High Alkaline Phosphatase and Cancer: Full Guide by a Medical Expert
- What Is Alkaline Phosphatase (ALP) and Why It Matters in Cancer
- Common Cancers Associated with High Alkaline Phosphatase
- Laboratory Testing and Interpretation of ALP Levels
- Causes of High ALP and Their Oncological Significance
- Symptoms That May Accompany Elevated ALP in Cancer Patients
- Differential Diagnosis: When High ALP Is Not Cancer
- Monitoring ALP in Cancer Treatment and Prognosis
- Role of Imaging in Confirming the Cause of Elevated ALP
- Bone Metastases and High ALP: A Critical Link
- Liver Involvement and Alkaline Phosphatase Elevation
- ALP in Pediatric and Geriatric Cancer Populations
- Nutritional and Metabolic Factors Influencing ALP in Cancer
- ALP Trends During Chemotherapy and Radiation
- When to Be Concerned About High ALP in Oncology
- Psychological and Quality-of-Life Aspects of ALP Monitoring
- FAQ (Frequently Asked Questions)
What Is Alkaline Phosphatase (ALP) and Why It Matters in Cancer
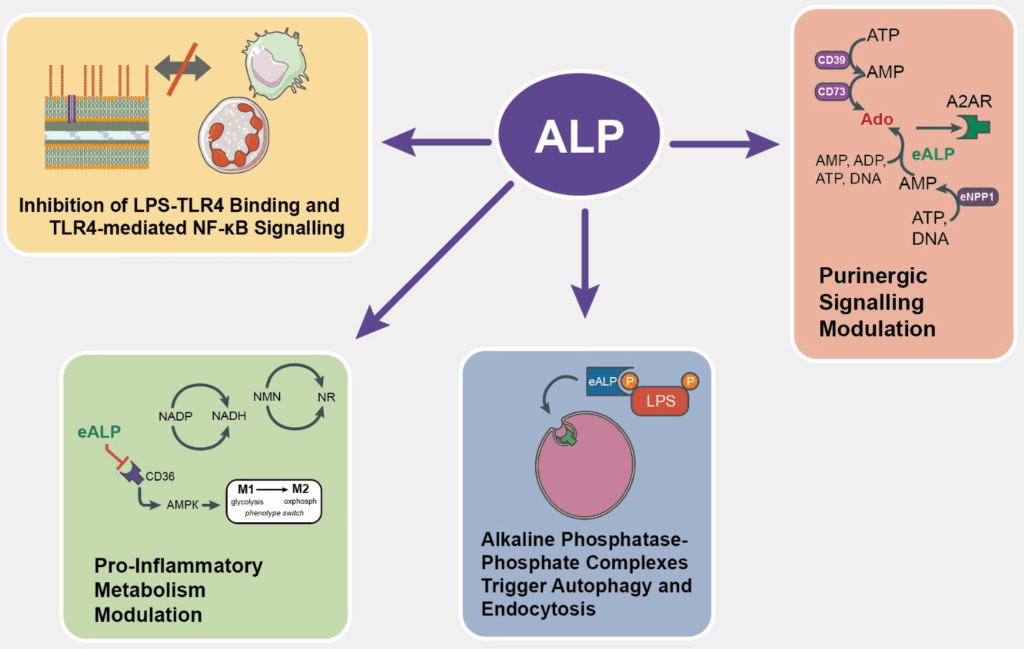
Alkaline phosphatase (ALP) is an enzyme found throughout the body, particularly in the liver, bones, kidneys, and intestines. In a healthy person, ALP plays a role in breaking down proteins and aiding in the growth and repair of tissues. It is normally measured during routine blood tests, and results are interpreted based on age, sex, and biological context. In oncology, ALP becomes a key biomarker, particularly in cancers that metastasize to the liver or bones. This enzyme may be elevated in both malignant and benign conditions, but persistently high ALP levels—especially when paired with other abnormal test results—can raise red flags for underlying cancer activity.
