Hand Numbness in Brain Tumor Patients
Hand Numbness in Brain Tumor Patients: Causes, Risks, and What to Do
- Why Does Hand Numbness Happen in Brain Tumor Patients?
- Neurological Mechanism Behind Hand Numbness in Brain Cancer
- How Common Is Hand Numbness Among Brain Tumor Patients?
- Statistics and Clinical Patterns Based on Tumor Type and Stage
- Why Does This Symptom Arise: Underlying Causes Behind Hand Numbness
- Red Flags: When Hand Numbness Requires Urgent Attention
- Diagnostic Approach: How Doctors Investigate Hand Numbness
- Managing Hand Numbness: Treatment Options That Help
- Can This Symptom Be Prevented in Brain Tumor Patients?
- Does It Go Away? Understanding the Prognosis of Numbness
- Insights from Oncologists: What Experts Say
- 15+ Questions to Ask Your Doctor About Hand Numbness
Why Does Hand Numbness Happen in Brain Tumor Patients?

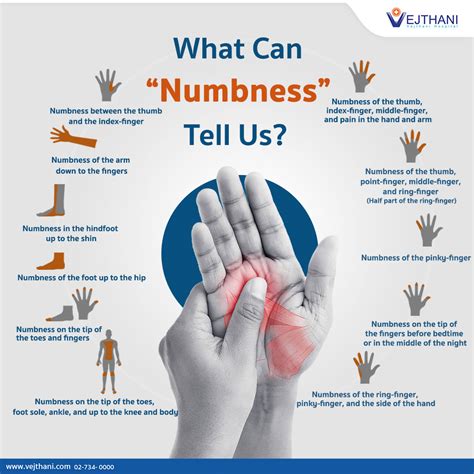
Hand numbness in individuals with brain tumors is a neurological symptom often related to the tumor’s impact on brain structures or surrounding tissues. This numbness typically presents as a tingling, pins-and-needles sensation, or a complete loss of sensation in the fingers, palm, or entire hand. The sensation may appear gradually or suddenly, depending on the tumor’s growth and location.
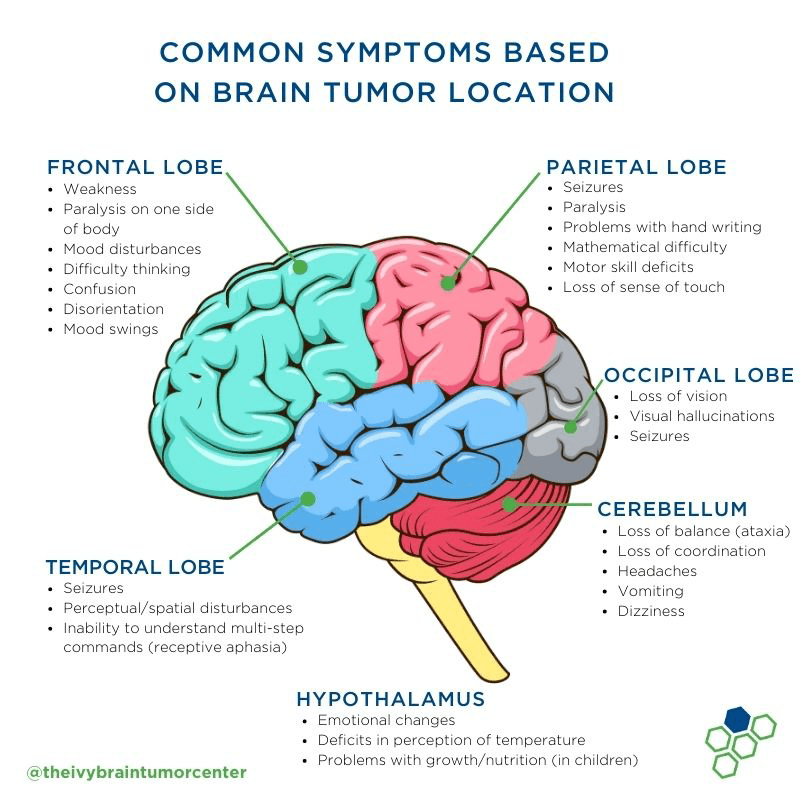
In many cases, tumors situated near the sensory cortex or along the motor-sensory pathways—particularly in the parietal lobe or brainstem—can directly interfere with nerve signal transmission to the hands. This results in misfiring of sensory input or complete sensory block. Patients sometimes describe the feeling as wearing a tight glove or a frozen hand. This can also coexist with weakness or clumsiness.
