Endometriosis Treatment Options in 2025: What Women Need to Know
👩⚕️ Dr. Emily Hart, MD — Board-Certified Physician in Internal Medicine
Medically reviewed • Last updated: September 2025
“In my years of practice, I have seen many women struggle with endometriosis — often for years before receiving a clear diagnosis. The pain can affect work, relationships, and the ability to have children. In this guide, I will explain the current treatment options, highlight what’s new in 2025, and share how women can work with their doctors to find the most effective, personalized plan of care.”
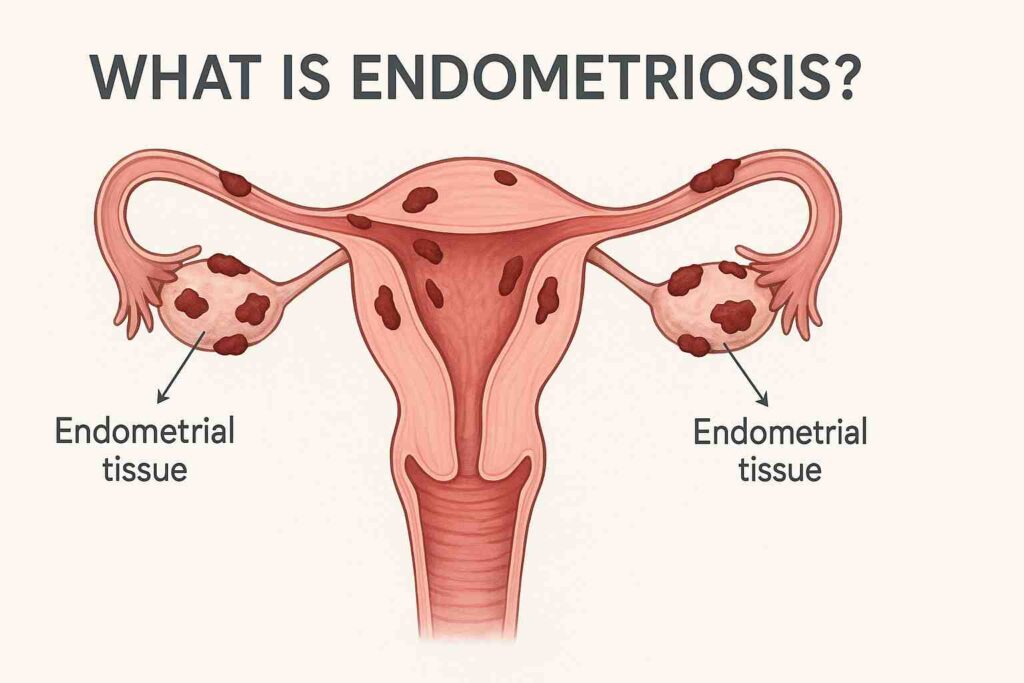
Endometriosis remains one of the most challenging conditions women face in reproductive health. Many of my patients tell me that their pain started years before they received a proper diagnosis. This delay often leads to frustration, fear, and an impact on daily life — from work to relationships.
In 2025, treatment options continue to expand, giving women more ways to manage symptoms and protect fertility. In this article, I will walk you through why endometriosis can be difficult to treat, what standard and new therapies are available this year, and how lifestyle changes can complement medical care. My goal is to help you feel informed, supported, and ready to discuss the right plan with your doctor.
Why treating endometriosis can be challenging
Managing endometriosis is rarely straightforward. The condition behaves differently in every woman, which makes treatment complex. Some find relief with medication, while others need surgery or a mix of both. Even when pain improves, endometriosis can return, affecting fertility and daily life. This is why doctors emphasize personalized care instead of a one-size-fits-all approach.
Why symptoms often return after treatment
Many women feel discouraged when their pain comes back after treatment. In my practice, I often meet patients who had surgery or hormonal therapy, only to notice symptoms again within a few years. This happens because endometriosis is a chronic condition — the tissue that resembles the lining of the uterus can grow back or persist in hidden areas.
