First Symptoms of Ovarian Cancer: A Comprehensive Guide
- Understanding Ovarian Cancer
- The Challenge of Early Detection
- Common Early Symptoms
- When to Seek Medical Advice
- Diagnostic Tools and Initial Tests
- The Role of Family History and Genetics
- Overlapping Symptoms with Gastrointestinal Disorders
- Hormonal Influence and Menstrual Irregularities
- Misdiagnosis and Delays in Care
- Ovarian Cancer in Younger Women
- The Importance of Multidisciplinary Care
- Hormone Receptors and Tumor Biology
- Monitoring Symptoms Over Time
- Impact of Lifestyle and Reproductive History
- Public Awareness and Screening Limitations
- Conclusion: Listening to the Subtle Signs
- FAQ
Understanding Ovarian Cancer
Ovarian cancer originates in the ovaries, the reproductive glands found in women that produce eggs and hormones like estrogen and progesterone. There are several types of ovarian cancer, with epithelial ovarian cancer being the most common. This type begins in the thin layer of tissue that covers the ovaries. Other types include germ cell tumors, which start in the egg-producing cells, and stromal tumors, which develop in the hormone-producing tissue.
The exact cause of ovarian cancer is not fully understood, but certain factors may increase the risk. These include age (most ovarian cancers develop after menopause), family history of ovarian or breast cancer, genetic mutations such as BRCA1 and BRCA2, and certain reproductive history factors. Understanding these risk factors is essential for early detection and prevention strategies.
The Challenge of Early Detection
One of the significant challenges with ovarian cancer is that it often goes undetected until it has spread within the pelvis and abdomen. This is primarily because early-stage ovarian cancer rarely causes noticeable symptoms. When symptoms do occur, they are often nonspecific and can be mistaken for more common benign conditions, such as digestive or bladder disorders.
As the disease progresses, symptoms become more apparent and severe. However, by this time, the cancer may have advanced to a stage where it is more difficult to treat. Therefore, recognizing the early signs, even if they are subtle, is crucial for timely diagnosis and treatment.
Common Early Symptoms
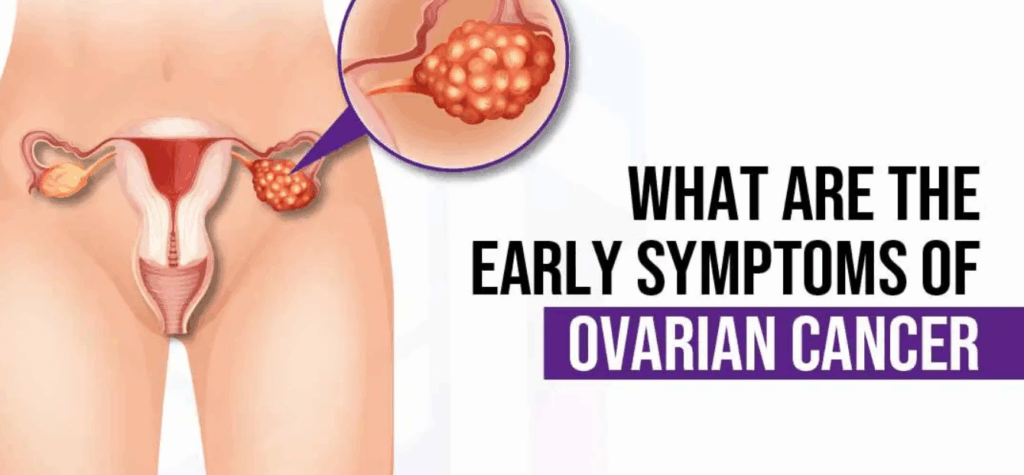
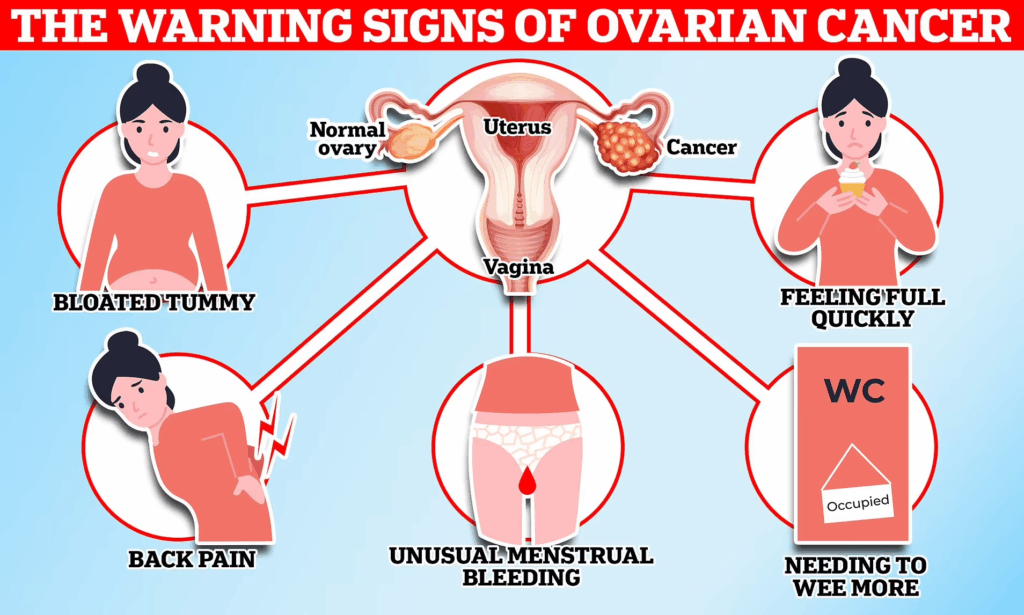
The early symptoms of ovarian cancer are often vague and can be easily overlooked. However, being attentive to these signs can lead to earlier detection. Common early symptoms include:
- Abdominal bloating or swelling: Persistent bloating that doesn’t go away can be a warning sign.
