Frequent Urination in Bladder Cancer
Frequent Urination in Bladder Cancer: Understanding the Symptom and Its Implications
- Why Frequent Urination Happens in Bladder Cancer
- What’s Happening Inside the Body: Tumor Impact on Urinary Function
- How Common Is This Symptom Among Bladder Cancer Patients?
- What Clinical Patterns Are Seen at Different Cancer Stages?
- What Causes This Symptom in Bladder Cancer Patients?
- Red Flags: When Frequent Urination Indicates a Serious Issue
- How Doctors Identify the Cause of Urinary Changes
- Managing and Treating Frequent Urination in Bladder Cancer
- Can This Symptom Be Prevented or Reduced?
- Does Frequent Urination Go Away After Treatment?
- What Specialists Say About Urinary Symptoms in Bladder Cancer
- 15+ Frequently Asked Questions (FAQ)
Why Frequent Urination Happens in Bladder Cancer
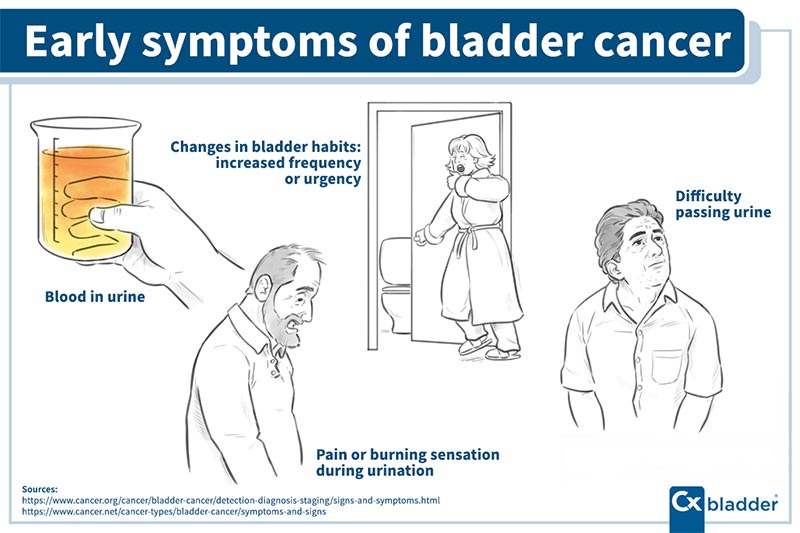
One of the earliest and most common symptoms cancer patients report with bladder involvement is frequent urination. It may begin subtly—an extra trip to the bathroom during the day or waking once at night—but gradually intensifies until it disrupts daily life.
In bladder cancer, tumors grow within or near the lining of the bladder wall. As these abnormal cells multiply, they irritate the bladder’s internal surface and reduce its functional capacity, creating a persistent feeling of urgency. Even if the bladder is only partially full, patients may feel an immediate need to void.
Frequent urination can also reflect the body’s inflammatory response to the tumor or indicate that the cancer has begun to obstruct or distort bladder anatomy. For many individuals, this symptom is mistaken for a urinary tract infection (UTI) or aging-related bladder changes, delaying proper diagnosis.
What’s Happening Inside the Body: Tumor Impact on Urinary Function
The mechanism behind frequent urination in bladder cancer is directly linked to how tumors affect bladder structure and neural signaling. The bladder normally stretches to accommodate urine and contracts only when full. However, when a tumor invades the bladder wall or grows into the lumen, it disrupts this balance.
Cancer cells trigger chronic inflammation, leading to swelling, nerve irritation, and hyperactivity of the detrusor muscle (the bladder’s main muscle). This hyperactivity causes the bladder to contract more often, even when it contains small amounts of urine.
In more advanced cases, the tumor may physically block part of the bladder neck or urethra, preventing complete emptying. As a result, patients void small amounts repeatedly. If the cancer infiltrates nearby nerves (a process called perineural invasion), the communication between brain and bladder becomes even more erratic, increasing urgency.
This explains why frequent urination may occur even when fluid intake hasn’t changed—and why traditional infection treatments fail to relieve it.
How Common Is This Symptom Among Bladder Cancer Patients?
