Extreme Fatigue in Hodgkin’s Lymphoma
Extreme Fatigue in Hodgkin’s Lymphoma: Why It Happens and How to Manage It
- Why Fatigue Is a Common Symptom in Hodgkin’s Lymphoma
- What Causes Fatigue in Hodgkin’s Lymphoma: Biological Mechanisms
- How Frequently Does Fatigue Affect Lymphoma Patients?
- Clinical Observations: How Fatigue Varies by Stage and Tumor Distribution
- Root Causes of Fatigue in Hodgkin’s Lymphoma and Its Treatment
- When to Take Fatigue Seriously: Medical Red Flags
- Tests and Assessments Doctors Use to Diagnose the Source of Fatigue
- Relief Strategies: How to Manage and Treat Lymphoma-Related Fatigue
- Can This Symptom Be Prevented or Reduced in Hodgkin’s Lymphoma?
- How Long Does the Fatigue Last—And Will It Go Away?
- What Oncologists Say About Fatigue in Hodgkin’s Lymphoma
- 15+ Frequently Asked Questions (FAQ)
Why Fatigue Is a Common Symptom in Hodgkin’s Lymphoma
Fatigue in cancer patients is not the same as ordinary tiredness. It is a profound, persistent lack of energy that doesn’t improve with rest and can deeply affect physical, emotional, and cognitive function. In Hodgkin’s lymphoma, extreme fatigue is one of the most commonly reported symptoms, both before and during treatment.
This fatigue can precede diagnosis or emerge as a side effect of therapy. It may involve the inability to concentrate, loss of motivation, physical weakness, or a sense of being “drained” even after minimal activity. Unlike sleep-related fatigue, this type is often systemic—linked to inflammation, immune system activation, and the body’s metabolic response to malignancy.
Patients often describe it as overwhelming and debilitating, interfering with their daily routines, social life, and ability to work. Understanding why it occurs in Hodgkin’s lymphoma can lead to better coping strategies and individualized management.
What Causes Fatigue in Hodgkin’s Lymphoma: Biological Mechanisms
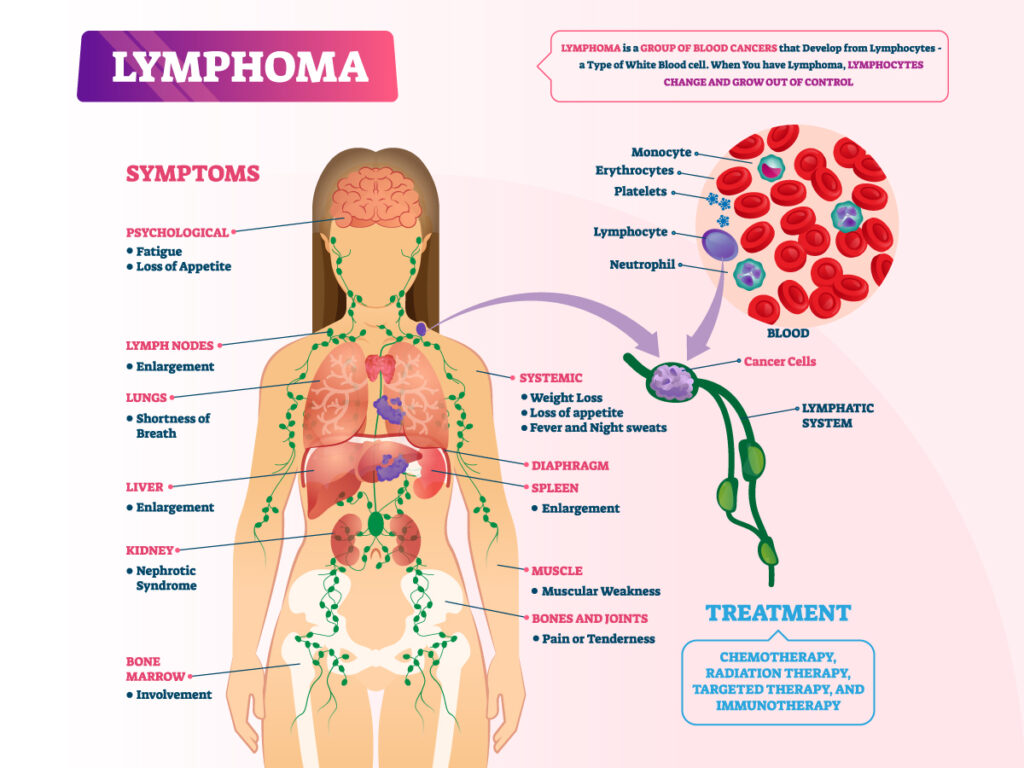
The mechanisms behind fatigue in Hodgkin’s lymphoma are multifactorial. First and foremost, cancer-related fatigue is driven by the body’s inflammatory response to the tumor. Cytokines like interleukin-1, interleukin-6, and tumor necrosis factor-alpha are released in large quantities, disrupting sleep regulation, mood, and muscle metabolism.