- Quickly feeling full when eating: A sudden loss of appetite or feeling full after eating a small amount.
- Weight loss: Unexplained weight loss without changes in diet or exercise.
- Discomfort in the pelvic area: Persistent pain or pressure in the pelvis.
- Fatigue: Unusual tiredness that doesn’t improve with rest.
- Back pain: Lower back pain that persists over time.
- Changes in bowel habits: Such as constipation or diarrhea.
- Frequent need to urinate: An increased urgency or frequency of urination.
It’s important to note that these symptoms can be caused by conditions other than ovarian cancer. However, if you experience these symptoms persistently, it’s essential to consult a healthcare professional for further evaluation.
When to Seek Medical Advice
Determining when to seek medical advice can be challenging, especially when symptoms are subtle. However, if you experience any of the aforementioned symptoms more than 12 times a month, it’s advisable to consult your doctor. Early evaluation can lead to earlier diagnosis, which is associated with better treatment outcomes.
Your doctor may perform a pelvic examination to check for any abnormalities. They might also recommend imaging tests, such as an ultrasound or CT scan, and blood tests like CA-125, which measures a protein that is often elevated in women with ovarian cancer. These diagnostic tools can help determine the cause of your symptoms and guide further management.
Diagnostic Tools and Initial Tests
When ovarian cancer is suspected, early diagnostic steps focus on imaging, blood markers, and physical examination. The pelvic exam is often the first step, allowing the physician to palpate any abnormalities in the ovaries or surrounding structures. However, small tumors in the early stages are rarely detectable this way, which is why imaging is essential.
Transvaginal ultrasound is the most common first-line tool. It provides detailed images of the ovaries and can identify cystic or solid masses. If suspicious features are noted, the next step may include a CT scan or MRI for more comprehensive assessment. Blood tests like CA-125 may be ordered to measure tumor markers, although this test is not specific to ovarian cancer and can be elevated in benign conditions as well.
Interestingly, these screening uncertainties mirror debates in other emerging health technologies. For instance, concerns about overstimulation of cells through unproven methods — such as those examined in the article Can Microcurrent Cause Cancer — show how difficult it is to balance innovation and biological safety in early-stage detection and intervention.