Neurological Mechanism Behind Hand Numbness in Brain Cancer
When a tumor forms in the brain, especially in areas responsible for sensory processing or motor control, it can cause pressure, inflammation, or damage to nerve pathways. These pathways—such as the corticospinal tract or spinothalamic tract—carry signals from the brain to the spinal cord and then to the peripheral nerves in the limbs.
In brain tumor patients, hand numbness may result from:
- Direct compression of sensory brain regions
- Disrupted blood supply due to tumor pressure or edema
- Surgical intervention impacting adjacent nerves
- Side effects from radiation or chemotherapy
In rare cases, numbness is a paraneoplastic syndrome—a remote effect of cancer that involves immune-mediated nerve dysfunction. Chemotherapy-induced peripheral neuropathy (CIPN) can also contribute if the brain tumor is part of a broader cancer diagnosis being treated systemically.
How Common Is Hand Numbness Among Brain Tumor Patients?
Hand numbness is not universally present but is a known symptom in a significant portion of brain tumor cases. Its frequency depends heavily on the tumor’s location, size, and growth pattern. Tumors affecting the sensory cortex or thalamus are more likely to cause numbness than those in frontal or occipital lobes.
Based on clinical reports:
| Tumor Location | % of Patients Reporting Numbness |
| Parietal Lobe | 35–50% |
| Brainstem or Cerebellum | 20–30% |
| Motor Cortex | 15–25% (often paired with weakness) |
| Diffuse Gliomas | 10–15% |
These symptoms may be more frequent in advanced stages or when tumors are aggressive, such as glioblastomas. In rare cases, numbness in the hands may be the first sign of a deeper neurological issue, leading to the initial discovery of the tumor.
Statistics and Clinical Patterns Based on Tumor Type and Stage
Clinical observations indicate a strong correlation between the stage and location of brain tumors and the appearance of sensory symptoms like hand numbness. In early-stage tumors confined to small regions, numbness may be subtle or absent. However, as the tumor enlarges or metastasizes, the chances of affecting adjacent nerve tissue increase.
For example, in high-grade gliomas or metastatic brain tumors, hand numbness may present alongside balance problems, headaches, or cognitive decline. In comparison, slow-growing benign tumors like meningiomas may only cause symptoms after significant compression of brain tissue.
There’s also a notable difference in symptom presentation between adult and pediatric patients. Adolescents and young adults often report more focal numbness with high-grade tumors, whereas elderly patients might show diffuse symptoms due to age-related brain atrophy.
Moreover, patients with underlying neurological diseases, such as multiple sclerosis, may experience exacerbated hand numbness, complicating the differential diagnosis.
Why Does This Symptom Arise: Underlying Causes Behind Hand Numbness
The appearance of hand numbness in patients with brain tumors can stem from a range of underlying triggers—neurological, oncological, metabolic, and pharmacological. Each plays a distinct role in the development and persistence of this symptom.
Tumor-related factors include direct invasion or pressure on the parietal cortex (which governs sensory input) or tumor-induced ischemia affecting nearby vessels. As the tumor expands or causes swelling (edema), it can compress white matter tracts responsible for relaying signals from the hand to the brain.