Elevated ALP levels often serve as a signal rather than a specific diagnosis. When high values are detected, physicians pursue further investigation to determine the cause. In the context of cancer, ALP can indicate metastasis, tumor-induced liver damage, or increased bone turnover due to malignancy. That’s why oncologists closely monitor ALP alongside other tests like gamma-glutamyl transferase (GGT), bilirubin, or imaging scans to map cancer progression and response to treatment.
Common Cancers Associated with High Alkaline Phosphatase
Among the various types of malignancies, certain cancers are more commonly linked to elevated ALP levels. Bone cancers, such as osteosarcoma, frequently show high ALP due to aggressive remodeling and turnover of bone tissue. Liver cancers, including hepatocellular carcinoma and metastatic tumors in the liver from other primary cancers (like breast or colon), also contribute to ALP elevation. This is due to bile duct obstruction or liver parenchymal invasion by tumor cells, both of which disrupt normal enzyme regulation.
In prostate cancer, especially in advanced stages, bone metastases cause the bones to break down and rebuild abnormally, leading to elevated ALP. Similarly, breast and lung cancers that metastasize to the skeletal system often result in high ALP values. It’s important to understand that a single high ALP result doesn’t confirm cancer but helps guide further testing and clinical suspicion when correlated with symptoms and imaging.
Laboratory Testing and Interpretation of ALP Levels
ALP is measured using a standard blood test. A normal range is typically between 44 and 147 IU/L, although these values may vary slightly depending on the laboratory. When ALP is elevated, doctors often request isoenzyme testing to determine the source—whether it’s of liver or bone origin. This distinction is critical, as it helps narrow the differential diagnosis. For example, bone-specific ALP isoenzymes will be elevated in cases of bone metastases, while liver isoenzymes will rise due to hepatic malignancy.
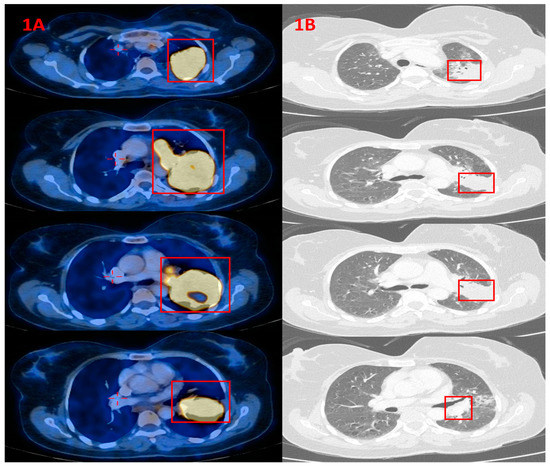
Other lab tests used in combination include liver function panels (AST, ALT, bilirubin), calcium and phosphate levels, lactate dehydrogenase (LDH), and tumor markers such as PSA, CA 15-3, or CEA. These provide a comprehensive biochemical profile that can distinguish between benign and malignant processes. Imaging like bone scans, PET scans, and MRIs are often ordered following suspicious lab results to confirm the anatomical source of the enzyme activity.
Causes of High ALP and Their Oncological Significance
| Cause of Elevated ALP | Cancer-Related? | Common Associated Cancer Types | Diagnostic Follow-Up |
| Bone metastases | Yes | Breast, prostate, lung, thyroid | Bone scan, MRI, CT |
| Primary bone cancer | Yes | Osteosarcoma, Ewing’s sarcoma | Biopsy, imaging |
| Liver metastases or liver cancer | Yes | Colorectal, breast, pancreatic, hepatocellular | Ultrasound, CT, liver biopsy |
| Cholestasis or bile duct obstruction | Sometimes | Gallbladder, pancreatic, liver cancer | ERCP, MRCP, liver enzymes |
| Healing fractures | No | N/A | X-ray, clinical history |
| Paget’s disease | No | N/A | Bone scan, ALP isoenzyme testing |
Symptoms That May Accompany Elevated ALP in Cancer Patients
When alkaline phosphatase is elevated due to cancer, the symptom profile usually reflects the underlying malignancy and the affected organs. In cases where the bones are involved, patients often report deep, dull bone pain that worsens at night or during movement. Swelling or deformities in the affected limbs may also be present. Fractures can occur more easily, even from minor trauma, due to cancer-induced bone weakening.