The Role of Family History and Genetics
Genetic predisposition plays a major role in the development of ovarian cancer. Mutations in BRCA1 and BRCA2 significantly increase the lifetime risk not only of breast cancer but also of ovarian malignancy. Women with Lynch syndrome, a hereditary condition linked to several cancers, also face elevated risk.
Understanding family history is critical. Patients with a strong family history of ovarian, breast, or colorectal cancer should consider genetic counseling. Testing for BRCA mutations can guide decisions about screening, preventive surgery (such as prophylactic oophorectomy), or chemoprevention.
Importantly, guidelines recommend earlier and more aggressive monitoring for women with known genetic risks. This includes baseline imaging and regular CA-125 testing, even if no symptoms are present. Tailored risk-reduction strategies can significantly impact long-term outcomes for genetically predisposed individuals.
Overlapping Symptoms with Gastrointestinal Disorders
One reason ovarian cancer is often diagnosed late is that its early symptoms overlap heavily with common gastrointestinal (GI) complaints. Bloating, constipation, indigestion, and early satiety are all signs that could be easily attributed to dietary issues, irritable bowel syndrome, or food intolerance.
This symptom confusion delays proper evaluation, especially in younger women or those without known risk factors. Unfortunately, by the time GI-focused treatment fails and further testing is initiated, the cancer may have progressed. Physicians must be aware of this overlap and maintain a low threshold for initiating pelvic imaging in women with persistent, unexplained GI complaints.
As seen in other cancers — overlapping symptoms can significantly affect how quickly and accurately a diagnosis is reached. Pattern recognition, persistence, and physician intuition are essential in both human and veterinary medicine.
Hormonal Influence and Menstrual Irregularities
Hormonal fluctuations play a role in both the development and early presentation of ovarian cancer. While most ovarian cancers are diagnosed after menopause, some women may experience abnormal menstrual cycles or hormonal imbalances in the perimenopausal period that precede diagnosis.
Symptoms such as irregular bleeding, heavier than usual periods, or skipped cycles should be taken seriously — especially when combined with pelvic discomfort or bloating. These signs are sometimes written off as hormonal “shifts” due to aging, yet they may reflect early disruption in ovarian function caused by tumor growth.
Women with hormone-sensitive cancers may also present with endocrine changes, including breast tenderness, mood swings, or hot flashes. While these signs are subtle, in the context of other early symptoms, they can form part of a clearer clinical picture. Recording cycle patterns and hormonal symptoms can aid in earlier intervention.

Misdiagnosis and Delays in Care
Ovarian cancer is often misdiagnosed in its early stages due to the subtle and nonspecific nature of its symptoms. Many women report being initially treated for gastrointestinal issues, bladder infections, or perimenopausal symptoms. In some cases, healthcare providers may attribute complaints to psychological causes, especially in younger patients, leading to months or even years of delayed diagnosis.
These diagnostic delays can significantly affect prognosis, as ovarian cancer responds best to treatment when caught early. The average time from first symptom to diagnosis is estimated to be more than 6 months for many patients, particularly those without clear risk markers. This delay is exacerbated in healthcare systems with limited access to specialists or imaging services.
Similar diagnostic challenges are seen in aggressive forms of breast cancer such as HER2-positive subtypes, where patients often benefit from early, aggressive treatment like TCHP chemotherapy. In both diseases, fast and accurate recognition of symptom patterns is critical to survival, underscoring the need for heightened awareness across primary care and gynecology.
Ovarian Cancer in Younger Women
While ovarian cancer is more commonly diagnosed after menopause, it is not exclusive to older women. Germ cell tumors and some stromal tumors tend to present at younger ages, sometimes even in teenagers or women in their 20s and 30s. Unfortunately, because ovarian cancer is considered a “disease of aging,” early symptoms in younger women may be dismissed or misinterpreted as stress-related or reproductive disorders.
Common signs in this group include persistent bloating, missed periods, unexplained weight changes, or abdominal pain unrelated to menstruation. In some cases, the discovery of a pelvic mass during a routine gynecological exam or ultrasound for infertility leads to diagnosis.
Healthcare providers must remain vigilant, especially when presented with unusual symptoms that persist despite treatment. Young women with family history or genetic predisposition should be screened earlier, and those presenting with unexplained pelvic symptoms should be evaluated with imaging promptly — regardless of age.
