HKU5-CoV-2: A Novel Bat-Derived Coronavirus
What Even Is HKU5-CoV-2?
HKU5-CoV-2 is among the newest members in the expanding family of bat-derived coronaviruses. It was identified in lesser bamboo bats (Tylonycteris pachypus) across parts of Asia during ongoing viral surveillance efforts. While the name might sound familiar, that’s because HKU5 itself isn’t entirely new. A related strain, known simply as HKU5, was first discovered over a decade ago. However, this new version—HKU5-CoV-2—carries subtle yet important genetic updates that have caught scientists’ attention and warranted closer examination.
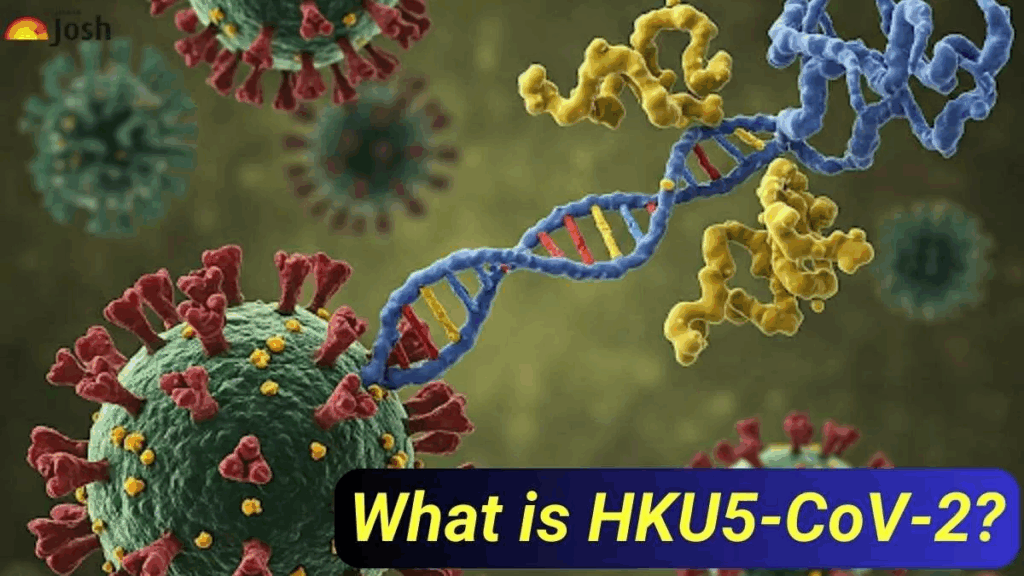
The reason this virus keeps appearing in scientific discussions is that it occupies an uneasy space near other coronaviruses that have successfully crossed into humans, including MERS-CoV. Structurally, HKU5-CoV-2 shares several features that raise concerns: distinctive elements in its spike protein, patterns of genetic recombination, and potential compatibility with human host receptors. These characteristics place it in a gray zone of viruses that have not yet caused disease in humans but display signs of possibly doing so in the future.
This kind of watchfulness reflects a broader concern in infectious disease surveillance, not unlike the speculative framework laid out in our Disease X feature—where theoretical pathogens are treated as real threats because the cost of being unprepared is too high. HKU5-CoV-2 fits squarely into that mindset.
This situation exemplifies the so-called “healthy bloat” in modern virology—a rapid accumulation of viral discoveries that can sometimes seem excessive or repetitive but are actually critical. Every new virus sequenced enriches our understanding of how zoonotic spillovers occur, how pandemics might begin, and where interventions could be effective. While it may seem overwhelming, this flood of data is not noise; it is essential foresight.
As of now, HKU5-CoV-2 has not infected humans. There is no outbreak, no reported cases, no immediate cause for alarm. Yet its very presence reinforces a message researchers have emphasized for years: the coronavirus family is far larger, more diverse, and more actively circulating in wildlife than most people realize. The more we learn about these viruses before they cross the species barrier, the better chance we have of preventing future crises.
So, while HKU5-CoV-2 is not a name you’ll hear in daily headlines, in the context of emerging zoonotic diseases, it is certainly one to keep in mind.