Hodgkin’s lymphoma typically involves abnormal lymphocytes—Reed-Sternberg cells—which create a chronic immune-stimulating environment. This heightened immune activity contributes to what is known as “sickness behavior”—a state marked by low energy, loss of interest, and cognitive fog.
Furthermore, anemia is common in lymphoma patients, either due to the disease itself or as a result of chemotherapy. Low red blood cell counts reduce oxygen delivery to tissues, compounding physical exhaustion.
Treatments like ABVD chemotherapy, radiation, and immunotherapy also damage healthy cells, particularly in bone marrow and the digestive tract. These side effects result in nutritional deficits, dehydration, and reduced energy levels. As documented in Blood Tests for Lymphomas, laboratory workups often reveal electrolyte imbalances and low hemoglobin—all contributing to fatigue.
How Frequently Does Fatigue Affect Lymphoma Patients?
Extreme fatigue is reported by more than 80% of Hodgkin’s lymphoma patients at some point during their cancer journey. In fact, it is often one of the first symptoms to appear—sometimes months before diagnosis—and may persist well beyond the conclusion of treatment.
In early-stage Hodgkin’s lymphoma (stage I or II), fatigue may be mild and intermittent, often dismissed as stress or overwork. As the disease advances into stages cancer III and IV, fatigue becomes more persistent and severe due to higher systemic inflammation, increased tumor burden, and greater nutritional depletion.
Post-treatment fatigue is also common. Studies show that up to 40% of survivors continue to experience significant fatigue six months or more after completing therapy, particularly if they received radiation or high-dose chemotherapy. Factors like age, gender, comorbidities, and depression can increase vulnerability to chronic fatigue.
Unlike pain or nausea, fatigue is often underreported but ranks among the top quality-of-life concerns for lymphoma patients and survivors.
Clinical Observations: How Fatigue Varies by Stage and Tumor Distribution
Fatigue patterns in Hodgkin’s lymphoma can often be correlated with the cancer’s stage and anatomical spread.
In stage I disease, where involvement is localized to a single lymph node region, fatigue may be minimal or even absent. It’s more likely attributed to psychological stress than systemic disease burden.
In stage II, where two or more lymph node groups on the same side of the diaphragm are affected, mild to moderate fatigue may emerge—especially if large mediastinal masses compress airways or blood vessels, impairing oxygen delivery.
By stage III or IV, which involve lymph nodes on both sides of the diaphragm or organs like the liver, bone marrow, or spleen, fatigue is almost always present. Tumor infiltration in the bone marrow leads to anemia and immune dysfunction, while liver involvement disrupts metabolism and toxin clearance, both of which intensify exhaustion.
