How Fast Does Squamous Cell Skin Cancer Spread?
How Fast Does Squamous Cell Skin Cancer Spread? The Ultimate Guide
- Understanding Squamous Cell Carcinoma (SCC) Basics
- How Fast Does Squamous Cell Skin Cancer Typically Spread?
- Risk Factors That Influence Speed of Spread
- How SCC Invades Lymph Nodes and Beyond
- Comparing Slow-Growing vs. Aggressive SCC Types
- Typical Timeline From Detection to Spread
- What Body Locations Signal Faster Spread?
- How Is SCC Diagnosed and Monitored for Spread?
- Treatment Timeliness and Its Impact on Spread
- How Does SCC Compare to Other Skin Cancers in Spread?
- When SCC Behavior Signals Urgency
- Prognosis Based on Spread and Stage
- Monitoring After Treatment to Detect Recurrence
- The Role of Imaging in Tracking SCC Spread
- How to Lower the Risk of Rapid Spread
- Final Thoughts: Why Timely Action Matters Most
- 15+ FAQ: Squamous Cell Skin Cancer Spread
Understanding Squamous Cell Carcinoma (SCC) Basics
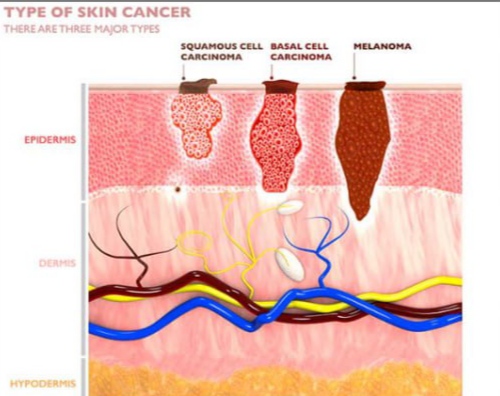
Squamous cell carcinoma (SCC) is the second most common form of skin cancer, arising from the flat squamous cells in the upper layers of the skin. It typically forms after long-term sun exposure but can also develop on scars, wounds, or in mucous membranes. SCC is generally less aggressive than melanoma but more dangerous than basal cell carcinoma, particularly when left untreated.
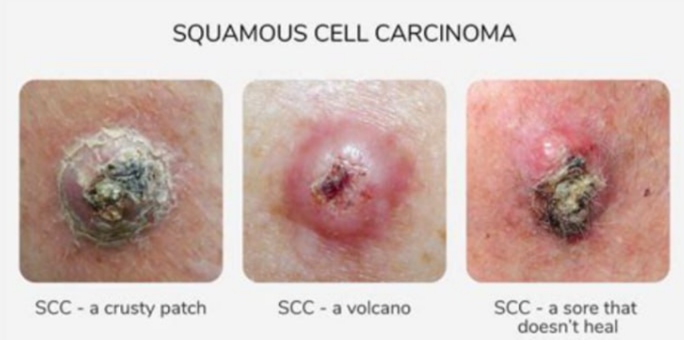
SCC often begins as a rough, scaly patch or nodule that can bleed, crust over, and resist healing. Over time, these lesions may grow deeper into surrounding tissues and, in some cases, spread (metastasize) to lymph nodes or distant organs. The key factor in determining how fast SCC spreads lies in its subtype, size, location, and depth of penetration.
This form of cancer is usually curable when detected early — but in rare cases, it can behave aggressively.
How Fast Does Squamous Cell Skin Cancer Typically Spread?
Unlike melanoma, which is notorious for rapid spread, squamous cell carcinoma usually grows slowly in its early stages. However, certain high-risk cases show much faster progression. On average, SCC grows at a rate of 0.1–0.3 cm per month, but invasive or poorly differentiated tumors may grow significantly faster and deeper.
Infographic:
Growth Timeline Comparison
| Type of Skin Cancer | Typical Growth Speed | Risk of Metastasis |
| Basal Cell Carcinoma | Very slow | Rare |
| Squamous Cell Carcinoma | Moderate (variable by subtype) | Moderate (2–5%) |
| Melanoma | Often rapid | High (15–40%) |
The spread to lymph nodes can happen in weeks to months in high-risk cases, especially if the cancer is neglected or occurs in vulnerable areas like the ears, lips, or genitals.
