Fungating Breast Tumors: Appearance, Symptoms, and Management
Foreword
A diagnosis of fungating breast cancer is something many never expect to hear, and understandably, it can be both shocking and overwhelming. The term “fungating” can sound frightening, and when it’s paired with an advanced stage of breast cancer, it can feel even more so. But it’s important to remember that even in these challenging circumstances, there is help — both medically and emotionally — and there are ways to manage the symptoms, ease discomfort, and maintain your quality of life.
Fungating tumors occur when breast cancer grows to a point where it breaches the skin, creating painful and often visible open sores. They can be distressing, both physically and emotionally, but they are manageable with the right care. In this article, we’re going to break down everything you need to know about these tumors: how they look, what symptoms they bring, how to manage them, and most importantly, how to live your life to the fullest while managing a diagnosis like this.
We’ll dive into the appearance and physical symptoms, discuss ways to handle the emotional impact, and explore the treatment options that can make a difference. Whether you’re facing this directly or supporting a loved one, our goal is to provide information that not only informs but empowers you.
Let’s get started with the basics: what exactly is a fungating breast tumor?
Part 1: What Are Fungating Breast Tumors?
Fungating breast tumors are a manifestation of advanced breast cancer. They are characterized by ulceration or open wounds that form when the tumor outgrows its blood supply and spreads to the skin. These tumors, although relatively rare, occur in a small but significant percentage of breast cancer patients, typically in the later stages when cancer cells have invaded surrounding tissues and the skin.
Understanding Fungating Tumors
A fungating tumor is a cancerous mass that breaches the skin, creating an open ulcer. These tumors develop as the cancer grows more aggressively, outpacing the ability of the surrounding blood vessels to nourish the tumor cells. Without a sufficient blood supply, areas of the tumor die, resulting in necrosis. As the tumor continues to expand, the dead tissue becomes exposed, leading to a wound that may ooze fluid or even bleed.
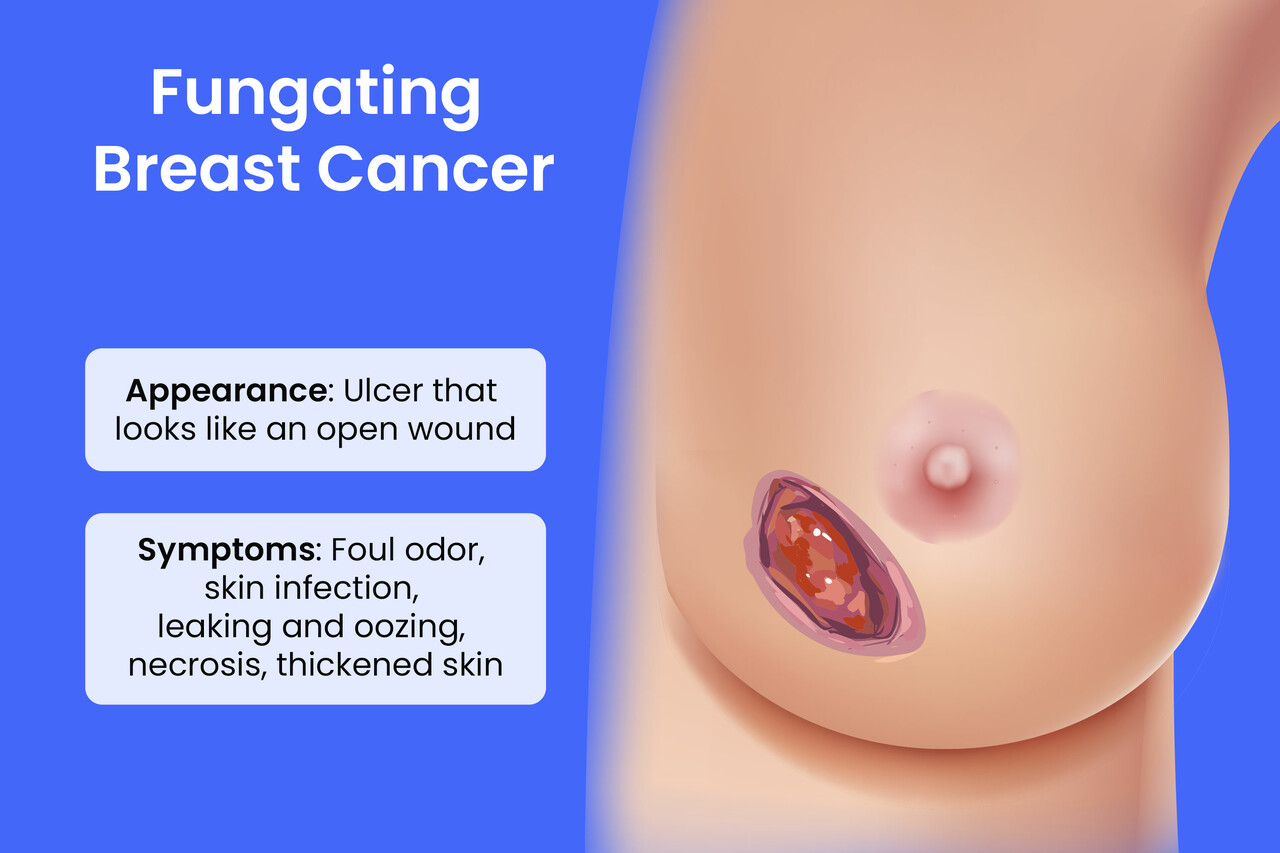
The appearance of a fungating breast tumor can vary depending on its size and location. These tumors often appear as raised masses, which may have irregular, jagged edges. Over time, they may become painful, discolored, and unpredictable in shape. The wound may produce foul-smelling discharge, which can be distressing for the patient.
Why Do Fungating Tumors Occur?