Frequent urination is highly prevalent in patients with bladder cancer, especially in non-muscle-invasive forms, where tumors grow on or just beneath the inner bladder lining. Studies estimate that up to 80% of early-stage bladder cancer patients experience urinary frequency, urgency, or discomfort at some point during their illness.
In more advanced or muscle-invasive bladder cancers, the symptom may shift from simple frequency to more complex patterns, including incomplete emptying or overflow incontinence. Post-surgical patients who have undergone bladder removal (cystectomy) and urinary diversion may experience entirely different urinary patterns, but frequent urination often returns in the early phases of treatment.
Veterinary data shows similar findings in animal oncology: both Bladder Cancer in Dogs and Bladder Cancer in Cats often present with urinary frequency and discomfort, highlighting how this symptom reflects irritation and obstruction across species.
Age, tumor location (especially near the bladder neck or trigone), and prior bladder damage (from smoking or chronic infections) also influence how early and how severely frequent urination presents.
What Clinical Patterns Are Seen at Different Cancer Stages?
The frequency and severity of urination symptoms often correlate with the stage and spread of the tumor. In early-stage (Ta, T1) bladder cancer, which is confined to the mucosa or lamina propria, urination becomes more frequent due to localized inflammation and early nerve sensitization.
As tumors progress into muscle-invasive (T2–T4) stages, symptoms may intensify. At this point, frequent urination is often joined by pelvic discomfort, hematuria (blood in the urine), or flank pain if the ureters are involved.
Patients with carcinoma in situ (CIS)—a flat, aggressive form of bladder cancer—may experience extremely frequent urination, even in the absence of visible tumors. CIS is known to cause profound bladder lining inflammation, resulting in what some patients describe as “constant pressure” or “never feeling empty.”
In metastatic cases, bladder function may be further affected by secondary tumor sites, nerve damage, or complications from therapies like radiation. In such stages, managing urination becomes a multidisciplinary challenge involving urology, oncology, and palliative care teams.
What Causes This Symptom in Bladder Cancer Patients?
Frequent urination in bladder cancer arises from a complex mix of tumor-related, treatment-induced, and metabolic factors. Understanding these causes can help distinguish between benign urinary issues and those warranting urgent oncologic care.
Tumor Irritation and Inflammation
The most direct cause is irritation of the bladder wall by cancer cells. Even small tumors can trigger a powerful local immune response, releasing cytokines and inflammatory mediators that sensitize the bladder’s nerves. This leads to overactivity of the detrusor muscle and premature urges to urinate.
Reduced Bladder Capacity
Tumors growing near the bladder neck or trigone (where the ureters and urethra meet) physically reduce the volume the bladder can hold. In these cases, the bladder reaches its threshold sooner, even with minimal fluid, prompting more frequent urination.
Treatment Side Effects
Intravesical therapies (such as BCG immunotherapy) used to treat non-muscle-invasive cancer often cause inflammation, mimicking infection. Chemotherapy agents that are excreted via the bladder may also inflame the lining, creating temporary urgency.
Radiation Cystitis
In patients receiving pelvic radiation for invasive bladder cancer, damage to the urothelium and microvasculature can lead to chronic radiation cystitis—a condition marked by persistent urgency, frequency, and pain during urination.
Secondary Conditions
Not all urinary frequency is tumor-related. Co-existing bladder stones, infections, diabetes, or prostate enlargement can coexist in cancer patients, making proper diagnosis essential.
Red Flags: When Frequent Urination Indicates a Serious Issue
While urinary frequency is often manageable, certain patterns suggest progression, complications, or treatment toxicity—and should prompt immediate evaluation by a medical professional.