Risk Factors That Influence Speed of Spread
Several patient-specific and tumor-specific factors influence how quickly squamous cell carcinoma can grow or spread. Here are the most critical ones:
| Risk Factor | Effect on SCC Progression |
| Tumor location (lips, ears, genitals) | Higher likelihood of metastasis |
| Tumor size > 2 cm | Increased risk of spread |
| Poorly differentiated histology | Aggressive behavior, faster invasion |
| Weakened immune system | Less control over tumor growth |
| Chronic wounds or burns | Can mask aggressive tumors |
These elements are considered by dermatologists and oncologists when evaluating urgency and treatment approach. Immunosuppressed patients, such as those with organ transplants, are particularly at risk for fast-spreading SCCs.
How SCC Invades Lymph Nodes and Beyond
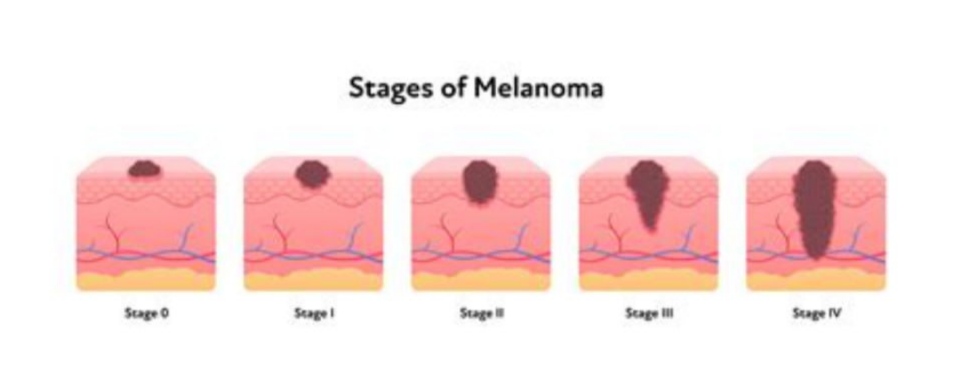
Squamous cell carcinoma typically starts at the skin surface, but if untreated, it can penetrate downward into the dermis and subcutaneous layers. Once it reaches blood vessels or lymphatic channels, it has the potential to travel to regional lymph nodes, and rarely, to distant organs like the lungs or bones.
Infographic:
Stages of SCC Invasion
- Epidermal layer (initial lesion)
- Dermal penetration (increased risk)
- Lymphatic involvement (stage III)
- Distant metastasis (stage IV)
The likelihood of systemic spread is low — around 2–5% — but when it occurs, the disease becomes much more difficult to manage. This is why regular skin checks and early treatment are critical.
As SCC becomes invasive, its behavior may resemble other forms of Dangerous Skin Cancer.
Comparing Slow-Growing vs. Aggressive SCC Types
Not all squamous cell carcinomas behave the same way. Some are superficial and remain localized for years, while others are aggressive from early on. The histological subtype and cellular differentiation grade significantly affect behavior.
Superficial SCCs may remain in the epidermis (in situ) for a long time, while poorly differentiated types can invade rapidly. For example, acantholytic and desmoplastic variants often present with deeper invasion and a greater risk of recurrence or spread.
| SCC Subtype | Typical Behavior | Spread Risk |
| Well-differentiated | Slow-growing, less invasive | Low |
| Moderately differentiated | May spread beyond skin layers | Moderate |
| Poorly differentiated | Rapid invasion, aggressive potential | High |
| Acantholytic | Poor cohesion, deeper tissue spread | High |
Identifying the exact type via biopsy helps determine the urgency of treatment and monitoring.
Typical Timeline From Detection to Spread
There is no universal timeline, but we can generalize patterns based on clinical observations and studies:
| Timeline Stage | Description |
| 0–3 months | Lesion appears, possibly mistaken for rash or sore |
| 3–6 months | Lesion thickens, bleeds, or becomes ulcerated |
| 6–12 months | Possible dermal invasion; requires medical evaluation |
| 1–2 years | Lymph node involvement in high-risk SCCs |
| 2+ years (untreated) | Rare distant metastasis to lung, bone, or liver |
SCC generally doesn’t metastasize quickly, but once it breaches the dermis, the risk of further spread increases significantly. Rapid changes in lesion appearance, bleeding, and pain suggest progression.
What Body Locations Signal Faster Spread?