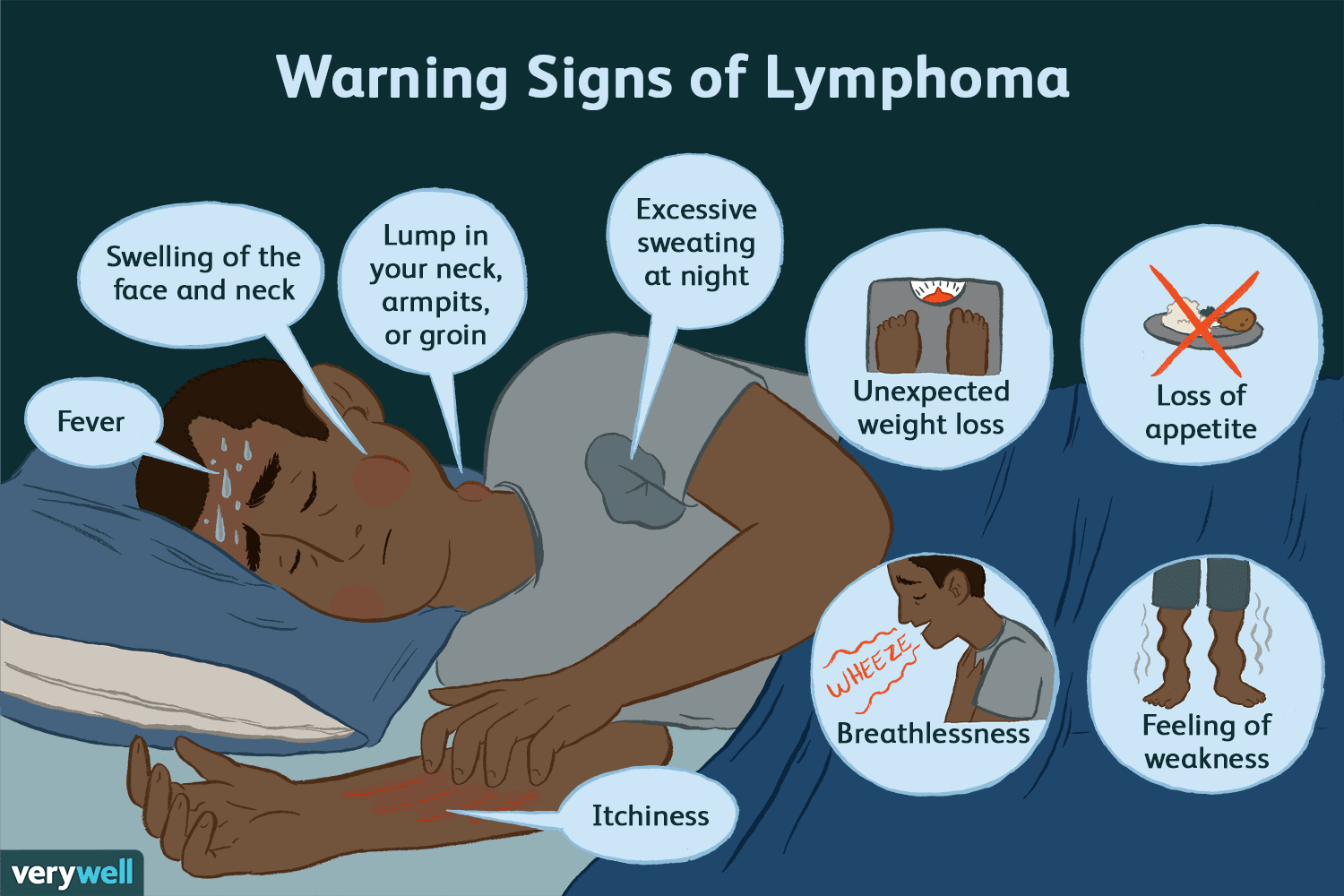
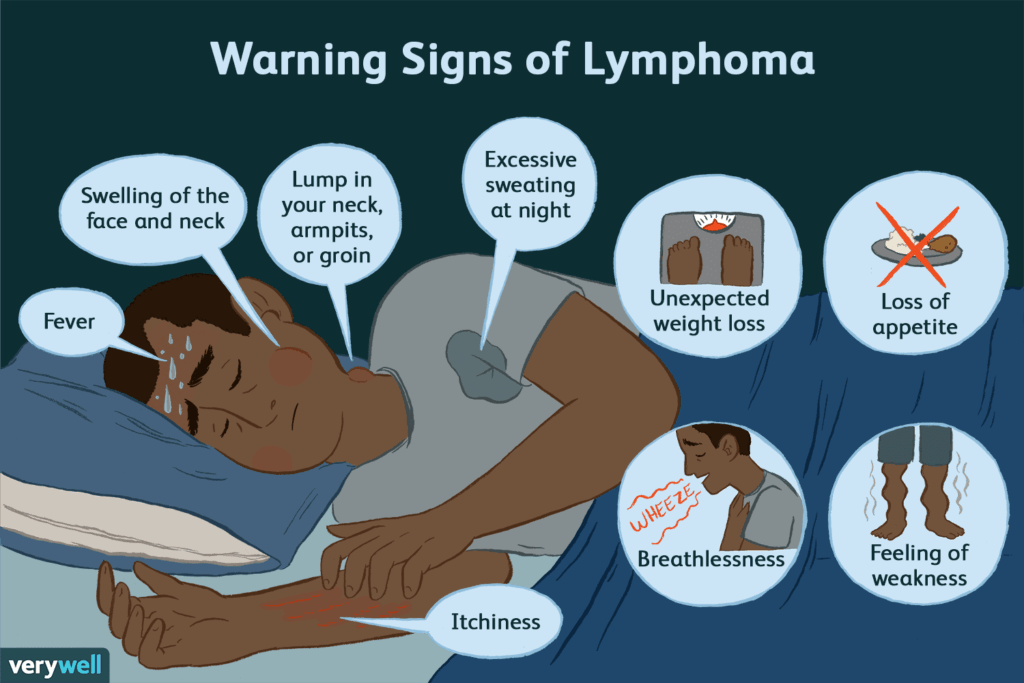
Moreover, advanced disease often triggers B symptoms—fever, night sweats, and weight loss—all of which correlate strongly with extreme fatigue and decreased performance status.