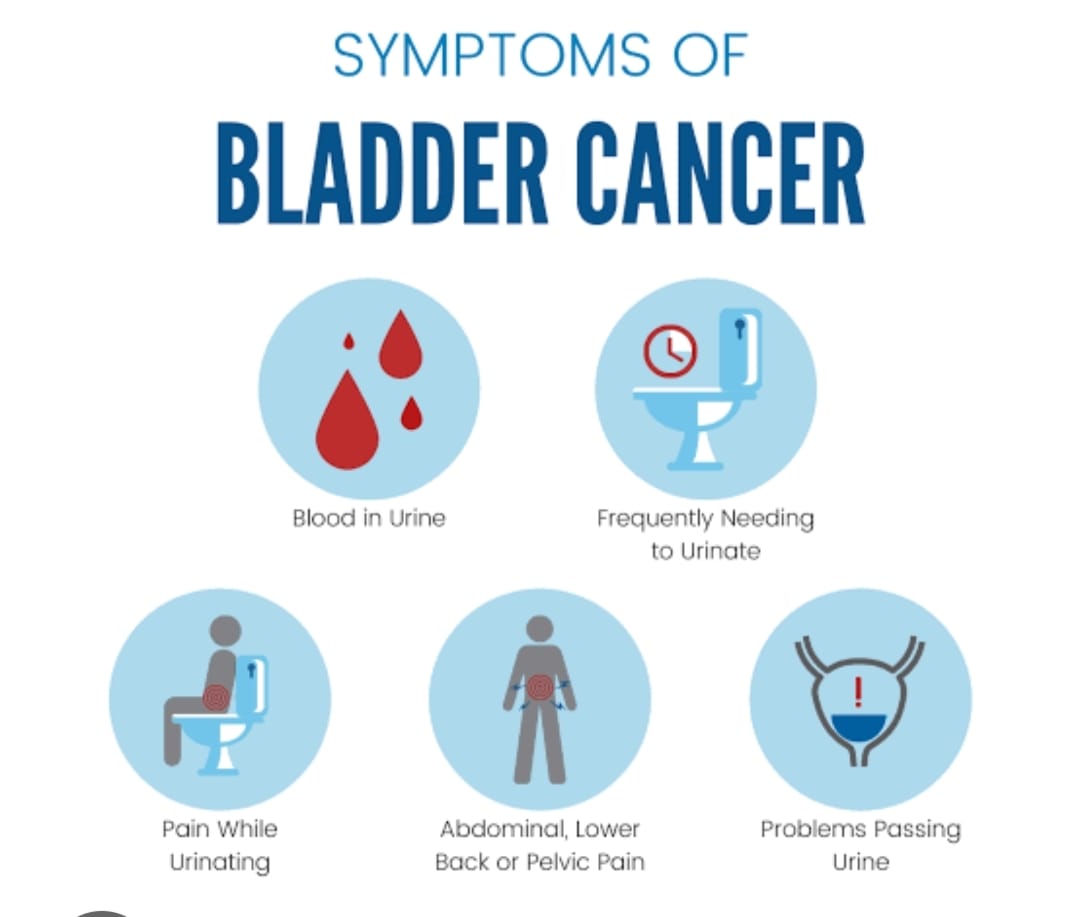
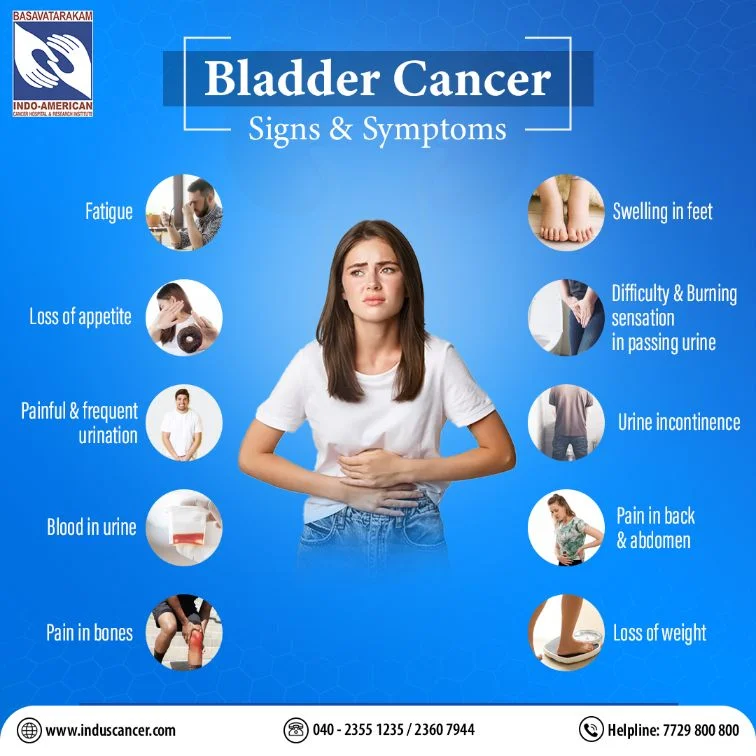
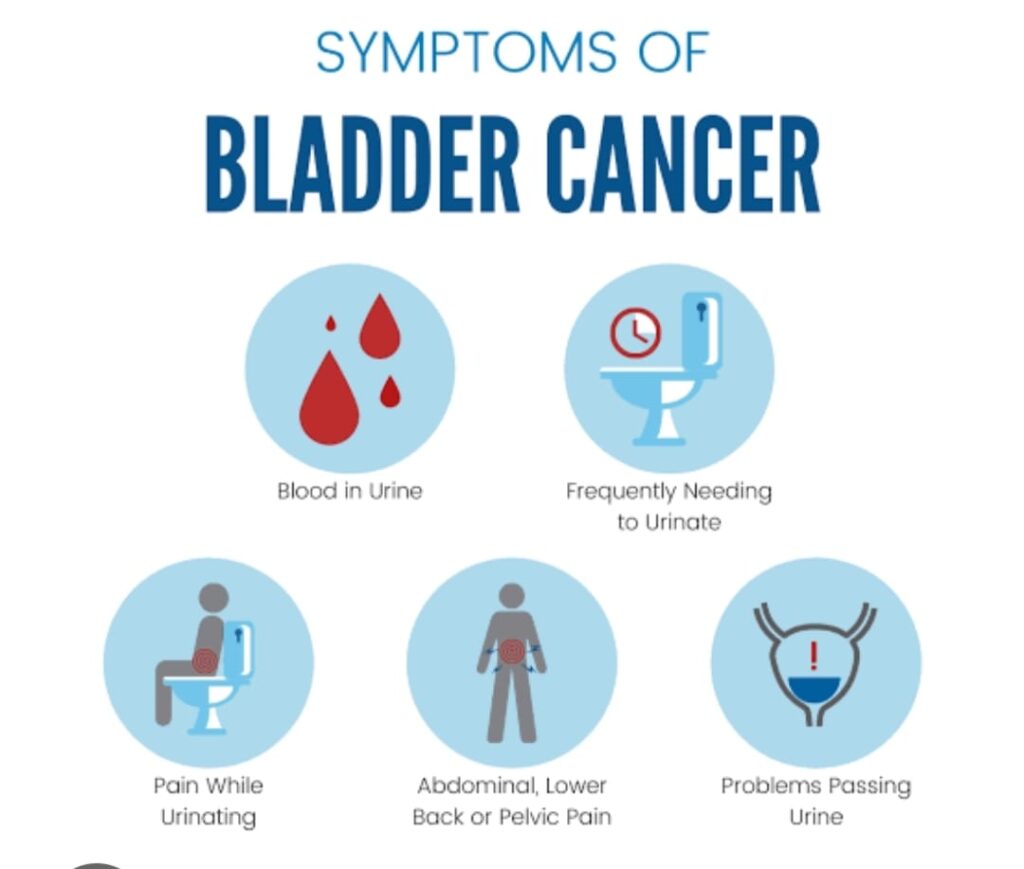
- Increased frequency accompanied by blood in urine (gross or microscopic hematuria)
- Persistent urgency that worsens despite antibiotics
- Pain or burning during urination, especially after bladder treatments
- Sudden incontinence or inability to control urination
- Fever or chills, which may signal urinary tract infection or urosepsis
- Pelvic or lower back pain, particularly in advanced stages
- Nocturia (waking multiple times per night to urinate) combined with fatigue and appetite loss
These signs may point to deeper invasion of the bladder wall, obstruction of the ureters, or metastasis to nearby structures. In some cases, they also suggest immune-mediated inflammation from therapies like BCG.
In patients with a known cancer diagnosis, any rapid shift in urination patterns should be reported promptly—even if they seem minor. These changes may signal tumor recurrence or a complication needing intervention.
How Doctors Identify the Cause of Urinary Changes
Evaluating frequent urination in the context of bladder cancer involves a structured diagnostic approach that differentiates between cancer progression, treatment effects, and unrelated urinary tract conditions.