Fungating tumors typically occur in advanced stages of breast cancer when the tumor has reached a size and level of aggressiveness that makes it more likely to invade surrounding tissues, including the skin. The primary cause behind the development of a fungating tumor is tumor necrosis — the dying of cancer cells within the tumor mass. As the tumor cells outgrow their blood supply, parts of the tumor die off, leading to the open, ulcerated wound characteristic of fungating tumors.
In many cases, these tumors develop in larger, undiagnosed tumors that have not been treated early, leading to local invasion of the skin and surrounding tissue. The tissue surrounding the tumor can also become inflamed and ulcerated as the cancer grows and breaks through the skin’s surface.
Visual Characteristics of Fungating Tumors
The visual appearance of a fungating breast tumor is often alarming for patients and loved ones. As the tumor grows, the exposed area becomes raised, often with an uneven surface. The skin may appear red, ulcerated, and sometimes bleeding, with discharge oozing from the wound. The size of the tumor varies, but larger fungating tumors often spread over a wider area of skin, making them more difficult to manage.
One of the most challenging aspects of a fungating tumor is the odor that often accompanies it. Due to the open wound and potential for bacterial infection, the smell can be difficult to control, adding to the physical and emotional burden of the patient. This odor is a result of necrotic tissue and bacteria growing in the exposed wound.
The Stage of Cancer at the Time of Diagnosis
Fungating tumors are usually a sign of advanced-stage cancer, often diagnosed when the cancer has spread locally or has already metastasized to other organs. By the time a tumor reaches the fungating stage, it is usually indicative of Stage 3 or Stage 4 breast cancer, where the cancer has outgrown its primary location and begun to invade surrounding tissues, including the skin.
Because the presence of a fungating tumor indicates that the cancer is at a later stage, it is often accompanied by additional symptoms of metastasis, such as pain, swelling, and other systemic signs of disease progression.
Part 2: Symptoms of Fungating Breast Tumors
Dealing with a fungating breast tumor can bring up a lot of questions and understandably, concerns. Beyond the physical symptoms, there’s the emotional impact — it’s hard to ignore that visible wound, and the discomfort it brings. But here’s the thing: while these tumors are certainly challenging, there are practical ways to manage the symptoms and support your well-being.
1. Physical Symptoms of Fungating Tumors
Pain
Pain is one of the most common and difficult symptoms when living with a fungating tumor. As the tumor grows, it can put pressure on the skin and nearby tissues, leading to irritation. The exposed tissue can also become inflamed, which adds to the discomfort.