The Importance of Multidisciplinary Care
Management of ovarian cancer, even from the first symptom, often requires coordination between various specialties. Gynecologists, oncologists, radiologists, genetic counselors, and sometimes gastroenterologists must work together to reach an accurate diagnosis and establish a treatment plan. For example, early involvement of a gynecologic oncologist improves surgical outcomes and is linked to higher survival rates.
This multidisciplinary approach also helps identify and support patients with complex presentations, overlapping diagnoses, or comorbid conditions. Psychosocial support, nutritional guidance, and fertility counseling are often necessary during early stages, especially for younger women.
Integrating this collaborative care model early — even before definitive diagnosis — improves patient outcomes and experience. Many comprehensive cancer centers now use nurse navigators to streamline referrals, explain test results, and ensure timely follow-up, which is particularly beneficial in a disease known for diagnostic delay.
Hormone Receptors and Tumor Biology
Understanding the biological characteristics of ovarian tumors is crucial for both diagnosis and treatment. Some ovarian cancers express hormone receptors, such as estrogen or progesterone receptors, which may influence how the cancer grows and responds to therapy. While not all ovarian cancers are hormone-sensitive, those that are may be influenced by the body’s natural or synthetic hormonal environment.
Tumor biology also affects symptom presentation. For example, some slow-growing tumors may produce more subtle, chronic symptoms, while aggressive high-grade serous carcinomas can cause more rapid abdominal swelling and weight changes. Molecular profiling helps classify the tumor and tailor treatment, including decisions about chemotherapy, targeted therapy, or hormone modulation.
This approach is increasingly aligned with personalized oncology models used in other cancers — such as HER2 status guiding the use of TCHP in breast cancer — ensuring patients receive not just fast care, but the right care. The shift toward precision medicine is gradually transforming how even early symptoms are evaluated in oncology.
Monitoring Symptoms Over Time
One of the most important strategies in recognizing ovarian cancer early is tracking symptoms over time. Because the early signs are often intermittent and nonspecific, many patients disregard them until they become persistent. Healthcare providers recommend that women keep a symptom diary — noting frequency, intensity, and duration of issues such as bloating, appetite loss, or pelvic pain.
Symptom tracking becomes especially valuable when combined with patient history and risk profile. A symptom that occurs once or twice might be inconsequential, but if it occurs more than 12 times in a month, further evaluation is warranted. Structured documentation can support clinical suspicion and justify imaging or laboratory workups.
This longitudinal observation approach is common in other fields of medicine as well. For instance, subtle neurological symptoms in animals — like dragging limbs or postural changes — are key to early detection of diseases like spinal cancer in dogs, where missed signals delay treatment. Similarly, cumulative symptom tracking in ovarian cancer can be life-saving.
Impact of Lifestyle and Reproductive History
Lifestyle and reproductive history also play a role in modulating ovarian cancer risk and potentially influencing how symptoms present. Women who have had children, used oral contraceptives, or breastfed may have a slightly lower risk of ovarian cancer. These factors affect ovulation frequency and hormonal cycles, which are believed to influence cell turnover in the ovaries.
Conversely, women with early menarche, late menopause, or a history of infertility treatments may face higher risk due to prolonged estrogen exposure and increased ovulatory cycles. These conditions can also cause hormonal symptoms similar to those seen in early ovarian cancer, making diagnostic differentiation more difficult.
Understanding how reproductive patterns affect not only risk but also symptom mimicry is essential. It supports the need for individualized assessment, especially in women with overlapping gynecological or hormonal concerns. Doctors should consider these nuances when interpreting early symptoms and recommending follow-up steps.
Public Awareness and Screening Limitations
Despite being one of the deadliest gynecologic cancers, ovarian cancer receives relatively little public attention compared to breast or cervical cancer. This low awareness contributes to delayed diagnoses and inadequate symptom recognition. Unlike cervical cancer, which can be screened via Pap smears, or breast cancer, which has widespread mammographic guidelines, ovarian cancer lacks an effective, universally accepted screening method.