The location of SCC significantly impacts its spread potential. Certain areas have a richer vascular or lymphatic supply, thinner skin, or more exposure to sun damage, making them more vulnerable.
| High-Risk Locations | Features Contributing to Aggression |
| Lips | Rich vascular supply, UV exposure |
| Ears | Thin skin, close to lymphatic drainage |
| Genital area | Delicate tissue, delayed detection |
| Perianal region | Poor visibility, high-risk HPV association |
| Scars/Burns | Altered healing may mask early symptoms |
Lesions in these zones require more aggressive treatment and closer monitoring than those on the trunk or limbs.
How Is SCC Diagnosed and Monitored for Spread?
Diagnosis begins with a clinical examination followed by a skin biopsy, which provides information on the tumor depth, subtype, and margin status. If invasion is suspected, imaging (CT, MRI, or PET scans) may be ordered to assess local and distant spread.
A visual flow:
Infographic: Diagnostic Pathway for SCC
- Skin lesion noticed
- Dermatologic evaluation
- Punch or excisional biopsy
- Histopathology report
- Staging with imaging if invasion suspected
- Follow-up plan
In cases of aggressive SCC, physicians may also check lymph nodes manually or via ultrasound. Regular follow-ups are vital, especially in the first two years after diagnosis, when recurrence or spread is most likely.
In advanced SCCs with skin involvement, cases may resemble Breast Cancer Spreads to the Skin.
Treatment Timeliness and Its Impact on Spread
Early intervention is one of the most critical factors in limiting the spread of squamous cell carcinoma. The longer SCC is left untreated, the greater the chance it will grow deeper into tissue or migrate to lymph nodes. The average time from detection to potential systemic spread in high-risk cases is approximately 12 to 24 months if left untreated.
| Scenario | Spread Risk if Treated Early | Risk if Delayed |
| Small, localized SCC | <1% | 4–6% |
| SCC near high-risk areas (lips) | ~3% | >10% |
| Recurrent SCC | ~5% | 15–20% |
Prompt surgical removal, typically via Mohs micrographic surgery, offers the best prognosis. Delays in diagnosis—especially in hidden or ignored lesions—can dramatically increase risk of spread.
How Does SCC Compare to Other Skin Cancers in Spread?
Squamous cell carcinoma lies in the middle of the skin cancer aggression spectrum. It is more dangerous than basal cell carcinoma, which rarely spreads, but generally less aggressive than melanoma.
Comparison Table:
| Skin Cancer Type | Spread Potential | Average Spread Timeline |
| Basal Cell Carcinoma | Very low | Rarely metastasizes |
| Squamous Cell Carcinoma | Moderate (2–5%) | Can spread within 1–2 years |
| Melanoma | High (15–40%) | Can spread in a matter of weeks |
Patients diagnosed with SCC are often reassured that with early treatment, the chance of spread is very low. However, understanding these differences is crucial in triaging urgency and monitoring over time.
When SCC Behavior Signals Urgency
Several warning signs indicate that SCC may be more aggressive or already spreading:
- Rapid growth over weeks
- Increasing pain, bleeding, or crusting
- New lumps under the skin near the original lesion
- Fatigue, weight loss, or general malaise (rare, late signs)
Such developments demand immediate imaging and potentially broader systemic evaluation. For example, in some rare presentations, early skin metastasis may mimic symptoms seen in conditions like Early Skin Metastases, requiring a multidisciplinary review and biopsy confirmation.
The distinction between localized skin changes and systemic involvement is subtle—so dermatologic vigilance is critical.
Prognosis Based on Spread and Stage
Prognosis in squamous cell carcinoma depends heavily on the stage at diagnosis. Most localized cases are cured with excision and never return. However, when SCC spreads to lymph nodes or distant organs, outcomes are poorer, and treatment becomes more complex.
| SCC Stage | 5-Year Survival Rate (Approx.) |
| Localized (Stage I) | 95–98% |
| Regional Spread (II) | 70–80% |
| Lymph Node Involvement (III) | 50–60% |
| Distant Metastasis (IV) | <35% |
Factors that improve prognosis include early detection, clean surgical margins, and absence of perineural invasion. Post-treatment surveillance is essential, particularly within the first 2 years when recurrence is most likely.
Monitoring After Treatment to Detect Recurrence
After successful treatment, particularly in high-risk cases, follow-up is essential. The first two years are considered the most critical for recurrence. Dermatologists typically recommend skin checks every 3–6 months during this period.
| Follow-up Phase | Frequency | Purpose |
| Year 1–2 | Every 3–6 months | Early detection of recurrence |
| Year 3–5 | Every 6–12 months | Monitor for new or recurring lesions |
| After Year 5 | Annually | Lifelong surveillance for new skin cancers |
Advanced cases may also require periodic imaging or lymph node evaluation, especially if perineural invasion or deep dermal penetration was observed in the pathology.