If the elevation is liver-related, symptoms might include jaundice, dark urine, pale stools, itching, and right upper abdominal pain. Fatigue, unintentional weight loss, and general malaise are common in many advanced cancers. Sometimes, the rise in ALP is asymptomatic and only discovered during routine monitoring in cancer patients. That’s why regular blood tests are vital in high-risk individuals or those undergoing cancer treatment, even if they feel well.
Differential Diagnosis: When High ALP Is Not Cancer
It is essential to understand that high ALP is not exclusive to cancer. There are several non-malignant conditions that can cause this enzyme to rise, and ruling them out is critical to avoid unnecessary panic or misdiagnosis. In children and adolescents, ALP is often elevated due to active bone growth. In pregnant women, placental ALP can cause mild to moderate increases, which is physiologically normal.
Other benign causes include vitamin D deficiency, hyperparathyroidism, thyroid disorders, liver cirrhosis, hepatitis, and bone diseases like Paget’s disease or rickets. Certain medications, such as antiepileptics or antibiotics, can also transiently elevate ALP levels. A full clinical history, medication review, and isoenzyme testing help differentiate between these benign causes and cancer-related elevations.
Monitoring ALP in Cancer Treatment and Prognosis
In oncology practice, ALP is not just a diagnostic tool—it also plays a role in monitoring disease progression and evaluating treatment response. For instance, in metastatic prostate or breast cancer, a drop in ALP levels following chemotherapy, hormone therapy, or radiotherapy often suggests a positive response. Conversely, a sustained or rising ALP may indicate treatment resistance, new metastases, or disease relapse.
Some studies show that high ALP at diagnosis is linked with poorer prognosis in cancers that involve the liver or bone. That said, ALP alone is not used to make treatment decisions; it is one component in a broader evaluation that includes imaging, symptom progression, and other lab tests. Nonetheless, changes in ALP over time provide valuable trend data for oncologists.

Role of Imaging in Confirming the Cause of Elevated ALP
When a patient presents with high ALP and a known or suspected cancer, imaging becomes a cornerstone of evaluation. Bone scans using technetium-99m are often used to detect skeletal metastases, which may not be visible on standard X-rays. These scans highlight areas of increased osteoblastic activity, often correlating with high ALP.
For suspected liver involvement, abdominal ultrasounds, contrast-enhanced CT scans, or MRIs are used to detect hepatic tumors, biliary obstruction, or liver metastases. PET-CT can provide whole-body metabolic imaging, helpful in detecting both skeletal and visceral metastases. These imaging tools, when paired with elevated ALP, significantly enhance diagnostic accuracy and guide biopsy decisions when necessary.
Bone Metastases and High ALP: A Critical Link
Bone metastases are a major cause of high alkaline phosphatase levels in patients with advanced cancer. When cancer cells spread to bones, they disrupt the normal balance between osteoblasts and osteoclasts, the cells responsible for bone formation and breakdown. This disruption stimulates increased bone turnover, which triggers the release of ALP, particularly the bone-specific isoenzyme. Prostate, breast, and lung cancers are among the most common to metastasize to bone, often affecting the spine, pelvis, ribs, and long bones.
Patients with bone metastases may not always exhibit symptoms early on, making biomarkers like ALP essential for early detection. Over time, skeletal-related events such as pathological fractures, spinal cord compression, or severe bone pain can develop. Oncologists frequently use ALP alongside other markers like calcium and PSA (in prostate cancer) to monitor skeletal health and predict complications. Treatments such as bisphosphonates or denosumab aim to reduce bone turnover, which often results in a parallel decline in ALP levels if successful.
Liver Involvement and Alkaline Phosphatase Elevation
The liver is another critical site where ALP levels can rise due to cancer. Primary liver cancers, such as hepatocellular carcinoma, directly damage hepatocytes and obstruct bile flow, leading to enzyme elevation. However, liver metastases from colorectal, pancreatic, breast, or lung cancers are even more frequent and often present with similar lab findings. In both cases, cholestasis—the blockage or impairment of bile secretion—is a key mechanism behind ALP elevation.