History and Symptom Mapping
Physicians begin with a detailed history of urinary frequency: timing, urgency, nocturia, pain, and volume. They also assess recent treatments and medications to rule out therapy-related side effects.
Urinalysis and Culture
Initial lab tests include urinalysis to detect blood, leukocytes, or nitrates (markers of infection). A urine culture may be ordered to exclude bacterial causes, which are common in immunocompromised patients.
Urine Cytology and Biomarkers
In high-risk patients, urine samples may be tested for malignant cells or tumor markers like NMP22 or UroVysion. These tests help detect cancer recurrence in patients under surveillance.
Imaging
Ultrasound or CT urogram can reveal structural abnormalities, tumor masses, or post-void residual urine. MRI may be used if nerve involvement or soft tissue infiltration is suspected.
Cystoscopy
This is the gold standard for diagnosing bladder cancer–related symptoms. A small camera is inserted into the bladder to directly visualize tumors, inflammation, or other structural changes.
If a patient previously treated for bladder cancer develops new frequency, cystoscopy helps distinguish between inflammation, recurrence, or treatment effect.
Managing and Treating Frequent Urination in Bladder Cancer
Relieving frequent urination in bladder cancer requires both symptom control and treatment of the underlying cause. Management strategies differ depending on whether the symptom is tumor-driven, treatment-induced, or functional.
Tumor-Directed Therapy
For early-stage cancer, transurethral resection (TURBT) of the tumor may significantly reduce frequency. In more advanced cases, neoadjuvant chemotherapy or immunotherapy may shrink tumors before further intervention.
Anti-Inflammatory Treatment
Intravesical therapies such as BCG may cause inflammation; in these cases, anti-inflammatory medications (NSAIDs, anticholinergics) are used to reduce symptoms. Topical bladder agents like hyaluronic acid instillation are also used off-label for chronic bladder pain and frequency.
Antimuscarinics and Beta-3 Agonists
Medications like oxybutynin or mirabegron help control overactive bladder symptoms by relaxing the detrusor muscle. They are commonly prescribed during and after bladder treatment if no obstruction is present.
Pelvic Floor Physical Therapy
In select patients, especially those with functional urinary issues post-treatment, guided therapy helps restore bladder control and reduce urgency episodes.
Palliative Support
In metastatic cases or when curative treatment isn’t feasible, palliative care focuses on comfort. This may include medications to manage bladder spasms, lifestyle adaptations, and devices to help with incontinence.
The key is personalized management—tailored to tumor burden, treatment history, and quality-of-life goals.
Can This Symptom Be Prevented or Reduced?
Although frequent urination is a common part of the bladder cancer experience, early intervention and preventive strategies can reduce its severity or even delay its onset. Prevention focuses on managing inflammation, preserving bladder health, and minimizing treatment-related side effects.
Surveillance and Early Detection
For patients at high risk (smokers, those with chronic bladder infections), regular screening and urinalysis can help detect bladder lesions early—before they disrupt normal bladder function.
Lifestyle Measures
Avoiding bladder irritants like caffeine, alcohol, acidic foods, and spicy meals may help reduce urgency and frequency. Staying hydrated with water—rather than carbonated or sugary drinks—also helps flush irritants without overstimulating the bladder.
Anti-inflammatory Support During Therapy
In patients undergoing BCG or chemotherapy, physicians may preemptively prescribe anticholinergic medications to manage expected urinary side effects. Maintaining bladder mucosa integrity with hydration and protective agents (like sodium hyaluronate) is under clinical exploration.
Pelvic Muscle Strengthening
Pelvic floor exercises (Kegels) under the supervision of a physical therapist can support bladder control, especially in post-treatment or elderly patients.
While frequent urination may not be completely avoidable, taking a proactive approach can significantly reduce discomfort and support quality of life.
Does Frequent Urination Go Away After Treatment?
The outcome of frequent urination in bladder cancer varies by stage, tumor location, and treatment type. In many cases, the symptom does improve—but not always fully.
After Tumor Removal (TURBT or Cystectomy)
If frequency was caused by direct tumor irritation, removal often results in rapid relief. Patients with superficial tumors may see a return to near-normal bladder habits within weeks.