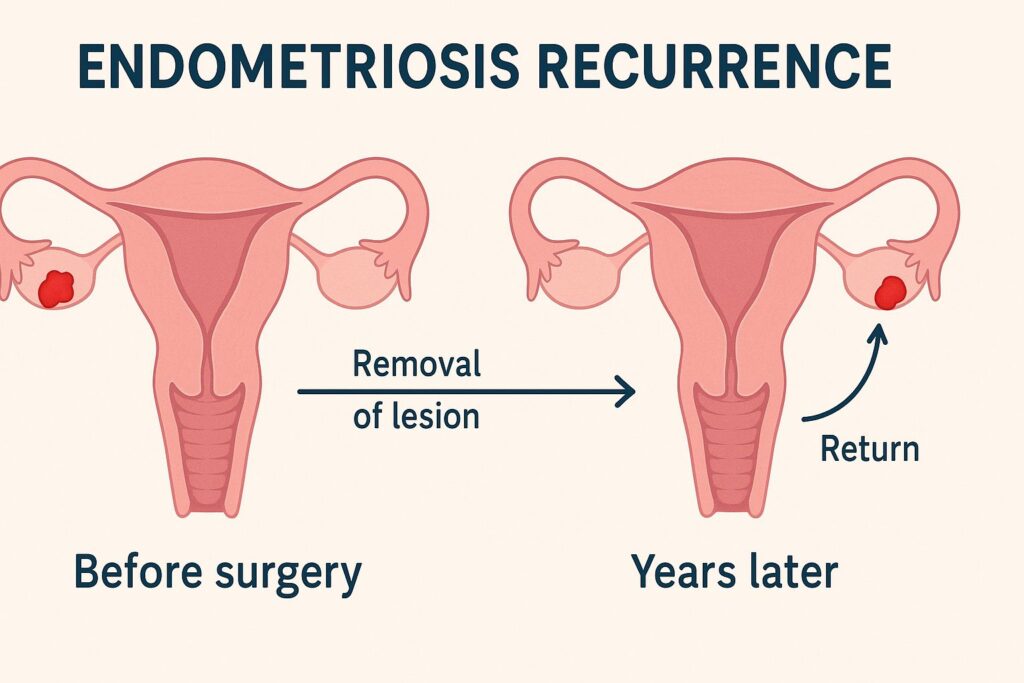
Hormonal therapy may suppress symptoms but does not remove existing lesions. Surgery can remove visible tissue, but tiny implants sometimes remain and continue to cause inflammation. Genetics, hormone levels, and immune system factors also play a role in recurrence. That is why long-term management usually combines medical treatment, lifestyle adjustments, and regular follow-up with a doctor, rather than expecting a permanent cure from a single intervention.
Impact on fertility and daily life
Endometriosis does more than cause pain — it often affects a woman’s ability to plan her future. In my consultations, I meet patients who worry about whether they will be able to have children. Endometriosis can damage the ovaries, block fallopian tubes, or interfere with egg quality, all of which make pregnancy more difficult.
Beyond fertility, the condition disrupts everyday life. Persistent pelvic pain may make it hard to focus at work, enjoy social activities, or maintain intimacy in relationships. Some women experience fatigue from chronic inflammation or side effects of medications. These challenges explain why endometriosis is not only a medical issue but also a condition that impacts quality of life at every level.
Why a personalized treatment plan is essential
No two women experience endometriosis in the same way. Some have mild pain with severe fertility problems, while others struggle with daily discomfort but conceive without difficulty. Because of these differences, doctors cannot rely on a single “standard” solution.
In my practice, I encourage patients to share their priorities: pain relief, fertility preservation, or minimizing side effects. A personalized treatment plan considers age, severity of symptoms, reproductive goals, and how previous therapies worked. This approach helps women feel more in control of their care and increases the chance of long-term success.
H2: Current standard treatments for endometriosis
Doctors usually start treatment with established therapies that have been studied for many years. These approaches aim to relieve pain, control the growth of endometriosis tissue, and support fertility when possible. While not every option works for every woman, understanding the standard treatments helps patients make informed choices.
Pain management with NSAIDs
Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or naproxen, reduce inflammation and ease menstrual cramps. Many women use them as the first step when pain flares up. In my practice, I often recommend trying NSAIDs before moving to stronger therapies.
These medications can lower pelvic pain and improve daily comfort, but they do not treat the root cause of endometriosis. Some women also experience stomach irritation or other side effects if they take NSAIDs for long periods. Because of this, doctors usually combine NSAIDs with other therapies for more complete control.
Hormonal therapy (birth control pills, progestins, GnRH antagonists)
Hormonal therapy aims to control how estrogen fuels the growth of endometriosis tissue. Birth control pills and progestins can regulate periods, reduce heavy bleeding, and lessen pain. Many of my patients notice clear improvement after just a few months on these medications.
For women with more severe symptoms, newer options like GnRH antagonists switch off ovarian hormone production more strongly. This approach often brings significant pain relief, but it can also lead to menopausal-like side effects such as hot flashes or bone thinning. Because of this, doctors monitor patients closely and adjust doses or combine therapy with protective add-ons.