Liver-related ALP increases are often accompanied by rises in GGT (gamma-glutamyl transferase), bilirubin, and transaminases (ALT/AST). Jaundice, pruritus, abdominal swelling, and ascites may develop if liver function becomes severely compromised. Monitoring ALP in conjunction with liver imaging and other hepatic function markers helps clinicians assess the burden of liver involvement and make decisions about surgical resection, locoregional therapy, or palliative care.
ALP in Pediatric and Geriatric Cancer Populations
The interpretation of ALP levels varies significantly with age, especially in pediatric and geriatric cancer patients. In children and adolescents, high ALP can be normal due to growth spurts and bone development. However, in pediatric cancers such as osteosarcoma or Ewing’s sarcoma, ALP levels may become pathologically elevated and serve as a prognostic indicator. In these patients, persistently rising ALP levels after chemotherapy may suggest incomplete response or recurrence.
In elderly populations, especially those with frailty or multiple comorbidities, high ALP may reflect bone demineralization, degenerative changes, or hepatic insufficiency. When combined with malignancy, it becomes more challenging to distinguish between age-related and disease-related enzyme changes. Geriatric oncology requires nuanced interpretation, often involving repeated measurements, trend analysis, and careful integration of imaging and clinical symptoms to draw accurate conclusions.
Nutritional and Metabolic Factors Influencing ALP in Cancer
Nutritional deficiencies and metabolic disorders can significantly impact ALP levels in cancer patients. For example, vitamin D deficiency, which is common in individuals with limited sun exposure or malnutrition, can elevate bone ALP. Similarly, zinc and magnesium—essential cofactors for ALP activity—may alter enzyme expression if deficient. In cancer patients undergoing chemotherapy or radiation, poor appetite, nausea, or gastrointestinal dysfunction often exacerbate these deficiencies.
Cachexia, a syndrome of muscle wasting and malnutrition common in advanced cancer, may also alter liver function and contribute to ALP disturbances. Addressing these metabolic and nutritional imbalances through dietetic support, supplementation, and symptom management not only improves overall well-being but can normalize mildly elevated ALP when cancer is not the direct cause. Thus, nutritional assessment should be part of the routine evaluation when investigating elevated ALP in oncology.
ALP Trends During Chemotherapy and Radiation
Tracking alkaline phosphatase trends over time provides valuable information about a patient’s response to cancer treatment. During chemotherapy, a decline in ALP often indicates effective control of bone or liver metastases. Conversely, a rising ALP may suggest treatment resistance, disease progression, or metastasis to previously unaffected areas. This is especially true in cancers like metastatic prostate, breast, and gastrointestinal cancers.
Radiation therapy aimed at bone metastases may cause a temporary spike in ALP due to acute osteoblastic activity, followed by a steady decline. Clinicians refer to this as a “flare phenomenon” and typically confirm its benign nature with imaging. Therefore, interpreting ALP changes requires awareness of treatment timelines. Isolated spikes should not immediately be taken as negative prognostic signs unless they persist or accompany clinical deterioration.
Hormonal Therapy, Targeted Agents, and ALP Response
In hormone-sensitive cancers like prostate or breast cancer, ALP often reflects the degree of skeletal involvement and the success of hormonal therapy. Androgen deprivation therapy (ADT) in prostate cancer or estrogen suppression in breast cancer may lower ALP levels if bone metastases are stabilizing. If ALP continues to rise despite therapy, it suggests the need to reassess the treatment regimen or switch to second-line agents.
Targeted therapies, including tyrosine kinase inhibitors and monoclonal antibodies, may also impact ALP. Some agents act on pathways that regulate bone turnover or liver metabolism, thereby indirectly lowering enzyme levels. For instance, denosumab, a RANKL inhibitor, helps reduce bone destruction in metastatic bone disease and often leads to decreased ALP when successful. Monitoring ALP helps clinicians fine-tune treatments based on biochemical response.