Therapy-related causes are equally significant. Radiotherapy to the brain can lead to delayed radiation-induced neuropathy. Chemotherapeutic agents—especially platinum-based drugs and vincristine—can cause peripheral nerve damage that presents as glove-like numbness.
In some cases, patients with brain metastases from systemic cancers (such as breast or lung cancer) experience numbness due to combined peripheral and central nervous system compromise.
Metabolic issues, like low vitamin B12, elevated calcium, or paraneoplastic syndromes, may also mimic or worsen sensory changes, adding complexity to the clinical picture.
Red Flags: When Hand Numbness Requires Urgent Attention
While numbness alone is often benign or manageable, there are scenarios where it becomes a red flag demanding immediate investigation:
- Rapid progression or spread of numbness beyond the hand
- Numbness paired with new weakness, slurred speech, or vision changes
- Sudden onset after trauma or seizure
- Loss of coordination or falling objects from the hand
- Worsening numbness during steroid withdrawal
If these signs are observed, it could indicate tumor growth, hemorrhage, increased intracranial pressure, or infarction. Emergency neuroimaging is essential in such cases.
These warning signs are especially concerning in patients already diagnosed with Brain Cancer in Dogs, Brain Cancer in Cats, or other neurological malignancies that demonstrate similar symptom progression in veterinary or comparative models, aiding human diagnostics.
Diagnostic Approach: How Doctors Investigate Hand Numbness
To uncover the exact cause of hand numbness in a brain tumor patient, physicians rely on a combination of imaging, neurological exams, and lab work. The diagnostic roadmap often looks like this:
| Diagnostic Method | Purpose |
| Brain MRI with contrast | Identify tumor location, size, and edema |
| Functional MRI (fMRI) | Assess activity in sensory cortex |
| Electromyography (EMG) | Evaluate peripheral nerve involvement |
| Nerve conduction studies | Distinguish between central and peripheral damage |
| Blood tests (B12, calcium, CRP) | Rule out metabolic contributors |
In ambiguous cases, lumbar puncture may be conducted to assess cerebrospinal fluid for cancer cells or paraneoplastic antibodies. If numbness is suspected to be post-treatment related, imaging may also include DTI (diffusion tensor imaging) to detect nerve tract disruptions.
Managing Hand Numbness: Treatment Options That Help
Treatment depends on whether the numbness is tumor-related, treatment-induced, or secondary to metabolic causes. Here are the main approaches used in clinical settings:
Medication adjustments are often the first step. If chemotherapy is the suspected cause, dose reduction or a switch to a less neurotoxic agent may help. For inflammation-related compression, corticosteroids like dexamethasone can reduce swelling and restore some sensation.
Physiotherapy and occupational therapy play a vital role in improving hand function, especially if fine motor skills are affected. Adaptive tools and sensory re-education techniques are frequently used.
Neuropathic pain medications such as gabapentin or pregabalin may be prescribed if numbness is accompanied by burning or discomfort.
In patients with severe progressive symptoms, surgical intervention (such as tumor debulking or stereotactic radiosurgery) may relieve the pressure causing the numbness. Collaboration between neurologists, oncologists, and physical therapists ensures tailored, symptom-specific care.
Can This Symptom Be Prevented in Brain Tumor Patients?
While complete prevention of hand numbness in brain tumor cases is not always possible, certain proactive strategies can reduce the likelihood or severity of the symptom.
Early tumor detection and timely treatment are critical. When tumors are identified before they grow large enough to compress neurological structures, numbness and other sensory deficits may never occur. Regular neuroimaging, especially in high-risk patients or those with genetic predispositions, supports this approach.
Lifestyle interventions can also reduce risk. Adequate hydration, balanced electrolytes, and vitamin sufficiency (especially B-complex and magnesium) help keep peripheral nerves healthy. Preventing metabolic complications, like diabetes or renal dysfunction, also plays a key role.
For patients undergoing chemotherapy, oncologists often modify dosage or use neuroprotective agents such as glutamine or calcium/magnesium infusions to mitigate nerve damage.