The Role of Imaging in Tracking SCC Spread
While most SCC cases are diagnosed and staged clinically, imaging is used when deeper invasion or metastasis is suspected. This includes ultrasound, CT, MRI, or PET scans — depending on lesion location and symptoms.
| Imaging Type | Best Used For | Notes |
| Ultrasound | Enlarged lymph nodes | Non-invasive, low cost |
| CT Scan | Suspected deep tissue or lung spread | Cross-sectional detail |
| MRI | Tumors near nerves or muscles | Especially for head & neck SCC |
| PET Scan | Whole-body assessment for metastasis | More sensitive, higher cost |
Imaging is not always needed in low-risk, superficial cases — but becomes essential in recurrent or poorly differentiated SCCs.
How to Lower the Risk of Rapid Spread
While genetic and immune-related factors can’t be controlled, there are actionable steps to reduce the chance of aggressive SCC:
Infographic: Protective Actions
- Early biopsy of new or changing lesions
- Avoid chronic sun exposure and use broad-spectrum sunscreen
- Regular skin exams, especially for high-risk individuals
- Manage wounds, scars, or burns with care
- Avoid tanning beds or artificial UV light
These proactive choices can dramatically change outcomes by catching lesions before they penetrate deeper layers.
Final Thoughts: Why Timely Action Matters Most
Squamous cell carcinoma can be deceptive. It often starts as something that seems minor — a scaly patch or bump that doesn’t go away. But under the surface, it can grow inward or outward at unpredictable rates. That’s why timely diagnosis, histological typing, and treatment are essential.
In most cases, SCC is treatable and non-life-threatening, but in a small percentage, it may act aggressively, especially if ignored. Understanding how fast it spreads is critical for patients, families, and physicians alike.
Related cases can resemble Dangerous Skin Cancer or even rare spread forms of Breast Cancer Spreads to the Skin, making differential diagnosis essential.
15+ FAQ: Squamous Cell Skin Cancer Spread
1. How long can squamous cell carcinoma go unnoticed?
It can remain unnoticed for months to years if it’s slow-growing or resembles benign lesions. Some cases only come to light when bleeding or ulceration begins.
2. Can SCC come back after removal?
Yes, especially if margins were not clear, or if the tumor was aggressive. Recurrence rates vary but can be up to 10% in high-risk cases.
3. What does metastatic SCC feel like?
It may cause firm lumps under the skin, swelling in lymph nodes, or unexplained fatigue. Pain or discomfort may arise near the original site.
4. Are certain people more likely to develop fast-spreading SCC?
Yes — people with organ transplants, chronic sun exposure, HPV infection, or a history of radiation therapy are at higher risk.
5. How do I know if my SCC has spread?
Only biopsy and imaging can confirm spread. Enlarged lymph nodes or unusual symptoms should prompt evaluation.
6. Is SCC always removed surgically?
Most often, yes. Surgery offers the best control. In some cases, radiation or topical treatments are added.
7. Does SCC spread through the bloodstream?
It primarily spreads through the lymphatic system, but late-stage cancers may enter the bloodstream and reach lungs or bones.
8. What is perineural invasion in SCC?
It’s when the tumor grows along nerve pathways. This is a high-risk feature and often leads to recurrence or spread.
9. How can I protect a scar or burn from becoming SCC?
Keep it clean, covered when exposed to sun, and monitor for any changes in color, texture, or bleeding.
10. Can SCC affect younger people?
It’s rare in young adults but increasing in incidence due to sunbed use and immunosuppression.
11. Can it be confused with psoriasis or eczema?
Yes. Many SCCs are misdiagnosed early. If a skin lesion resists treatment or bleeds, a biopsy is warranted.
12. Should I get a second opinion before surgery?
If you’re unsure about the diagnosis or treatment plan, especially for aggressive or recurrent lesions, yes — a second opinion helps.
13. Can sunscreen really prevent SCC?
It doesn’t eliminate risk but greatly reduces it. Daily use of SPF 30 or higher is recommended.
14. Is there a vaccine to prevent SCC?
No, but HPV vaccines may reduce the risk of SCC in the genital or anal area.
15. What is the survival rate if SCC spreads?
Once it reaches distant organs, survival drops significantly — to around 30–35%. Early detection offers the best prognosis.