Root Causes of Fatigue in Hodgkin’s Lymphoma and Its Treatment
Fatigue in Hodgkin’s lymphoma patients stems from a variety of overlapping causes—some directly related to the cancer itself, and others induced by treatment or the body’s reaction to both.
Tumor-Induced Inflammation
The immune system reacts aggressively to Reed-Sternberg cells (the hallmark of Hodgkin’s lymphoma), triggering a cascade of inflammatory cytokines. These substances alter central nervous system signaling, increase resting energy expenditure, and contribute to a persistent sense of exhaustion.
Chemotherapy Side Effects
Regimens like ABVD (doxorubicin, bleomycin, vinblastine, dacarbazine) damage not only cancer cells but healthy cells as well. The result is anemia, reduced immunity, and digestive toxicity, all of which compromise energy levels.
Radiation Therapy
Radiation to the chest or neck can suppress bone marrow function and thyroid activity—both of which regulate metabolic energy. Hypothyroidism is a known delayed complication in patients receiving mantle-field radiation.
Nutritional and Electrolyte Deficiencies
Chemotherapy can lead to nausea, vomiting, and appetite loss. Combined with damage to the gut lining, this impairs absorption of iron, B12, and electrolytes—all of which are critical to muscle and cognitive energy.
Psychological Stress and Sleep Disturbances
The emotional burden of a cancer diagnosis, along with insomnia or disrupted sleep from steroid medications or night sweats, amplifies perceived fatigue.
Understanding these layered mechanisms helps clinicians address fatigue as more than a minor side effect—it is often a systemic manifestation of the disease and its treatment.
When to Take Fatigue Seriously: Medical Red Flags
While fatigue is expected in many cancer journeys, certain warning signs indicate it could be masking a more urgent issue. Patients and caregivers should watch for these red flags:
- Sudden or rapidly worsening fatigue not relieved by rest
- Fatigue accompanied by dizziness or fainting
- Severe shortness of breath during minimal exertion
- Palpitations, chest pain, or new swelling in legs or ankles
- Persistent or worsening fever and chills, suggesting infection
- Dark stools or signs of internal bleeding (which can cause anemia)
- Fatigue that prevents basic activities like walking or eating
These symptoms could indicate complications such as sepsis, deep anemia, cardiac involvement, or adrenal insufficiency from steroid use. In the context of Hodgkin’s lymphoma, they warrant immediate medical attention.
Patients should also report fatigue that interferes with treatment adherence—missing chemotherapy appointments, failing to take medications, or becoming socially withdrawn. These are functional markers of severe fatigue that require both medical and psychosocial support.
Tests and Assessments Doctors Use to Diagnose the Source of Fatigue
Diagnosing the true cause of fatigue in lymphoma patients involves ruling out treatable contributors while assessing the disease’s broader impact on the body.
