatory standards, treatment protocols, and long-term studies are still being refined. Wider access to clinical trials may increase the affordability and reach of this therapy. The future points toward personalized, tech-driven, minimally invasive cancer care for dogs.
Owner Experiences and Testimonials
First-hand accounts from pet owners who have chosen hyperthermia therapy can be powerful. Many describe the procedure as life-extending and stress-reducing, especially in comparison to radical surgery. One owner shared how her 10-year-old Labrador tolerated all sessions calmly, regained appetite, and showed renewed energy after only three treatments.
Another testimonial came from a family whose small mixed-breed dog had a reoccurring mammary tumor. Hyperthermia helped reduce inflammation and allowed the tumor to become operable. They called it a “bridge to surgery” that gave their dog a second chance.
These narratives often highlight the importance of trusting the veterinary team, staying informed, and balancing emotional decisions with medical facts. They also reflect that hyperthermia is more than a clinical option — it’s a compassionate path toward comfort and extended companionship.
Ethical Considerations in Cancer Treatment for Dogs
Choosing any cancer treatment for a pet brings emotional and ethical dilemmas. Owners must weigh the potential extension of life against the stress and side effects of therapy. Hyperthermia, being non-invasive and generally well-tolerated, often presents a middle ground between aggressive intervention and comfort care.
Ethical veterinary practice prioritizes informed consent, transparency in outcomes, and attention to the animal’s quality of life. Veterinarians should assess the dog’s behavior, pain levels, and post-treatment well-being at every stage, not just tumor response. Treatments that prolong suffering without improving comfort should be avoided.
Respect for the animal’s dignity and open communication with the family are essential. Hyperthermia may offer more than physical benefits — it can provide peace of mind when curative options are limited, allowing families to feel they’ve done all they could within reason.

Integrating Hyperthermia into Veterinary Oncology Practice
For clinics considering the adoption of hyperthermia equipment, several logistical and training steps are involved. It begins with selecting the right device — microwave, infrared, or ultrasound-based — depending on the types of cancers most frequently treated.
Veterinarians and technicians must undergo specific training in thermal dosimetry, temperature monitoring, and anesthesia protocols. Workflow integration also includes allocating space, coordinating with surgical and imaging departments, and developing standard operating procedures.
Patient selection criteria, treatment algorithms, and documentation systems should be clearly established. Follow-up studies and outcome tracking help validate the practice’s effectiveness and guide future refinements. As client demand for minimally invasive options grows, hyperthermia may become a central offering in forward-thinking clinics.
Alternatives to Hyperthermia for Mammary Cancer in Dogs
While hyperthermia offers unique advantages, several alternative or complementary treatments are commonly used in canine mammary cancer cases. These include:
- Surgery (mastectomy or lumpectomy): still the most definitive method for localized tumors.
- Chemotherapy: particularly effective for high-grade or metastatic tumors, with drugs like carboplatin, doxorubicin, or cyclophosphamide.
- Radiation therapy: used when surgery is incomplete or tumors are inoperable.
- Immunotherapy: a growing area of interest involving tumor vaccines or monoclonal antibodies.
- Palliative care: focused on comfort, appetite support, pain management, and fluid balance in end-stage disease.
Each modality has specific indications, benefits, and limitations. Treatment should be customized based on the dog’s age, tumor pathology, and family goals.
Long-Term Follow-Up and Monitoring
After the final hyperthermia session, dogs should be scheduled for regular re-evaluations every 4 to 8 weeks during the first six months. These visits typically involve a physical exam, imaging of the treated area, and assessment for any signs of recurrence or metastasis.
In cases where tumors were completely resolved or surgically removed following hyperthermia, annual monitoring is usually sufficient after the first year. Any sudden changes in appetite, weight, or behavior should prompt an immediate visit to the vet.
Owners may be advised to continue nutritional support, immune boosters, or mild activity regimens. Detailed medical records of hyperthermia sessions, temperature profiles, and any observed reactions are crucial for future care decisions and contribute to broader clinical research.
FAQ
What is hyperthermia therapy for dogs with cancer?
Hyperthermia therapy is a medical technique that uses controlled heat to damage or destroy cancer cells. In veterinary medicine, it is used to treat tumors like mammary cancer by raising the temperature of the tumor tissue to enhance its sensitivity to other therapies such as chemotherapy or radiation.
Is hyperthermia effective for treating canine breast cancer?
Yes, especially when used early and in combination with other treatments. Hyperthermia improves the effectiveness of traditional therapies and has shown promising results in reducing tumor size, alleviating symptoms, and extending the lives of dogs with mammary tumors.
How many sessions of hyperthermia does a dog usually need?
Typically, dogs undergo between 4 to 10 sessions depending on the tumor’s size, location, response to treatment, and whether it is part of a combined therapy plan. Sessions are often spaced one week apart.
Is the procedure painful for the dog?
The procedure is not painful. Dogs are usually sedated or anesthetized to stay calm and still during the session. Real-time temperature monitoring ensures that the heat is applied precisely, avoiding discomfort or tissue damage.
Can hyperthermia replace surgery or chemotherapy?
No, hyperthermia is generally used as a supportive treatment, not a replacement. It can make tumors more operable, reduce their size before surgery, or increase the success of chemotherapy, but it is rarely used as a standalone solution.
Are there side effects associated with hyperthermia in dogs?
Most side effects are mild, such as skin redness, minor swelling, or fatigue after treatment. Serious complications are rare if the procedure is properly performed and monitored by trained veterinary professionals.
How much does canine hyperthermia treatment cost?
Costs vary by location and clinic, but most treatments range from $500 to $1,500 per session. A full course of therapy may total between $3,000 and $10,000. Additional costs may apply for diagnostics and combined treatments.
Is this treatment available at most veterinary clinics?
No, hyperthermia therapy requires specialized equipment and trained personnel, so it is mostly available in veterinary oncology centers or teaching hospitals. It is not yet widely available in general veterinary practice.
What follow-up care is needed after treatment?
Follow-up care includes regular veterinary visits, imaging to monitor tumor changes, and blood work to assess overall health. Owners should watch for signs of skin irritation, lethargy, or appetite loss and report them promptly.
Can all dog breeds undergo hyperthermia therapy?
Most breeds can safely undergo hyperthermia, but certain dogs — such as those with respiratory or cardiac conditions — may need special precautions. The veterinarian will assess the dog’s individual risk before proceeding.
What’s the success rate of hyperthermia for mammary tumors?
Success varies depending on the stage and type of tumor. Early-stage tumors treated with hyperthermia alongside surgery or chemo have high success rates. Even in advanced cases, it often improves comfort and slows tumor progression.
Is hyperthermia safe for senior dogs?
Yes, many senior dogs tolerate hyperthermia well if their heart, kidney, and liver functions are stable. Pre-treatment screening helps identify any risks, and sedation protocols are adjusted for older dogs.
How soon will I see results after starting treatment?
Some changes in tumor size or firmness can appear after just a few sessions. However, full therapeutic effects, especially when combined with chemo or radiation, may take several weeks to become clearly noticeable.
What if the tumor comes back after hyperthermia?
In the case of recurrence, additional sessions may be scheduled, or alternative treatments such as surgery or stronger chemotherapy might be considered. Each case is evaluated individually based on response history and health status.
Can hyperthermia be used for other types of cancer in dogs?
Yes, it’s being explored for other cancers such as soft tissue sarcomas, melanomas, and osteosarcomas. While mammary cancer is the most common use today, ongoing research supports broader application in veterinary oncology.