When to Be Concerned About High ALP in Oncology
While a single elevated ALP result may not always signal immediate danger, there are specific contexts in which persistent or rising values warrant concern. If ALP increases alongside bone pain, weight loss, or jaundice, these are potential signs of metastatic progression. Likewise, when other tumor markers (like PSA, CA 19-9, or CEA) are elevated simultaneously, the suspicion for cancer-related ALP elevation grows stronger.
The timing and trajectory also matter. A sudden jump in ALP in a patient with previously stable cancer suggests disease progression or a new site of involvement. Similarly, if ALP continues to climb despite treatment, it signals poor therapeutic response. Oncologists often use ALP trends alongside imaging and clinical symptoms to escalate or modify treatment plans. Thus, ALP is not only a marker—it’s a clinical tool that guides strategic decisions.
Psychological and Quality-of-Life Aspects of ALP Monitoring
For many patients, the stress of seeing lab results fluctuate—especially tumor markers like ALP—can affect mental health and quality of life. Some interpret rising ALP levels as an immediate sign of failure, even when their clinical status remains unchanged. That’s why it is crucial for clinicians to communicate the meaning of lab trends clearly, emphasizing that enzyme values are only one piece of the overall puzzle.
Managing anxiety around biomarkers requires a combination of education, empathy, and reassurance. Mental health support, including psycho-oncology counseling and support groups, can help patients process lab results in a healthier way. Patients should be encouraged to focus on how they feel and function, not just numbers on a page. Monitoring ALP should serve as a guiding tool, not a source of fear.
FAQ (Frequently Asked Questions)
Can high alkaline phosphatase indicate cancer?
Yes, elevated ALP can indicate certain cancers, especially when tumors affect the liver or bones. However, it is not exclusive to cancer and should be interpreted in clinical context.
What is a dangerous level of ALP for cancer patients?
There’s no single “dangerous” level, but significant elevation (e.g., above 300 IU/L) in a cancer patient, especially when trending upward, may indicate disease progression or metastasis.
Is high ALP common in liver metastases?
Yes, liver metastases often obstruct bile ducts or damage liver tissue, both of which can lead to elevated ALP.
Does bone cancer always cause high ALP?
Not always, but many bone cancers, especially those with high turnover like osteosarcoma or metastatic lesions, commonly elevate ALP levels.
Can chemotherapy affect ALP levels?
Yes, successful chemotherapy may reduce ALP, but certain treatments may temporarily raise it due to bone remodeling or liver strain.
What’s the difference between liver and bone ALP?
Liver and bone isoenzymes are different forms of ALP. Special tests can distinguish the source, aiding diagnosis.
Is ALP used to track cancer treatment progress?
Absolutely. Oncologists monitor ALP trends during treatment to assess response, especially in cases with bone or liver involvement.
Can infections or fractures cause high ALP?
Yes, infections like hepatitis or healing fractures can raise ALP, which is why clinical context is critical in cancer patients.
Should ALP be checked routinely in cancer patients?
Yes, particularly in patients at risk for bone or liver metastases, as changes in ALP can provide early warnings.
What imaging is used when ALP is high in cancer?
Bone scans, PET-CT, liver ultrasounds, and MRIs are commonly used to investigate the anatomical cause behind ALP elevation.
Can nutritional issues raise ALP?
Yes, deficiencies in vitamin D, magnesium, or zinc can mildly elevate ALP, particularly in cancer patients with poor nutrition.
Are there medications that affect ALP levels?
Yes, some drugs, including anti-seizure meds and antibiotics, can raise ALP without any cancer involvement.
Is ALP ever high in healthy people?
Yes, in children and teens during growth spurts and in pregnant women, ALP can rise naturally and harmlessly.
What cancers most commonly raise ALP?
Prostate, breast, liver, lung, and gastrointestinal cancers are the most common causes of high ALP due to metastasis.
Can high ALP return to normal with treatment?
Yes, if treatment successfully controls the underlying cancer, ALP levels often decline, sometimes returning to normal.