Blood Tests
- Complete Blood Count (CBC): Identifies anemia, neutropenia, and thrombocytopenia
- Ferritin, iron, B12, folate levels: Detect nutritional causes of fatigue
- Thyroid Function Tests (TSH, T4): Evaluate for hypothyroidism, especially after radiation
- Electrolyte panel (Na, K, Mg, Ca): Reveals metabolic imbalances
- C-reactive protein (CRP) and ESR: Measure systemic inflammation
These tests, which are part of routine Blood Tests for Lymphomas, provide insight into whether fatigue is driven by inflammation, infection, marrow suppression, or other treatable factors.
Cardiac and Pulmonary Tests
For patients on anthracycline chemotherapy (like doxorubicin), echocardiograms may be ordered to rule out chemotherapy-induced cardiomyopathy.
Pulmonary function tests may be needed in patients receiving bleomycin, which is known to cause lung toxicity and breathlessness.
Functional Assessment
Fatigue scales like the Brief Fatigue Inventory (BFI) or FACT-F (Functional Assessment of Chronic Illness Therapy–Fatigue) help quantify impact and monitor change over time.
Sleep Studies and Mental Health Screening
If fatigue appears out of proportion to lab findings, screening for sleep apnea, depression, or anxiety may be indicated. These are common yet under-recognized contributors to persistent cancer-related fatigue.
Relief Strategies: How to Manage and Treat Lymphoma-Related Fatigue
Managing extreme fatigue in Hodgkin’s lymphoma requires a multi-pronged approach, tailored to each patient’s physical, emotional, and treatment context.
Treat the Underlying Cause
If blood tests reveal anemia, iron or erythropoietin supplements may be prescribed. Correcting thyroid dysfunction or electrolyte imbalances often leads to rapid improvement in energy levels.
Energy Conservation Techniques
Occupational therapists teach pacing strategies: alternating activity with rest, organizing tasks efficiently, and avoiding energy “crashes.” Using assistive devices or home support can reduce physical strain.
Light to Moderate Physical Activity
Paradoxically, exercise helps reduce cancer-related fatigue. Walking, yoga, or stationary cycling for 15–30 minutes a day boosts circulation, mood, and muscle strength. It also improves sleep.
Psychological Support
Counseling, support groups, and cognitive behavioral therapy (CBT) have been shown to reduce fatigue severity—particularly in those dealing with grief, anxiety, or fear of recurrence.
Pharmacologic Options
In selected cases, low-dose psychostimulants (like methylphenidate) or corticosteroids are used under medical supervision. These are typically short-term solutions for patients with functional impairments or palliative needs.
Sleep and Nutrition Optimization
Encouraging consistent sleep-wake schedules, minimizing nighttime interruptions, and correcting vitamin deficiencies (especially B12 and D) can meaningfully improve fatigue.
Fatigue may not disappear entirely during treatment, but with structured care, it becomes manageable—allowing patients to maintain independence, dignity, and hope.
Can This Symptom Be Prevented or Reduced in Hodgkin’s Lymphoma?
Although extreme fatigue is a common experience in Hodgkin’s lymphoma, it can often be reduced or prevented from becoming debilitating with early interventions and lifestyle adjustments.
Proactive Monitoring
Fatigue should be monitored from the point of diagnosis, not just once treatment begins. Keeping a symptom diary can help identify patterns or triggers, such as dehydration, medication timing, or nutritional deficits.
Nutritional Support
Working with a dietitian to maintain adequate protein, caloric intake, and hydration can prevent malnutrition-driven fatigue. Supplements (like iron, B12, or vitamin D) may be introduced early in high-risk patients.
Early Physical Activity
Light, regular exercise before and during treatment—tailored to energy levels—has been shown to reduce the intensity of fatigue and improve cardiovascular resilience.
Addressing Sleep and Mental Health Early
If patients are experiencing insomnia, anxiety, or depressive symptoms, these should be treated proactively. Managing emotional health is crucial for sustaining energy.
While fatigue may not be fully preventable, these supportive strategies can lessen its intensity and duration, particularly during the demanding phases of chemotherapy or radiation.
How Long Does the Fatigue Last—And Will It Go Away?
Fatigue in Hodgkin’s lymphoma can be acute, chronic, or even late-onset—depending on treatment course, individual resilience, and presence of complications.
During Active Treatment
Fatigue typically peaks within days of chemotherapy administration and can last several weeks. It often fluctuates with treatment cycles, gradually intensifying over time if not managed.