The good news is that pain management is something doctors take seriously. There are options like pain-relieving creams, oral pain medications, and even radiation therapy aimed at shrinking the tumor and reducing pain. While some patients experience only mild discomfort, others may need a more aggressive pain management plan. Your healthcare team will work with you to find the best strategy.
Swelling and Bleeding
A fungating tumor can often cause swelling around the area, as it may block lymphatic drainage or blood flow. This can lead to fluid buildup, making the area feel tender and swollen.
There’s also the possibility of bleeding, especially if the tumor is large or the skin around it is fragile. This can be frightening at first, but it’s another symptom that can be managed with proper care. Regular wound care, dressings, and medications can help control bleeding and minimize any additional risks.
Discharge and Odor
The presence of a fungating tumor means that the tumor’s cells are necrotic — they’re dying off, and that leads to an open wound that might ooze fluid or pus. This fluid can often have a strong odor, which can be upsetting, especially when the tumor is near a visible area like the chest.
Managing odor is absolutely possible. Regular wound care and antiseptic dressings are key. It’s also possible to find odor-controlling products designed specifically for situations like this. It’s all about keeping the wound clean, dry, and properly dressed.
Infection
Open wounds are at risk of infection due to exposure to the environment. Fungating tumors are especially vulnerable, and infection can make symptoms worse. Antibiotics and topical treatments can help treat infections and prevent them from spreading.
Your healthcare team will keep a close eye on the area to help reduce the risk of infection. It’s also important to check for signs of infection — increased redness, warmth, or drainage — and communicate any changes to your doctor right away.
2. Psychological and Emotional Impact
Body Image and Self-Esteem
One of the toughest aspects of having a fungating tumor is the emotional toll it can take. You might feel embarrassed or self-conscious about the way the wound looks, especially if it’s visible to others. It’s important to acknowledge that your feelings are valid. The physical changes can be unsettling, and it’s okay to feel a sense of loss or discomfort about your appearance.
Talking to your doctor about ways to manage both the physical symptoms and emotional toll is crucial. And don’t forget, there are support groups and mental health professionals who specialize in helping patients navigate the emotional side of cancer. You’re not alone in this.
Social Isolation and Stigma
The presence of a visible wound can sometimes lead to social isolation, as patients may feel reluctant to go out or interact with others. It’s common to feel self-conscious about how the tumor might be perceived by others. However, social support is a critical part of your recovery and well-being. Don’t hesitate to reach out to loved ones, support networks, or professional counselors who can help.
Overcoming the stigma around visible wounds starts with open communication. The more you allow others to understand what you’re going through, the more support they can offer.
Anxiety About Disease Progression
When faced with a fungating tumor, it’s natural to feel concerned about the spread of cancer and what the future holds. Anxiety about disease progression is a common response. Patients often worry about recurrence, treatment effectiveness, and their long-term prognosis.
Talking openly with your healthcare team about your concerns and questions can help alleviate some of this anxiety. They’ll help you understand what’s happening with your cancer and guide you through the treatment options that can provide relief. It’s also helpful to practice mindfulness techniques or consider speaking with a mental health professional to ease anxiety.
3. Impact on Daily Life
Fungating tumors can significantly impact daily routines. With pain, swelling, and discharge to manage, simple tasks like dressing, eating, or even sleeping can become more difficult. But the key is finding ways to make these activities easier.
Managing a fungating tumor often requires additional care and assistance, especially with wound dressing changes and maintaining personal hygiene. Having someone to help you with these tasks, or hiring a home care nurse to assist with care, can reduce the burden and allow you to focus on your well-being.
Fatigue and Nutritional Concerns
Fatigue can be a big challenge when living with a fungating tumor. The energy your body expends fighting the cancer, managing pain, and dealing with wound care can leave you feeling drained. Add to that the emotional weight of a visible tumor, and it’s no surprise that many patients feel worn out.
Nutritional support is also essential. When pain makes eating difficult or when chemotherapy leaves you feeling nauseous, maintaining good nutrition is even more important. A nutritionist can help you plan meals that are both easy on the stomach and rich in the nutrients you need to stay strong.