Finally, incorporating gentle physical activity, hand stretching, and tactile stimulation early in treatment plans can help maintain neural connections and reduce the onset of long-term numbness.
Does It Go Away? Understanding the Prognosis of Numbness
The persistence or resolution of hand numbness in brain tumor patients varies depending on the underlying cause and stage of cancer. The table below outlines typical scenarios:
| Underlying Cause | Prognosis |
| Tumor compression with early treatment | Often reversible after surgery or radiotherapy |
| Chemotherapy-induced neuropathy | May improve post-treatment; can be partially permanent |
| Radiation-induced nerve damage | Often delayed onset and may be long-lasting |
| Metabolic contributors (e.g., B12 deficiency) | Usually reversible with supplementation |
In advanced stages or if numbness results from permanent neural damage, it may persist for life. In such cases, symptom management becomes the focus. However, when detected and treated early, especially in low-grade gliomas or operable tumors, patients often regain full or partial sensation over time.
This is also supported by long-term follow-up studies of patients included in Cancer Symptoms in 2025, which highlighted the variability and patient-specific recovery trajectory of sensory loss symptoms, particularly in the hands.
Insights from Oncologists: What Experts Say
Practicing neuro-oncologists emphasize that hand numbness should never be dismissed, even if it seems minor. It is often one of the earliest signs that a tumor is expanding or exerting new pressure on critical structures.
Experts recommend routine sensory exams, even in asymptomatic patients, especially those being treated for glioblastoma, astrocytoma, or metastatic cancers. Functional impairments like hand numbness can guide treatment adjustments before more severe symptoms emerge.
They also advocate for early referral to physiotherapy and hand therapy, rather than waiting until numbness impairs daily activities. Collaboration with neurologists is essential when the source of numbness is uncertain or appears unrelated to known tumor growth.
According to neurology-oncology specialists, the most favorable outcomes are achieved through a multidisciplinary approach—oncology, neurology, rehabilitation, and nutrition—especially when the symptom is addressed early.
15+ Questions to Ask Your Doctor About Hand Numbness
1. What might be causing my hand numbness in relation to my brain tumor?
The doctor can explain whether it’s due to the tumor, treatment, or another issue like vitamin deficiency.
2. Is this symptom temporary or likely to be permanent?
This depends on whether the affected nerves are only compressed or already damaged.
3. Should we change or pause my current treatment because of this symptom?
Your team may need to modify medications or radiation to protect nerve health.
4. Are there any supplements or medications that can help relieve the numbness?
Some patients benefit from vitamins, anti-neuropathic drugs, or metabolic support.
5. Could this be a sign of the tumor growing or returning?
New or worsening numbness can sometimes indicate progression.
6. Do I need additional scans or neurological tests?
MRI, EMG, or nerve conduction studies might be necessary.
7. Should I see a neurologist or specialist?
Referral to a neurologist can help clarify the cause and guide therapy.
8. Will physical or occupational therapy help in my case?
Hand therapy can be very effective in managing numbness and loss of function.
9. Is there a risk of the numbness spreading or worsening?
If left untreated, the underlying issue might cause broader deficits.
10. Could this numbness affect my ability to perform daily tasks or work?
Doctors can evaluate risk and provide tools or support if needed.
11. What warning signs should I watch for in addition to numbness?
Look for new weakness, speech changes, or coordination problems.
12. How often should I report changes in this symptom to my care team?
Regular updates help the team adjust care appropriately.
13. Are there alternative therapies I can try safely?
Massage, acupuncture, and low-level laser therapy may offer relief in some cases.
14. Does numbness mean my treatment isn’t working?
Not necessarily—side effects sometimes occur even when treatment is effective.
15. What’s the long-term outlook for this symptom in my specific case?
Your prognosis depends on tumor type, location, and your body’s response to treatment.












