How Cancer Can Lead to Low Phosphate Levels: A Comprehensive Guide for Patients and Caregivers
- The Overlooked Link Between Cancer and Phosphate Levels
- What Is Phosphate and Why It Matters
- How Cancer Disrupts Phosphate Balance
- Common Cancers Associated with Low Phosphate Levels
- Chemotherapy and Hypophosphatemia
- Radiation Therapy and Phosphate Regulation
- Symptoms of Low Phosphate in Cancer Patients
- Diagnosing Hypophosphatemia in Oncology
- Treatment Strategies for Cancer-Related Hypophosphatemia
- Dietary and Nutritional Considerations
- Complications from Untreated Low Phosphate Levels
- Comparison of Phosphate Disturbances in Cancer Context
- Monitoring and Follow-Up in Oncology Settings
- Pediatric Considerations: Children with Cancer and Phosphate Imbalance
- The Role of Multidisciplinary Care in Managing Hypophosphatemia
- Future Research and Emerging Therapies
- FAQ: Can Cancer Cause Low Phosphate Levels?
The Overlooked Link Between Cancer and Phosphate Levels
Phosphate is a mineral that rarely receives attention in conversations about cancer care, yet its physiological importance is profound. In patients undergoing treatment or living with cancer, the balance of phosphate in the blood can become disrupted, leading to a condition called hypophosphatemia. While the focus in oncology often lies on managing tumor burden, immune function, and weight loss, imbalances in minerals like phosphate can have equally serious clinical consequences. Hypophosphatemia can affect energy production, muscular and neurological function, cardiac output, and even the immune response—all of which are already vulnerable in individuals battling malignancy.
In cancer care, phosphate abnormalities are not always recognized or treated promptly. This may be due to overlapping symptoms, such as fatigue or confusion, which are common both in cancer progression and phosphate deficiency. In addition, blood phosphate levels are not always monitored unless there is a specific indication, which may lead to underdiagnosis. This article provides a comprehensive exploration of how and why phosphate levels drop in cancer patients, which cancers are most commonly involved, how treatment regimens affect mineral balance, and what can be done to manage or prevent complications.
What Is Phosphate and Why It Matters
Phosphate, or inorganic phosphate, is a critical mineral found in every cell of the body. Roughly 85% of the body’s phosphate is stored in bones and teeth, with the remainder circulating in blood and soft tissues. It plays a central role in forming and stabilizing DNA and RNA, producing cellular energy (ATP), facilitating cell signaling, and maintaining acid-base balance. Without adequate phosphate, cells cannot generate the energy they need to function, which is why even mild deficiencies can produce systemic effects.
Phosphate is primarily regulated by the intestines, kidneys, bones, and endocrine system. Dietary phosphate is absorbed in the small intestine, with help from vitamin D. The kidneys then either retain or excrete phosphate based on the body’s current needs, a process controlled by hormones like parathyroid hormone (PTH) and fibroblast growth factor 23 (FGF23). These systems normally work in synchrony, but in patients with cancer, these processes can be disrupted by tumors, therapies, or nutritional deficiencies. The result is a potentially dangerous drop in phosphate that can go unnoticed until symptoms are severe.
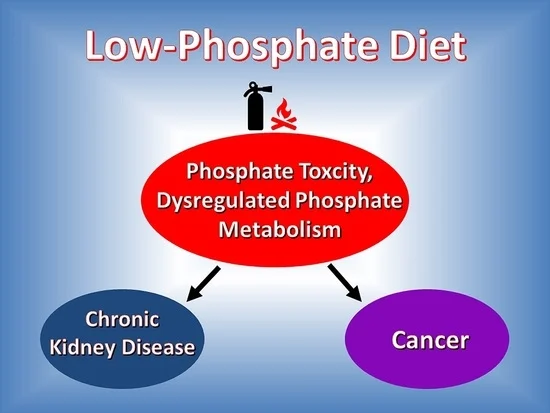
How Cancer Disrupts Phosphate Balance
Cancer can cause low phosphate levels in the body through several mechanisms. One common route is through increased phosphate excretion by the kidneys, which can be triggered by tumor-secreted substances like FGF23 or paraneoplastic syndromes. These factors act hormonally to tell the kidneys to excrete more phosphate than usual, even when blood levels are already low. Tumors such as prostate, ovarian, breast, or small-cell lung cancers have been reported to produce these substances.