Part 3: Managing Fungating Breast Tumors
When it comes to managing fungating breast tumors, the goal isn’t just to address the tumor itself but to improve quality of life and symptom relief. Fungating tumors present several challenges, from managing pain and discomfort to dealing with the visible and emotional impact of the tumor. However, there are multiple approaches to symptom control, pain management, and wound care that can make a significant difference.
In this section, we’ll explore the key strategies for managing fun gating tumors effectively, including wound care, pain relief, infection control, and psychosocial support.
1. Wound Care and Hygiene
Proper wound care is essential in managing fungating breast tumors, not only to control the symptoms but also to prevent infection, reduce odor, and promote healing where possible. The open nature of the wound makes it vulnerable to bacteria, so keeping the wound clean and protected is critical.
Regular Wound Cleaning
The first step in proper wound care is regular cleaning of the tumor site to prevent infection. It’s important to use mild antiseptic solutions (such as saline or iodine-based cleansers) that won’t irritate the skin further. Cleaning the area gently, avoiding scrubbing, can help reduce the risk of spreading infection and minimize additional pain or irritation.
Dressing Changes
Dressings are a cornerstone of effective wound management. Fungating tumors require absorbent dressings that can manage the discharge from the tumor and help control odor. Hydrocolloid dressings, alginate dressings, and foam dressings are commonly used to absorb excess fluid and maintain a moist healing environment. Foam dressings are particularly effective in managing large amounts of exudate and controlling odor, while hydrocolloid dressings help reduce pain and keep the wound moist for faster healing.
Dressings should be changed regularly (usually once a day or more frequently, depending on the amount of discharge). It’s important that healthcare professionals or wound care specialists guide the patient or their caregivers in proper dressing change techniques.
Managing Odor
Odor management is a particularly challenging symptom when dealing with fungating tumors. The odor often results from necrotic tissue (dead tissue) and bacteria in the wound. Fortunately, there are several ways to manage this symptom:
- Charcoal dressings or odor-absorbing products can be placed over the wound to absorb and neutralize unpleasant smells.
- Antibiotic ointments or antiseptic creams can help treat or prevent infection, further reducing the odor caused by bacteria.
- Odor-neutralizing products like sprays or pads can also be used as part of a more holistic approach to managing smell.
2. Pain Management
Pain is one of the most difficult symptoms to manage with fungating tumors, as the open wound can cause both local pain and referred pain in surrounding tissues. Effective pain management is essential for improving quality of life and comfort.
Topical Analgesics
Topical treatments can be highly effective in controlling pain at the wound site. These include topical analgesic creamsand local anesthetics, such as lidocaine, which can numb the area and reduce pain during dressing changes. Applying a pain-relieving cream directly to the wound can provide temporary relief, although this should be used under the guidance of a healthcare professional.
Systemic Pain Relief
In more severe cases, oral pain medications like NSAIDs (nonsteroidal anti-inflammatory drugs) or opioids may be prescribed to manage pain. For many patients, these medications are effective at controlling discomfort, though care should be taken to adjust dosages based on the severity of pain and the patient’s response.
Radiation Therapy
For tumors that are localized and causing significant pain, radiation therapy can be a valuable treatment. Radiation can shrink the tumor, providing relief from pain and swelling, and it may also slow the growth of the tumor, helping manage the symptoms of fungating tumors. This treatment is typically used when chemotherapy is not appropriate or when the tumor is not responsive to other treatments.
Palliative Care
Ultimately, palliative care is a critical part of managing fungating breast tumors. Palliative care specialists focus on pain relief, symptom management, and improving quality of life rather than seeking a cure. They help ensure that patients are comfortable, informed, and supported through their treatment journey. Palliative care teams work closely with the patient to address pain, fatigue, nausea, and emotional distress.
3. Infection Control
One of the biggest risks when managing fungating breast tumors is infection. As the wound is exposed, it becomes highly susceptible to bacteria, which can cause complications and delay the healing process. Infection control is an ongoing process that requires vigilance and regular intervention.
Antibacterial Treatments
Doctors may prescribe antibiotics to treat or prevent infection. Topical antibiotic creams (such as silver sulfadiazine) can be applied directly to the wound to fight bacteria. Oral antibiotics may also be prescribed if the infection spreads beyond the wound or if there are signs of systemic infection.