While CA-125 and transvaginal ultrasound are used in high-risk populations, they are not recommended for routine screening due to low specificity and high false-positive rates. This gap makes symptom education even more critical — the earlier women recognize patterns that don’t resolve with standard care, the earlier intervention can begin.
Awareness campaigns, especially during Ovarian Cancer Awareness Month (September), are essential to elevate knowledge about early signs. Encouraging self-monitoring and regular gynecological evaluations empowers women to advocate for themselves in medical settings, potentially reducing the high percentage of late-stage diagnoses.
Conclusion: Listening to the Subtle Signs
Ovarian cancer rarely shouts — it whispers. The earliest symptoms are quiet, vague, and easy to dismiss. Yet, listening closely to your body and tracking persistent changes is often the first step toward early diagnosis. Bloating, appetite changes, pelvic pain, or unusual fatigue are not necessarily alarming on their own — but when they linger or cluster together, they demand attention.
The key to combating ovarian cancer is vigilance — both from patients and providers. While science works toward better screening tools, education remains the most powerful tool in our arsenal. Recognizing the subtle signs and acting on them promptly may save months of diagnostic delay — and ultimately, lives.
Whether you’re managing known risks, experiencing unexplained symptoms, or simply want to stay informed, trust your instincts and seek professional evaluation when something feels wrong. Early detection begins with awareness — and awareness begins with you.
FAQ
What are the earliest signs of ovarian cancer most women ignore?
The earliest signs are often vague and include persistent bloating, pelvic or abdominal pain, early satiety (feeling full quickly), and increased urinary frequency. Because these symptoms are common in many benign conditions, they’re frequently dismissed or misattributed until they become more severe.
How often should I experience symptoms before I see a doctor?
If you notice symptoms such as bloating, pelvic discomfort, or appetite changes more than 12 times in a month, it’s advisable to consult your healthcare provider. Early medical evaluation is critical for ruling out serious conditions, including ovarian cancer.
Can ovarian cancer cause digestive symptoms?
Yes, many early signs mimic gastrointestinal issues, including indigestion, constipation, and a feeling of fullness. This overlap often leads to misdiagnosis, especially when physicians focus solely on GI-related causes without considering gynecologic evaluation.
Is weight loss an early symptom of ovarian cancer?
Unexplained weight loss, especially when accompanied by decreased appetite and bloating, can be an early sign. While it’s not exclusive to ovarian cancer, it should raise concern if it occurs without dietary changes or increased activity.
Does back pain relate to ovarian cancer?
Yes, lower back pain can be an early symptom, particularly if it persists and doesn’t respond to conventional treatment. This pain may result from pressure on nearby tissues or early-stage tumor growth in the pelvic area.
Can ovarian cancer be detected through a Pap smear?
No. Pap smears are used to screen for cervical cancer, not ovarian cancer. Ovarian cancer is located higher in the reproductive tract, making it undetectable through standard Pap tests.
What tests are used to diagnose ovarian cancer?
Pelvic ultrasound and blood tests like CA-125 are common initial tools. If abnormalities are found, further imaging such as CT scans or biopsies may follow. These help confirm diagnosis and determine the extent of disease spread.
Is ovarian cancer hereditary?
Yes, a significant portion of ovarian cancers are linked to inherited genetic mutations like BRCA1 and BRCA2. Women with a family history of breast or ovarian cancer should consider genetic testing and counseling.
Can younger women get ovarian cancer?
While it’s more common after menopause, younger women can develop certain subtypes like germ cell tumors. In these cases, symptoms may be similar but are often misattributed to hormonal fluctuations or menstrual irregularities.
Does hormone therapy increase the risk of ovarian cancer?
Some studies suggest that prolonged use of postmenopausal hormone replacement therapy may slightly increase the risk. Women on HRT should be closely monitored, especially if they experience new or unusual pelvic symptoms.
What role do hormone receptors play in symptoms?
Some ovarian tumors express hormone receptors, which can lead to symptoms resembling menstrual cycle disturbances, such as irregular bleeding or breast tenderness. Understanding tumor biology is important for diagnosis and treatment decisions.