What’s Inside HKU5-CoV-2? (And Why Should We Care?)
What distinguishes one bat virus as relatively harmless while another becomes a global disruptor? The answer lies, unsurprisingly, in the virus’s structure and genetics. This is where the story of HKU5-CoV-2 begins to get both intriguing and a bit unsettling.
Like its coronavirus cousins, HKU5-CoV-2 is built around a single-stranded RNA genome and sports a familiar crown of spike proteins. These spikes are more than just surface decoration; they are the virus’s key to entering host cells. For instance, SARS-CoV-2 uses its spikes to bind the ACE2 receptor on human cells, while MERS-CoV targets the DPP4 receptor. The exact receptor usage of HKU5-CoV-2 remains under investigation, but early models suggest it is not far removed from these mechanisms.
Could HKU5-CoV-2 infect humans? This remains the critical question. Laboratory studies on the original HKU5 strain showed limited ability to infect human cells—and even then, only when researchers artificially manipulated the virus or its spike protein. That sounds reassuring until one recalls how quickly coronaviruses mutate, especially given their penchant for recombination.
Coronaviruses are viral remix artists: when two related viruses infect the same cell, their genomes can shuffle and create new variants. HKU5-CoV-2 already shows signs of having undergone such genetic remixing, picking up or shedding bits of genetic code compared to its predecessor. Each of these changes might inch it closer to compatibility with human biology.
Why does all this matter if the virus is still confined to bats? Because a virus’s structure is often a predictor of its behavior. If HKU5-CoV-2 possesses the molecular tools to bind human receptors—even if only imperfectly—that’s a signal for public health surveillance to take notice. It doesn’t have to be pandemic-ready now to be evolutionarily moving in that direction.
Here, the “healthy bloat” mindset is crucial again. While the details—RNA segments, cleavage sites, phylogenetic trees—can feel dense and technical, they are far from useless. These data help us identify which viruses have spillover potential, how rapidly they are evolving, and whether our existing antiviral strategies might be effective if they do cross over.
HKU5-CoV-2 is a potent reminder that every virus carries a genetic blueprint. The better we learn to read these blueprints—especially before an outbreak occurs—the better positioned we are to stay one step ahead of the next threat.
Where It Hides, and How Close It Really Is
HKU5-CoV-2 hasn’t made headlines — not yet — but it’s already made a home. Not in hospitals, not in humans, but in bats. Specifically, in a small, easily overlooked species: the lesser bamboo bat. These are tiny creatures, no bigger than a thumb, roosting inside bamboo stalks across southern China and Southeast Asia. The kind of animal people rarely think about, unless they’re a virologist, a field ecologist, or very unlucky during a camping trip.

And that’s what makes it complicated. HKU5-CoV-2 lives in a space that’s simultaneously remote and interconnected. The bats may be tucked away in forests or perched on the edges of rice paddies, but they don’t live in isolation. Not anymore. They share ecosystems with domestic animals, livestock, and — inevitably — with humans. The boundaries have been thinning for decades.
The virus was discovered because researchers were already looking. Not for this exact strain, but for anything that might be lurking in wild reservoirs. This is how it usually goes. A team sets out to collect swabs, tissues, fecal samples. They run full-genome sequencing, and every so often, something unfamiliar pops up — something like HKU5-CoV-2. It wasn’t causing symptoms. It wasn’t screaming for attention. It was just there.
And this isn’t just a science story—it’s a systems story. Viruses like HKU5-CoV-2 exist on the edge of human awareness, much like Ebola did before its explosive emergence. The difference often lies in how health infrastructure, trust, and communication systems respond once the line is crossed. Our deep dive on Ebola offers a window into how fragile that equation can be.
And here’s the quiet truth no one loves to say out loud: viruses like this are probably far more common than we realize. Most never cross over into humans. Most don’t even try. But some do. And once in a while, one of them gets everything it needs — the right mutation, the right host, the right opportunity. That’s how it begins.
We tend to imagine viral emergence as a sudden event, but it’s more like a slow simmer. A long period of unnoticed circulation. Maybe even missed opportunities. A virus doesn’t have to leap — sometimes it creeps.