Regular Wound Debridement
In some cases, wound debridement (removal of dead tissue) is necessary to promote healing and prevent infection. This procedure, typically performed by a healthcare professional, helps clear the wound of necrotic tissue, allowing healthy tissue to grow and reducing the likelihood of infection. Regular debridement can also help improve odor control and drainage.
4. Psychosocial Support and Counseling
Dealing with a fungating breast tumor can take a heavy toll on a patient’s mental health. Psychosocial support is essential for patients navigating the physical and emotional challenges of living with an advanced cancer diagnosis.
Emotional Support
Patients with fungating tumors may experience feelings of isolation, embarrassment, and grief due to the visible nature of the tumor and the pain it causes. Speaking with a psychologist or oncology counselor can help patients process their emotions and provide them with strategies to cope with stress and anxiety.
Support Groups
Support groups can be an invaluable resource, helping patients connect with others who are going through similar experiences. Being part of a group where they can share their struggles and victories, ask questions, and gain emotional support can help reduce feelings of isolation.
5. Nutritional Support
Managing nutrition is also important for patients with fungating tumors. Loss of appetite, nausea, and difficulty swallowing are common in patients with advanced breast cancer, but maintaining good nutrition can help improve strength and well-being. Nutritional specialists can help guide patients in choosing foods that are easy to digest and rich in the nutrients they need to stay strong during treatment.
Part 4: Prognosis and Quality of Life
A diagnosis of fungating breast cancer signals an advanced stage of disease, but it’s important to understand that even at this stage, patients can manage symptoms and improve their quality of life. Prognosis can vary widely based on several factors, including the stage of cancer, response to treatment, and overall health of the patient. This section will cover what to expect regarding prognosis, how fungating tumors impact day-to-day life, and how patients can maintain their quality of life throughout treatment.
1. Prognosis for Fungating Tumors
A fungating tumor is generally an indicator of advanced-stage breast cancer. By the time a tumor reaches this stage, it often means that the cancer has spread locally or metastasized to other organs. The prognosis for patients with fungating breast cancer varies widely based on individual circumstances, but here’s what we know:
Tumor Size and Spread
- The size of the fungating tumor and the extent to which it has spread to other areas of the body significantly affect prognosis. In many cases, larger tumors that have spread to distant organs will have a poorer prognosis compared to smaller, more localized tumors.
- For patients with metastatic breast cancer, the 5-year survival rate can be lower, especially if the cancer has spread to vital organs like the liver, lungs, or bones. However, survival rates can vary depending on the site of metastasis and the response to treatments.
Impact of Treatment Options
While fungating tumors are generally associated with advanced cancer, patients can still find effective treatments that help manage symptoms and improve quality of life. Treatments like chemotherapy, radiation therapy, and immunotherapy may help shrink the tumor, control pain, and alleviate other symptoms, offering some patients extended survival. Even when a cure isn’t possible, palliative care can provide relief and ensure that patients remain comfortable.
Emotional Impact
The psychological burden of having a fungating tumor can be significant, as patients may feel anxious, isolated, or depressed. While the prognosis may be serious, it’s important to address the emotional impact of cancer and involve psychosocial support to help cope with feelings of distress. Mental health counseling, support groups, and community resources are essential to supporting a patient’s emotional well-being and quality of life.
2. Improving Quality of Life
For patients with fungating tumors, the goal is not only to extend life but to also improve quality of life. The physical symptoms of a fungating tumor, such as pain, swelling, and odor, can make daily life difficult, but they are manageable with the right treatments.
Pain and Symptom Management
Effective pain management and symptom control are central to maintaining quality of life. Palliative care is an excellent resource for patients with fungating tumors, as it focuses on managing symptoms and improving comfort without aiming to cure the disease. The use of pain relief medications, topical analgesics, and radiation therapy can help alleviate discomfort. Furthermore, wound care strategies such as moisture management, odor control, and infection prevention all contribute to better overall comfort.
Managing Emotional Well-Being
Dealing with a fungating tumor can bring emotional distress, but it’s essential to focus on the psychological aspects of care as well. Feeling isolated or self-conscious about the tumor’s appearance is natural, but having supportive care and mental health services in place can make a world of difference. Support groups, in particular, can help patients connect with others who understand their struggles and provide both emotional support and practical advice.