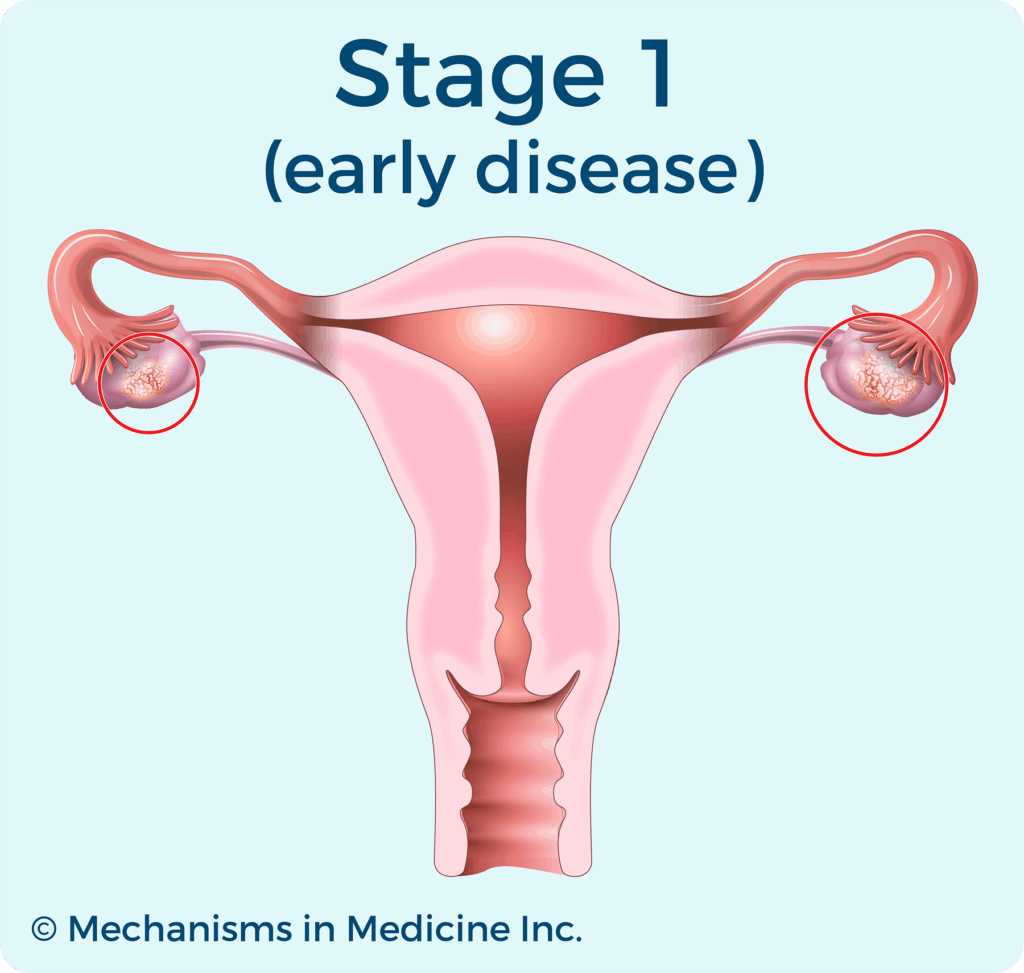
How is ovarian cancer staged after diagnosis?
Staging is determined based on tumor size, lymph node involvement, and whether the cancer has spread to other organs. This helps guide treatment and predict prognosis. Most ovarian cancers are diagnosed at stage III or higher due to delayed detection.
Is bloating always a sign of ovarian cancer?
Not always. Bloating can be caused by diet, irritable bowel syndrome, or hormonal shifts. However, if it is persistent, progressive, and not relieved by dietary changes, it should be evaluated further.
Can ovarian cancer be confused with urinary tract infections?
Yes. Increased urgency and frequency of urination, common in ovarian cancer, can mimic UTI symptoms. If antibiotics fail to resolve the issue, further pelvic assessment is warranted.
What should I do if I suspect I have symptoms?
Keep a record of your symptoms — frequency, duration, and severity — and schedule a visit with your doctor. Don’t minimize your concerns. Early detection leads to better treatment outcomes, and your attentiveness could make a life-saving difference.