Post-Treatment
Most patients begin to recover within 1–3 months after therapy ends. However, up to 30–40% continue to experience persistent fatigue for six months or longer, particularly those who received radiation or stem cell transplants.
Long-Term Survivors
For some, fatigue becomes a long-term survivorship issue. Known as cancer-related fatigue syndrome, it may last years and require ongoing multidisciplinary support.
Factors that increase the risk of prolonged fatigue include:
- Older age
- Female gender
- Coexisting depression or anxiety
- High-dose chemotherapy or radiation
- Persistent anemia or hormonal imbalances
Fortunately, with structured care, most patients regain substantial energy and functioning over time. Fatigue that lasts indefinitely is the exception—not the rule.
What Oncologists Say About Fatigue in Hodgkin’s Lymphoma
Experienced oncologists increasingly recognize fatigue as a critical symptom deserving equal attention as pain, fever, or infection.
Dr. Lillian Moore, hematologist at a leading U.S. cancer center, shares:
“Fatigue is not just ‘being tired.’ In Hodgkin’s lymphoma, it can be the first symptom and the last to go. It affects treatment tolerance, mental health, and quality of life. We treat it seriously.”
Dr. Rafael Choudhury, radiation oncologist, adds:
“Patients undergoing mantle field or neck radiation often experience thyroid dysfunction that worsens fatigue months later. It’s important we monitor labs long after therapy ends.”
Both experts agree that integrating fatigue screening into routine oncology visits improves survivorship outcomes. They advocate early referrals to psycho-oncology, physiotherapy, and nutrition teams—rather than waiting until patients are severely affected.
They also note how fatigue data from stages cancer registries is improving awareness, showing how symptom burden can be tracked across different phases of lymphoma treatment and recovery.
15+ Frequently Asked Questions (FAQ)
1. Is fatigue a sign of Hodgkin’s lymphoma before diagnosis?
Yes. For some, fatigue appears months before other symptoms like swollen nodes or fever. It’s often mistakenly attributed to stress or viral illness.
2. Can fatigue be the only symptom?
In rare cases, yes—particularly in early stages. But it’s usually accompanied by night sweats, weight loss, or lymph node enlargement.
3. Will chemotherapy make my fatigue worse?
Most likely, yes—especially within the first week of each cycle. However, it often improves between treatments with rest and supportive care.
4. How do I know if my fatigue is from anemia?
Lab tests like CBC and ferritin can show if red blood cells are low. Anemia-related fatigue often includes dizziness, pale skin, and shortness of breath.
5. Can I exercise if I’m extremely fatigued?
Yes, but only light activity. Walking or gentle stretching helps more than bed rest alone. Listen to your body and start small.
6. Do steroids help with lymphoma fatigue?
In some cases, yes—especially in palliative settings. But they have side effects and are usually reserved for short-term use.
7. Should I stop treatment if fatigue is unbearable?
Never stop treatment without consulting your oncologist. They may adjust the dose, schedule, or add supportive therapies to help.
8. Can antidepressants reduce cancer fatigue?
They can help if fatigue is linked to mood issues like depression or anxiety. Otherwise, their effect on physical fatigue is limited.
9. How can I explain this to my family or employer?
Fatigue from cancer is real and medical. It’s not laziness. Sharing educational resources or having a doctor explain can help others understand.
10. Will fatigue go away after radiation therapy?
For many, yes—within 1–2 months. But if the thyroid is affected, fatigue can persist until hormone levels are corrected.
11. What foods help with energy during lymphoma?
High-protein, iron-rich, and nutrient-dense foods like eggs, lentils, and smoothies support energy. Avoid sugary snacks that cause energy crashes.
12. Can hydration help with cancer fatigue?
Absolutely. Dehydration intensifies fatigue. Aim for small, frequent sips of water throughout the day, even if you’re not thirsty.
13. Is it safe to take supplements?
Only under medical supervision. Some may interfere with treatment. Always ask your doctor before starting new vitamins or herbs.
14. Are there support groups for cancer fatigue?
Yes. Many hospitals and cancer centers offer survivorship or energy management groups. Peer support helps emotionally and practically.
15. When should I ask for help with fatigue?
Right away. Don’t wait until you’re overwhelmed. Fatigue deserves treatment like any other symptom—it’s valid and manageable.