Social and Family Support
Having a strong support system is critical for patients coping with advanced cancer. Family members and friends play a key role in providing emotional support, assisting with day-to-day tasks, and accompanying patients to medical appointments. Home care services, including nurses or caregivers, may also be needed to help manage wound care and assist with mobility.
Patients are encouraged to stay connected with loved ones and reach out for support when needed. Social isolation can make the emotional toll of a fungating tumor even more difficult, so maintaining relationships is crucial for emotional and mental health.
3. Advanced Treatments and Future Options
While fungating tumors are an indication of advanced breast cancer, there is still a wealth of emerging treatmentsand innovations in palliative care that can help patients live longer and more comfortably. Research into immunotherapies, targeted therapies, and new forms of radiation is ongoing, and these treatments offer promise for those struggling with advanced-stage breast cancer.
Immunotherapy and Targeted Therapies
While traditional treatments like chemotherapy and radiation are still critical for symptom management, new immunotherapies and targeted therapies offer potential benefits. Drugs that help the immune system recognize and fight cancer cells, such as pembrolizumab (Keytruda) and atezolizumab (Tecentriq), are beginning to show promise in improving survival rates for some patients with metastatic breast cancer.
In addition, targeted therapies that focus on specific mutations or pathways involved in cancer progression (such as PARP inhibitors) are beginning to be more widely used, especially for patients with BRCA mutations. These therapies are changing the landscape for advanced cancer patients by offering treatments that are more tailored and effective in managing symptoms and controlling disease progression.
Advancements in Palliative Care
The field of palliative care is evolving as well, with new techniques and approaches designed to manage symptoms more effectively and improve the patient’s overall quality of life. For example, advanced wound care technology allows for more efficient healing of fungating wounds, reducing pain and infection risk. Telemedicine is also improving access to palliative care specialists and providing more personalized, home-based care options for patients.
Part 5: FAQs About Fungating Breast Tumors
Fungating breast tumors are a relatively rare yet distressing aspect of advanced breast cancer, and many patients have questions about how to manage them and what to expect. In this section, we’ll answer some of the most commonly asked questions, providing clarity on treatment options, symptom management, and emotional support.
1. What causes a breast tumor to become fungating?
Fungating tumors occur when breast cancer cells grow uncontrollably and outgrow their blood supply. As the tumor expands, it often causes necrosis (tissue death) in the center of the tumor because the blood vessels can no longer nourish the area. When the tissue dies, the tumor often ulcerates, creating an open wound on the surface of the skin. This is what we call a fungating tumor.
Fungating tumors are usually a sign of advanced breast cancer that has spread to surrounding tissues and, in some cases, to the skin. They are most common in patients with Stage 3 or Stage 4 breast cancer, where the tumor has grown large and aggressive.
2. Can fungating breast tumors be treated or cured?
Fungating breast tumors indicate an advanced stage of breast cancer, which means a cure is generally not possible. However, symptoms can be managed, and quality of life can be improved through treatment options like chemotherapy, radiation therapy, wound care, and pain management. In some cases, these treatments can help shrink the tumor, reduce pain, and control infection.
While a fungating tumor may not be curable, palliative care focuses on improving comfort and maintaining dignity. Patients should speak with their oncologist about the best options for symptom relief and maintaining overall health.
3. How can I manage pain and odor from a fungating tumor?
Managing pain and odor from a fungating tumor can be difficult, but there are several strategies that can help:
Odor Control: The use of odor-absorbing dressings (such as charcoal dressings) and antiseptic treatments can help reduce odor. Regular wound cleaning and dressing changes are key to managing the unpleasant smells associated with fungating tumors. Additionally, odor-neutralizing sprays and wound care products can further control odors.
Pain Management: Use of topical analgesics (such as lidocaine) and oral pain medications (such as NSAIDs or opioids) can help control pain. Radiation therapy may also be used to shrink the tumor and alleviate pain. Palliative care teams specialize in managing pain and can tailor treatments to individual needs.