Following Chemotherapy or BCG
Urinary frequency due to inflammation typically resolves within a few weeks of completing therapy. However, some patients experience lingering urgency or mild discomfort for months, especially after multiple treatment cycles.
After Radiation Therapy
Radiation cystitis can lead to chronic bladder damage, including fibrosis or reduced capacity. In these cases, frequency may persist long-term and require specialized urologic management.
With Urinary Diversion
Patients who undergo bladder removal and urinary diversion (ileal conduit, neobladder, or urostomy) will have different voiding patterns. Neobladder patients, for example, may urinate more frequently at first, but this often improves with time and training.
While the symptom may never disappear completely in some cases, it often becomes more manageable with time, proper therapy, and support.
What Specialists Say About Urinary Symptoms in Bladder Cancer
Urologic oncologists and bladder cancer specialists emphasize that frequent urination is more than just a nuisance—it’s a valuable clinical indicator.
Dr. Karen Lin, uro-oncology specialist, notes:
“New-onset urinary urgency in a patient over 50 should always raise suspicion. Bladder cancer symptoms often mimic benign conditions, which is why they get overlooked.”
Dr. Samuel Yeh, radiation oncologist, adds:
“In patients receiving pelvic radiation, it’s crucial to differentiate between expected side effects and signs of recurrence. Frequent urination post-radiation should always be investigated if it persists beyond three months.”
Veterinary oncologists echo this in animal care: both Bladder Cancer in Dogs and Bladder Cancer in Cats often present with frequency and straining, highlighting the symptom’s diagnostic value across species.
Experts recommend early cystoscopy, especially when antibiotics don’t relieve urinary symptoms. They also advocate for integrated care between urology, oncology, and palliative services to manage the symptom holistically.
15+ Frequently Asked Questions (FAQ)
1. Is frequent urination always a sign of bladder cancer?
No, but when it occurs alongside other symptoms like blood in urine or urgency, especially in older adults or smokers, it should be evaluated thoroughly.
2. How is frequent urination in bladder cancer different from an overactive bladder?
It’s often more persistent, can occur even with low urine volume, and doesn’t respond well to standard bladder medications without treating the underlying tumor.
3. Will frequent urination stop after tumor removal?
Often, yes—especially in non-muscle-invasive cases. However, some patients experience residual urgency due to inflammation or bladder wall changes.
4. Can bladder cancer cause incontinence too?
Yes, particularly in advanced cases or after certain surgeries. The bladder may lose capacity or control, leading to leakage or overflow.
5. Does BCG treatment cause urination problems?
Yes, it can temporarily increase urgency, frequency, and discomfort. These symptoms usually resolve after treatment ends.
6. What should I avoid eating or drinking to reduce frequency?
Limit caffeine, alcohol, citrus juices, spicy foods, and artificial sweeteners. Drink plain water and avoid bladder irritants.
7. Can medications help control urinary frequency in cancer?
Yes. Antimuscarinics or beta-3 agonists like mirabegron may help. Always consult a physician, as they must rule out obstruction first.
8. How often should a bladder cancer patient have urinalysis or imaging?
Typically every 3–6 months depending on cancer stage and treatment. Frequent urination between checkups should prompt earlier evaluation.
9. Is frequent urination dangerous on its own?
Not usually, but it can signal serious complications if paired with pain, blood, or systemic symptoms like fever.
10. Do women experience this symptom differently?
Yes. Women may delay reporting symptoms, mistaking them for UTIs. This often leads to delayed diagnosis.
11. What if frequent urination persists despite treatment?
You may need cystoscopy or imaging to rule out recurrence, inflammation, or bladder dysfunction. A uro-oncologist can advise further.
12. Can pelvic floor therapy help?
Yes, especially post-treatment or in cases of functional incontinence. A therapist can teach exercises to improve control.
13. Is frequent urination a sign of metastasis?
Sometimes—especially if paired with pelvic pain or neurological symptoms. Always get checked if new symptoms appear.
14. Will I need lifelong bladder medications?
Not always. Many patients improve after treatment, but some may need long-term symptom control depending on damage or scarring.
15. Should I track my urination habits?
Yes. Keeping a voiding diary helps doctors identify patterns, triggers, and assess treatment response.