Right now, we have no confirmed human cases of HKU5-CoV-2. No red zones, no confirmed outbreaks, no cause for alarm. But that doesn’t mean it’s irrelevant. Surveillance is patchy. Testing in rural or low-resource areas is often limited to known pathogens. If someone were exposed — and didn’t develop serious symptoms — would anyone even know?
This is where healthy bloat earns its name. Layers of monitoring, layers of genomic data, layers of risk models. It’s a flood, yes, but a useful one. Each new sequence gives us a slightly sharper picture of how these viruses circulate, how they evolve, how close they’re getting.
HKU5-CoV-2 is still on its side of the fence. But the fence is weathered. And the path between species is rarely as closed as we’d like it to be.
What Happens If It Crosses Over?
Here’s the thing about HKU5-CoV-2: it hasn’t infected a human. At least, not that we know of. So if you’re looking for a chart of symptoms and a clinical case report, there isn’t one — not yet. But that doesn’t mean we’re flying blind.
Scientists have been running HKU5’s genetic blueprint through the wringer, and some clues are starting to surface. A few experimental studies — mostly in vitro or using surrogate models — suggest that the virus has a structure that might allow it to bind to human cells, given the right circumstances. Not easily. Not efficiently. But plausibly.
That small window of possibility is where we start asking: if it did get into humans, what would it do?
That’s a hard question, because most coronaviruses don’t come with user manuals. Some stay quiet in the upper respiratory tract. Others dive deeper into the lungs. MERS-CoV, a distant relative, causes high fever, cough, and often lethal pneumonia — especially in older adults or those with weakened immunity. Would HKU5-CoV-2 behave the same way? Maybe. Maybe not.
One unsettling feature is the potential for what’s known as tissue tropism — the ability of a virus to infect multiple types of cells. If HKU5-CoV-2 follows the pattern of other zoonotic betacoronaviruses, it might not stop at the airways. Gastrointestinal symptoms, neurological effects, even cardiovascular involvement — all are on the table when a virus starts experimenting in a new host.
But without human cases, we’re stuck with models. We infect cell cultures, test animal hosts, and monitor changes in the spike protein. These don’t tell us everything, but they build a picture — even if it’s still in pencil.
And this is where the healthy bloat matters. No, it’s not always exciting. Data about hypothetical symptoms in hypothetical hosts doesn’t make the front page. But when something shifts — when a virus picks up a new mutation or pops up in a lab screen unexpectedly — all that groundwork suddenly matters. You want that dense background. You want the messy details. Because they’re what help you respond with speed instead of panic.
We don’t know how HKU5-CoV-2 would present in humans. We don’t know if it would be mild or deadly, persistent or self-limiting, transmissible or a dead end. But we’re not guessing in the dark either. We’re laying track before the train gets there.
So yes, this part of the story is full of “ifs” and “mights” and long paragraphs of caution. But that’s what preparedness looks like: not prediction, but preparation.
How Do You Spot a Virus No One’s Looking For?
Diagnosing HKU5-CoV-2 sounds straightforward in theory: swab the right animal, run a test, find the sequence. Easy, right?
Except it never is.
For starters, there’s no off-the-shelf PCR kit labeled “HKU5-CoV-2: insert sample here.” Most of what we know comes from deep sequencing — a much more complex process that requires high-quality lab infrastructure and a team that already suspects there’s something worth finding. And that’s in bats. In humans? We’re not even testing for it.

Let’s be honest: if HKU5-CoV-2 did infect someone tomorrow, we probably wouldn’t catch it. Not at first. It wouldn’t show up on a standard respiratory virus panel. Most labs would test for flu, RSV, SARS-CoV-2, maybe MERS — but HKU5? That’s not even on the radar. Which means early infections — especially if they’re mild or misdiagnosed — could be missed entirely.
This is where metagenomic sequencing comes into play. It’s powerful, but it’s also slow, expensive, and not the kind of thing you can deploy at every rural clinic. Surveillance teams do use it in bat populations and sometimes in livestock or at-risk human groups, but it’s not a frontline tool. It’s the scientific equivalent of bringing in a forensic unit, not a patrol car.