Another pathway involves the shifting of phosphate into cells. In cases of rapid cell proliferation or destruction—such as during aggressive tumor growth or tumor lysis syndrome—phosphate may be pulled from the bloodstream into the cells or locked into byproducts of breakdown. This leads to a sudden and sometimes dramatic drop in blood phosphate. Finally, cancer-related malabsorption due to gastrointestinal tumors, surgical resections, or radiation can impair the intestine’s ability to absorb phosphate, especially if combined with poor nutritional intake. All these factors can act together, making the cause of hypophosphatemia multifactorial and requiring a detailed clinical evaluation.
Common Cancers Associated with Low Phosphate Levels
Certain cancers are more strongly associated with the development of hypophosphatemia. Hematologic malignancies such as acute lymphoblastic leukemia (ALL) and non-Hodgkin lymphoma often lead to electrolyte imbalances due to their high cell turnover rates and responsiveness to chemotherapy. These cancers are also closely linked to tumor lysis syndrome, a dangerous condition that causes massive electrolyte shifts, including an initial phosphate spike followed by a crash as the body redistributes or excretes excess levels.
Solid tumors like prostate cancer, breast cancer, and small-cell lung cancer may produce hormone-like substances that influence phosphate metabolism. In prostate cancer, for instance, metastatic spread to bone can lead to increased phosphate uptake by bone tissue, reducing levels in the bloodstream. Tumors affecting the gastrointestinal tract, including pancreatic and colon cancers, can impair nutrient absorption or cause chronic diarrhea, further contributing to losses. It is important to note that the presence of low phosphate in a patient with cancer may point to underlying complications, even in early stages. In some patients with colon tumors, low phosphate may be one of many subtle metabolic changes—others may include changes in bowel habits or electrolyte loss, as explored further in the article 7 Symptoms of Colon Cancer in Women.
Chemotherapy and Hypophosphatemia
Chemotherapy, though essential in cancer management, often creates collateral damage in various organs, including the kidneys and gastrointestinal tract—two of the most important regulators of phosphate balance. Several chemotherapeutic agents, such as cisplatin, ifosfamide, and methotrexate, are directly nephrotoxic. This toxicity compromises the renal tubules’ ability to reabsorb phosphate, leading to excessive losses in urine.
Additionally, chemotherapy can damage the lining of the intestines, reducing their ability to absorb phosphate from food. This is particularly problematic in patients experiencing mucositis, diarrhea, or prolonged nausea. Chemotherapy can also trigger tumor lysis syndrome in rapidly growing cancers, where intracellular contents are dumped into the bloodstream after sudden cell death. This initially raises phosphate levels but causes a rebound effect where phosphate is either rapidly excreted or locked away inside other cells.
Over time, repeated cycles of chemotherapy deplete the body’s mineral reserves, especially if dietary intake is low. Many patients experience appetite loss, vomiting, and malnutrition, all of which contribute to diminished phosphate availability. This makes it essential for oncologists to monitor serum phosphate levels throughout treatment and adjust nutrition or medication as needed.

Radiation Therapy and Phosphate Regulation
The Impact of Radiation on Bone and Kidney Function
Radiation therapy, especially when targeted near the abdomen, pelvis, or spine, can damage organs involved in phosphate regulation. For example, radiation nephropathy may occur when the kidneys are exposed to high doses, leading to reduced phosphate reabsorption and chronic losses through urine. Radiation affecting the intestines can impair phosphate absorption and create long-term gastrointestinal malabsorption syndromes.
In cases where bones are irradiated, especially those with metastases, mineral metabolism becomes more complex. Bone turnover increases, sequestering phosphate in the skeletal matrix. Furthermore, radiation-induced inflammation and hormonal changes can exacerbate the imbalance. These effects may not be immediate but often accumulate over weeks or months of therapy, requiring long-term monitoring of phosphate and related minerals. “Does botox cause cancer” — as an example where it is important to distinguish real metabolic effects from controversial or unconfirmed ones.