4. What are the best ways to care for a fungating breast cancer wound?
Caring for a fungating breast cancer wound requires gentle, consistent care to prevent infection, manage odor, and promote healing. Here’s how to do it:
- Clean the wound regularly with mild antiseptic solutions, such as saline or iodine-based cleansers, to avoid irritating the skin.
- Use specialized wound dressings that are designed to absorb exudate, control odor, and maintain a moist environment to promote healing.
- Change dressings frequently (usually once a day or as recommended by your healthcare provider) to reduce the risk of infection and ensure proper healing.
- Keep the area as dry and clean as possible to prevent bacterial growth and further irritation.
Always work closely with healthcare providers or wound care specialists to develop a personalized care plan that suits your specific needs.
5. How can I cope with the emotional impact of a fungating tumor?
The emotional toll of living with a fungating breast tumor can be significant. It’s common to feel a range of emotions, from self-consciousness about appearance to anxiety about cancer progression. Here are a few ways to cope:
- Seek emotional support from a counselor, psychologist, or support group. Sharing your feelings with others who understand your experience can be incredibly healing.
- Stay connected with family and friends. While it can be difficult, talking to loved ones and keeping a support system in place can help alleviate feelings of isolation.
- Join a support group for people dealing with breast cancer or fungating tumors. These groups provide a space where patients can share their experiences and provide advice or encouragement.
- Mindfulness techniques, relaxation exercises, and therapy can help manage stress and emotional pain.
Remember, it’s okay to ask for help. Mental health professionals and oncology counselors are available to provide support during this challenging time.
6. Is a fungating tumor a sign of cancer spreading?
Yes, a fungating tumor is often a sign that the cancer has reached an advanced stage and has spread to the skin and possibly other tissues. It typically indicates that the tumor has grown large and aggressive, making it more likely to cause local invasion and ulceration.
However, the appearance of a fungating tumor doesn’t necessarily mean that the cancer has spread to distant organs (metastasized). It’s important for doctors to assess whether the cancer is localized or whether it has spread to other organs such as the liver, lungs, or bones. Imaging tests and biopsy procedures will help doctors understand the full extent of cancer spread.
7. What should I expect during treatment for a fungating tumor?
During treatment for a fungating tumor, patients can expect a combination of chemotherapy, radiation therapy, and palliative care to help manage symptoms and improve quality of life. The goal of treatment is to:
- Shrink the tumor and reduce pain through chemotherapy and radiation therapy.
- Manage symptoms, including pain, odor, and infection, with wound care and antibiotics.
- Provide emotional support through counseling and support groups to help patients cope with the emotional and psychological challenges of living with advanced cancer.
Treatment will depend on the stage of the tumor, its location, and the patient’s overall health. Working closely with a healthcare team will help ensure that the treatment plan is personalized and effective in addressing symptoms and improving quality of life.
Part 6: Final Thoughts
Fungating breast tumors, while challenging and distressing, are not the end of the road. Though they are often associated with advanced stages of breast cancer, it’s crucial to remember that there are still treatment options and support that can make a significant difference in quality of life. From pain management to wound care and psychosocial support, patients can manage symptoms, find comfort, and continue to lead fulfilling lives.
While prognosis can vary depending on factors like the extent of cancer spread, the size of the tumor, and the patient’s overall health, the emphasis on palliative care and symptom management ensures that each patient’s experience is as comfortable and supported as possible. It’s important to work closely with your healthcare team to make sure your care plan is personalized to your needs, and that every symptom, whether physical or emotional, is addressed.
Understanding the challenges of fungating breast tumors can also help patients and their loved ones make informed decisions about care and treatment choices. Advances in immunotherapy, targeted therapies, and wound care techniques have greatly improved the management of these tumors, giving patients hope and practical solutions for managing this difficult condition.
Finally, it’s vital to never underestimate the power of community and support. Whether through family, support groups, or counseling, having the emotional support you need is just as important as the physical treatments in managing this condition. Taking steps to reach out for help and embracing the support available to you can provide significant emotional relief during a time when it’s needed the most.
Remember, no one has to face a fungating tumor alone — with the right care, support, and resources, you can navigate this journey with strength and dignity.