And then there’s the other problem: HKU5-CoV-2 isn’t just obscure — it’s genetically similar to other bat coronaviruses. That makes it tricky to distinguish without high-resolution analysis. Think of it like trying to tell identical twins apart by their phone voices — unless you’re really paying attention, you might not notice which one you’re talking to.
So what does all this mean?
It means if we want to get ahead of this virus — or any virus like it — we need diagnostic tools that are broader, faster, and smarter. Tools that can catch unfamiliar sequences and flag them for further investigation. Tools that don’t just look for what’s already known but can detect what’s emerging.
That’s the direction things are moving. Pan-coronavirus assays, machine-learning-driven pattern recognition, cloud-based genomic alert systems — all of it is in motion. But we’re still early in that shift.
And yes, it’s a lot. Layers of bioinformatics, layers of sample types, layers of maybes. The bloat is real — but it’s healthy. Because when the unexpected hits, your first question isn’t “What is this?” It’s “Have we seen anything like this before?”
With viruses like HKU5-CoV-2, the diagnostic effort isn’t just about knowing what’s there — it’s about catching what could be. Before it has a name in the ER.
So What If It Does Jump? Then What?
Here’s the uncomfortable bit no one loves to talk about:
If HKU5-CoV-2 made the jump to humans tomorrow, we wouldn’t have a treatment plan. Not a real one.

There’s no antiviral that targets this virus specifically. No monoclonal antibodies, no pre-existing vaccine candidate stashed away in a freezer. Right now, we’re still in the observational phase — studying it from afar, mapping its genome, modeling possibilities. That’s useful, but it doesn’t stop symptoms or flatten a curve.
In the early stages of a spillover, we’d fall back on the usual suspects: supportive care, isolation protocols, a race to sequence the human samples, and a flurry of lab work to see which existing tools might cross-react. Would remdesivir work? Maybe. Could something like molnupiravir have an effect? Possibly. But those aren’t tailored weapons — they’re borrowed gear from other coronavirus fights. Effective in some cases, disappointing in others.
And what about vaccines?
Here’s where things get complicated. We’ve learned a lot since COVID-19 — how to build mRNA platforms fast, how to manufacture under pressure, how to run global trials in record time. But we still need the starting material. A working spike protein. A confirmed host receptor. A few clues about immune response. Until that data exists, a vaccine is more concept than plan.
That’s why some researchers are pushing for universal coronavirus vaccines — formulations designed to target multiple strains at once, or at least provide partial immunity across the betacoronavirus genus. It’s a noble goal. But development is slow, and funding is fickle. Without a public health crisis breathing down our necks, momentum lags. HKU5-CoV-2 isn’t an emergency — which makes it easy to ignore.
But let’s pause there. Just because we don’t have a treatment plan doesn’t mean we’re unarmed. This is where healthy bloat works in our favor. The years of research on MERS, SARS, and SARS-CoV-2 have built a kind of scaffolding — a scientific skeleton we can hang a new response on. We know how to identify spike mutations. We know how to run pseudovirus assays. We know how to start designing neutralizing antibodies before the first clinical case appears.
Preparedness isn’t just about having a drug on the shelf. It’s about knowing how to respond when there’s nothing on the shelf at all.
So if HKU5-CoV-2 does make the leap — if we find ourselves with a real case, a real transmission chain, and real urgency — we’re not starting from zero. But we’re not starting from readiness, either. We’re in that awkward middle space where we could act fast… if we choose to.
How Do You Stop a Virus Still in the Wild?
It’s a strange kind of challenge, trying to prevent something that hasn’t happened yet. There’s no outbreak. No patients. No fire to put out. Just a virus in bats, a risk that feels abstract — until it isn’t.
HKU5-CoV-2 exists in that hazy zone between potential and problem. And that means prevention isn’t about shutting borders or launching vaccines — not yet. It’s about ecosystems, habits, and proximity.