Symptoms of Low Phosphate in Cancer Patients
Clinical Clues That Often Go Unrecognized
The symptoms of hypophosphatemia can be subtle and often overlap with general cancer-related fatigue, making them hard to identify without laboratory testing. Mild cases may produce nonspecific fatigue, muscle weakness, and reduced appetite. As phosphate levels drop further, patients may experience bone pain, irritability, confusion, difficulty breathing, or even cardiac arrhythmias.
In severe cases, hypophosphatemia can lead to rhabdomyolysis (muscle breakdown), hemolytic anemia, and impaired white blood cell function, increasing infection risk. These complications are particularly dangerous in immunocompromised cancer patients. Because these symptoms are nonspecific, many go untreated unless clinicians specifically test for phosphate levels during routine blood work.
Diagnosing Hypophosphatemia in Oncology
Laboratory Workup and Clinical Assessment
Diagnosis of low phosphate begins with a serum phosphate test, often included in routine electrolyte panels or ordered when symptoms suggest a metabolic imbalance. However, phosphate levels can fluctuate quickly depending on feeding status, medications, and treatment timing, so single measurements may not be sufficient. Serial testing is often necessary to confirm a persistent drop.
Additional tests include urinary phosphate excretion to determine renal loss, serum calcium and magnesium levels (which frequently shift in tandem), and vitamin D status. In cases of unexplained hypophosphatemia, FGF23 testing may reveal a hormone-secreting tumor. For patients with gastrointestinal symptoms, malabsorption panels or stool studies may be warranted. A comprehensive metabolic panel, when reviewed in context, provides vital insight into the underlying cause.
Treatment Strategies for Cancer-Related Hypophosphatemia
Restoring Phosphate Safely and Effectively
Managing low phosphate levels in cancer patients requires a personalized approach that accounts for the underlying cause, cancer type, and patient’s clinical status. Mild cases are often addressed through dietary phosphate sources or oral supplements such as sodium phosphate or potassium phosphate. In patients with compromised absorption or more severe depletion, intravenous phosphate replacement may be necessary.
It’s essential to monitor phosphate closely during repletion to avoid hyperphosphatemia, which carries its own risks, especially in patients with kidney dysfunction. Replacement therapy should also address coexisting deficiencies in magnesium or vitamin D, as both can impair phosphate reabsorption. Long-term care must also correct the root problem—whether that’s controlling tumor activity, adjusting nephrotoxic treatment regimens, or improving nutrient intake.
Dietary and Nutritional Considerations
Supporting Phosphate Levels Through Food and Diet
Nutrition plays a vital role in preventing and treating hypophosphatemia, particularly in cancer patients experiencing appetite loss, nausea, or malabsorption. Foods naturally high in phosphate include dairy products, meats, nuts, whole grains, eggs, and legumes. However, phosphate from plant-based sources like beans and seeds is less bioavailable than that from animal products due to phytate content.
Cancer patients may need dietary counseling to ensure adequate intake, especially if undergoing chemotherapy or radiation that affects the GI tract. For those on feeding tubes or parenteral nutrition, phosphate must be correctly balanced with other electrolytes and calories. Registered dietitians often work closely with oncologists to design individualized plans that meet both caloric and mineral needs. “Is bowel leakage a sign of cancer” — After all, intestinal absorption disorders caused by a tumor can also cause electrolyte deficiency.
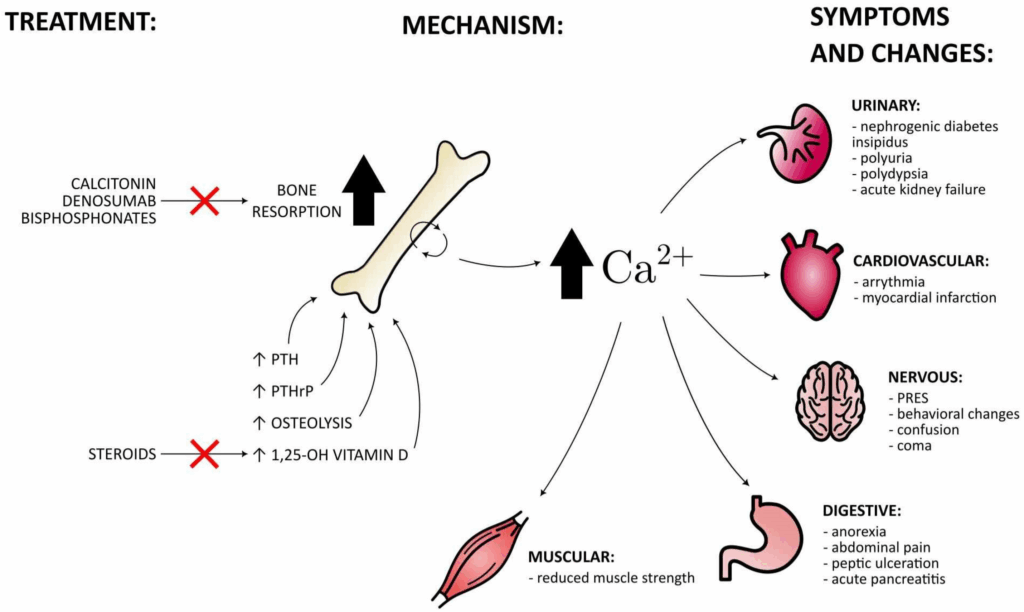
Complications from Untreated Low Phosphate Levels
Risks That Amplify Cancer’s Impact
Untreated hypophosphatemia can have far-reaching effects, particularly in individuals whose systems are already compromised by cancer or aggressive treatment. Severe phosphate deficiency impairs the ability of muscles to contract, including the diaphragm, which can lead to respiratory failure. This is especially dangerous in patients who are already fatigued or undergoing sedation.
Neurological effects include delirium, memory loss, and seizures. Cardiac complications, such as arrhythmias and decreased contractility, may exacerbate existing heart problems or contribute to treatment delays. In patients with bone metastases, low phosphate may worsen bone pain or fragility. Additionally, immune suppression from phosphate imbalance raises the risk of infection and reduces response to treatment.
Comparison of Phosphate Disturbances in Cancer Context
| Factor | Effect on Phosphate | Mechanism |
| Tumor lysis syndrome | Low initially | Cellular phosphate uptake after lysis |
| FGF23-secreting tumors | Low | Increased renal excretion of phosphate |
| Chemotherapy (cisplatin) | Low | Nephrotoxicity impairs renal reabsorption |
| Radiation to GI tract | Low | Impaired absorption due to mucosal damage |
| Poor nutrition/malabsorption | Low | Inadequate intake or absorption of phosphate |
| Kidney dysfunction | Low or high | Altered excretion depending on tubular damage |
| Bone metastasis | Low | Sequestration of phosphate into new bone formation |
This comparison emphasizes the importance of monitoring both lab results and clinical context, especially when multiple contributing factors overlap in oncology care.
Monitoring and Follow-Up in Oncology Settings
Ensuring Long-Term Phosphate Stability
Ongoing monitoring of phosphate levels is essential for cancer patients—especially those receiving intensive treatments or dealing with malignancies that directly affect mineral balance. Follow-up should include regular bloodwork during and after chemotherapy cycles, hospitalization, or radiation, with special attention to patients showing neuromuscular symptoms or unexplained fatigue.
Renal function, vitamin D levels, and magnesium status should also be tracked simultaneously. In high-risk cases such as hematologic malignancies or patients with known FGF23-producing tumors, phosphate testing may be integrated into routine panels. Survivorship care must extend beyond cancer remission to include correction of lingering metabolic disturbances, ensuring a safer return to daily life and reducing risk of relapse-related complications.
Pediatric Considerations: Children with Cancer and Phosphate Imbalance
How Hypophosphatemia Manifests in Younger Patients
While less common, low phosphate levels can occur in pediatric oncology, particularly among children with leukemia, bone tumors, or those undergoing high-intensity chemotherapy. Growth adds another layer of complexity, as children require higher phosphate availability for skeletal development and cellular proliferation. In this group, low phosphate may present as irritability, muscle weakness, slowed growth, or difficulty feeding.