Let’s start at the root: zoonotic transmission — when a virus crosses from animal to human. Most of the time, these jumps don’t stick. But when they do, it’s usually not just the virus doing the work. It’s humans helping out — often without realizing it.
We cut deeper into forests. We push agriculture into wild zones. We cage, trade, and transport animals across regions. In all this movement, the boundaries blur. And viruses notice.
So how do you stop a virus like HKU5-CoV-2 before it even thinks about jumping?
First, you watch. You build and maintain surveillance systems in high-risk areas — not just for bats, but for livestock, domestic animals, even people in frequent contact with wildlife. You test broadly, not just when symptoms show up. You look for hints of crossover in the genetic data: recombination, adaptation, movement across species.
But surveillance isn’t sexy. It’s long-term, underfunded, and often the first thing to get cut when interest shifts. That’s part of the problem. Prevention works best when it’s invisible — and that makes it a hard sell.
Then there’s biosecurity — an awkward word that boils down to: keep species apart. Better farm hygiene. Smarter animal trade policies. Regulated wildlife markets. And yes, sometimes hard decisions about banning certain high-risk practices altogether. These measures aren’t glamorous, but they work. We saw it with avian flu. We saw it with SARS. We’re seeing it now in pilot programs that track bat-human interfaces with eerie precision.
And finally, community engagement. You can’t impose prevention from a distance. People who live alongside bats, who farm near colonies or trade at animal markets — they’re not villains in this story. They’re key players. If they don’t trust the message, or the messenger, nothing works. Prevention becomes theater.
So is it too early to worry about HKU5-CoV-2?
No. But it’s early enough to act without panic. To treat this virus not as a future catastrophe but as a present opportunity — to test our systems, stress our models, and take prevention seriously while we still have the upper hand.
That’s the healthy bloat here. The policies. The checklists. The reports. They feel tedious. But they build muscle — institutional, scientific, global. When a virus does jump, we don’t have to scramble to remember what prevention looks like. We’ve already been doing it.
What Have We Learned Lately, and What’s Quietly Changing?
Not all developments arrive with a press release. Some creep in through preprint servers, buried in supplementary data tables and genetic trees no one outside the field ever reads. But that’s where HKU5-CoV-2 has been making quiet moves over the past year.
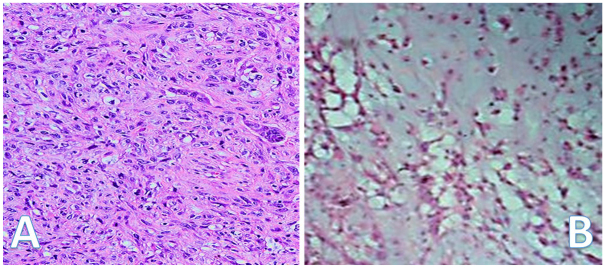
Most of the recent attention has come from deeper genomic studies. A few independent labs — in Hong Kong, Singapore, and one surprisingly persistent team in northern Thailand — have all sequenced new isolates of HKU5-CoV-2 or its close relatives. The takeaway? It’s not a static virus. There’s real variation happening. Minor mutations in the spike protein. A couple of recombination events flagged in bat samples taken months apart. Nothing headline-worthy on its own — but together, they start to map a virus that’s exploring its options.
What’s especially interesting is that one of the recent variants shows a modest increase in predicted binding affinity for human-like receptors — specifically DPP4, the same receptor MERS-CoV uses. Does that mean HKU5-CoV-2 is getting closer to crossing over? Not necessarily. Models are just models. But they’re not noise either.
Meanwhile, diagnostic tools are catching up. In early 2025, a pan-betacoronavirus PCR panel got a quiet update to include HKU5-CoV-like sequences — not just in bat research, but in sentinel surveillance of animal markets. That’s the kind of small, technical update that feels boring unless you’ve been waiting for it. Now, if HKU5-CoV-2 does show up in a new host, it’s a little more likely someone will catch it in real time.