Pediatric treatment protocols often include careful monitoring of electrolytes, and nutritionists play a crucial role in supporting bone and metabolic health. Since children’s kidneys and intestines are more responsive to treatment interventions, phosphate can often be corrected quickly, but requires vigilance to avoid refeeding syndrome or other electrolyte shifts.
The Role of Multidisciplinary Care in Managing Hypophosphatemia
Coordination Between Oncology, Nutrition, and Nephrology
Treating hypophosphatemia in cancer patients often requires a collaborative approach. Oncologists focus on tumor control and chemotherapy planning, while nephrologists evaluate renal phosphate handling and adjust replacement strategies. Nutritionists ensure that intake meets metabolic demands and advise on supplementation during periods of anorexia or GI toxicity.
Palliative care teams may also get involved when patients are in advanced stages of illness, balancing the risks and benefits of supplementation in the context of comfort-focused care. Effective communication between all care providers is essential to prevent oversights, especially in outpatient settings where symptoms may be vague and evolving.
Future Research and Emerging Therapies
What We Still Don’t Know About Phosphate and Cancer
Despite increasing awareness, hypophosphatemia remains under-researched in the oncology setting. Ongoing studies are exploring better biomarkers for early detection, targeted therapies to block FGF23-related phosphate wasting, and improved formulas for nutritional support. Researchers are also investigating whether chronic phosphate depletion affects cancer prognosis, treatment tolerance, or recurrence rates.
Some experimental therapies aim to modulate mineral balance more precisely in patients with bone involvement or advanced gastrointestinal cancers. As our understanding of the tumor microenvironment evolves, phosphate metabolism may emerge as a therapeutic target in select cases. This makes future collaboration between oncologists and endocrinologists especially promising.
FAQ: Can Cancer Cause Low Phosphate Levels?
Can all types of cancer cause low phosphate levels?
Not all, but several cancers—especially hematologic malignancies, prostate cancer, and some gastrointestinal tumors—can cause hypophosphatemia either directly or through treatment-related complications.
What is the most common reason for low phosphate in cancer patients?
Chemotherapy and tumor lysis syndrome are the most frequent contributors, especially in aggressive or fast-growing tumors.
How do I know if I have low phosphate?
Symptoms may include muscle weakness, confusion, fatigue, or irregular heartbeat, but confirmation requires a blood test.
Can low phosphate levels be life-threatening?
Yes. In severe cases, it can lead to respiratory failure, arrhythmias, and immune suppression, particularly if untreated.
Are there long-term effects of low phosphate in cancer survivors?
Chronic hypophosphatemia may impact bone health, energy metabolism, and cognitive function, especially if unrecognized for months.
Can radiation cause low phosphate?
Yes. Radiation to the kidneys, intestines, or bones can impair phosphate absorption or increase loss.
How is low phosphate treated during cancer care?
Depending on severity, treatment ranges from dietary changes and oral supplements to IV phosphate replacement.
Do phosphate levels affect cancer treatment outcomes?
Indirectly, yes. Severe deficiencies can delay treatment, worsen side effects, or contribute to complications.
What foods help restore phosphate levels naturally?
Animal proteins like dairy, eggs, and meats are rich in bioavailable phosphate and should be included when possible.
Does vitamin D influence phosphate levels?
Yes. Vitamin D enhances phosphate absorption in the intestines, and deficiency can worsen hypophosphatemia.
Is low phosphate more common in children or adults with cancer?
It’s more closely tracked in adults but does occur in children, particularly those with leukemia or sarcomas.
Can kidney function affect phosphate in cancer patients?
Absolutely. Kidneys regulate phosphate, and any impairment from cancer or treatment can disrupt this balance.
What’s the link between FGF23 and cancer?
Some tumors secrete FGF23, a hormone that increases phosphate loss via the kidneys, leading to persistent hypophosphatemia.
How often should phosphate levels be checked during treatment?
In high-risk patients, levels should be monitored weekly or biweekly, particularly during active treatment phases.
Are low phosphate levels a sign of cancer on their own?
Not typically. They usually occur in the context of existing cancer or its treatment, not as a standalone early warning.