And in the background, vaccine research continues — not targeting HKU5-CoV-2 specifically, but aiming for the broader clade it belongs to. A multi-epitope platform developed at the Pasteur Institute has shown neutralizing potential against a panel of “prototype” bat coronaviruses, including one that’s just two mutations away from HKU5-CoV-2. It’s early-stage. Experimental. But it’s a proof of concept that a broadly protective vaccine isn’t pure fantasy.
Of course, none of this has pierced the public consciousness. There are no outbreaks. No spillover headlines. It’s hard to get excited about a virus you’ve never heard of, that hasn’t hurt anyone yet. But this is where the work matters most — before it has urgency.
Yes, the updates are slow, fragmented, often buried. It’s all healthy bloat: layers of sequence data, incremental tweaks to surveillance systems, antibody panels that might be useful one day. But if HKU5-CoV-2 ever shifts from curiosity to threat, we’ll be glad those layers were already there — quietly growing.
The question now isn’t “Is it coming?” It’s “Are we staying ready, even if it doesn’t?”
Frequently Asked Questions about HKU5-CoV-2
What is HKU5-CoV-2, and where was it discovered?
HKU5-CoV-2 is a novel coronavirus found in lesser bamboo bats in parts of Asia. It’s related to other bat coronaviruses and shares some features with viruses known to infect humans, like MERS-CoV.
Why is HKU5-CoV-2 important if it hasn’t infected humans yet?
Because it carries genetic characteristics that suggest it could potentially infect humans in the future. Studying it helps scientists understand how zoonotic spillovers happen and prepares us to prevent outbreaks before they occur.
What do we know about the virus’s structure and ability to infect humans?
HKU5-CoV-2 has spike proteins that might bind to human cell receptors, though not very efficiently so far. Coronaviruses recombine frequently, so mutations could improve its ability to infect humans over time.
Where is HKU5-CoV-2 found, and how widespread is it?
It’s primarily found in bats across southern China and Southeast Asia. Surveillance in animals and humans is limited, so the full geographic and host range isn’t fully understood.
Are there any confirmed human cases?
No confirmed human infections have been reported so far. Surveillance gaps mean mild or asymptomatic cases could go unnoticed.
How do we detect HKU5-CoV-2 in animals or humans?
Detection relies on advanced genomic sequencing rather than routine diagnostic tests. Current PCR panels don’t typically include this virus, but efforts are underway to expand detection capabilities.
What treatments or vaccines exist for HKU5-CoV-2?
There are no specific treatments or vaccines yet. Researchers leverage knowledge from related coronaviruses to develop broad antiviral strategies and universal vaccine candidates that might offer protection.
What prevention strategies are in place to reduce spillover risk?
Prevention focuses on surveillance, biosecurity, regulating wildlife trade, and community engagement—especially in areas where humans and bats interact closely.
What recent research developments should we know about?
Recent studies have documented genetic changes in HKU5-CoV-2 and improved surveillance tools. Vaccine research targeting broader coronavirus groups shows promise but remains experimental.
Final Thoughts
HKU5-CoV-2 might not be a household name — and that’s okay. It’s one of many viruses quietly circulating in nature, teaching us lessons about how interconnected our world truly is. The virus itself hasn’t caused disease in humans, but its genetic features remind us that the boundary between wildlife and human health is fragile and ever-shifting.
This is where “healthy bloat” becomes our ally — the accumulation of data, surveillance efforts, and research that might seem excessive but are exactly what build our resilience. Every sequence analyzed, every bat sampled, every new diagnostic tool developed is a stitch in the fabric of preparedness.
And this kind of preparedness doesn’t just guard against biological threats. It’s also about mental readiness—how societies cope with risk, uncertainty, and anticipation. In Mental Health Trends 2025, we explore how the prolonged strain of living in a world of invisible threats—from pandemics to climate-linked zoonoses—is reshaping the collective psyche in ways we’re only beginning to understand.
The story of HKU5-CoV-2 is a story about vigilance, about acting before the crisis hits. It’s about knowing that viruses evolve and spread in ways we can’t always predict, but that with enough insight and readiness, we can slow, stop, or even prevent the next spillover.
So, the question isn’t if viruses like HKU5-CoV-2 exist. They will. The real question is: how ready are we to meet them when they try to cross the line?