Surgery (laparoscopy and excision techniques)
When medications do not provide enough relief, surgery becomes the next step. Laparoscopy, a minimally invasive procedure, allows surgeons to look inside the pelvis with a small camera and remove visible endometriosis tissue. In my practice, I have seen women regain significant quality of life after this approach.
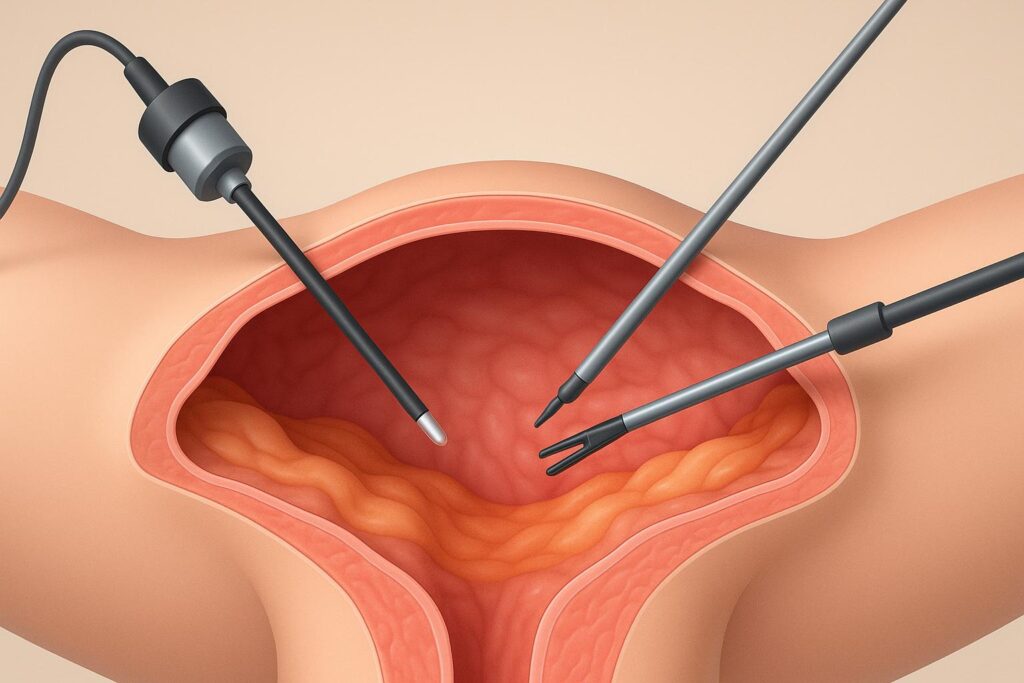
Excision techniques, where surgeons carefully cut out lesions rather than just burning them, often bring longer-lasting relief. However, no surgery guarantees that endometriosis will never return. Small implants may remain or new ones may grow later. Recovery is usually quicker with laparoscopy compared to open surgery, but it still carries risks such as infection or scar tissue.
Fertility-focused treatments for women who want children
For women who want to conceive, treatment strategies focus on protecting or improving fertility. Doctors may recommend surgery to remove endometriosis that blocks the ovaries or fallopian tubes. Sometimes this alone increases the chance of natural conception.
If pregnancy does not happen after surgery, assisted reproductive technologies such as in vitro fertilization (IVF) provide another path. In my consultations, I emphasize that the right choice depends on age, ovarian reserve, and the extent of endometriosis. Some women benefit from combining surgery with IVF, while others move directly to fertility treatments without additional operations.
What’s new in endometriosis treatment in 2025?
In recent years, research has brought new hope to women living with endometriosis. While standard treatments remain important, 2025 introduces fresh options — from medications designed to control pain more precisely to surgical tools that make operations safer and less invasive. Keeping track of these updates helps patients and doctors choose the most effective and up-to-date care plans.
Recently approved medications in the US
In 2025, the FDA approved several new medications that give women more choices beyond traditional hormonal pills. One example is an updated class of GnRH antagonists with fewer side effects, designed to maintain bone health while still reducing pain. These drugs help women who could not tolerate older therapies due to hot flashes or mood changes.
In my practice, I now discuss these options with patients who previously had limited success with standard hormonal therapy. Having more targeted medications means women can find relief without feeling forced to choose between symptom control and long-term safety.
Advances in minimally invasive surgery
Surgical techniques also continue to improve. Surgeons now use enhanced 3D imaging and high-precision instruments during laparoscopy, allowing them to identify and remove smaller endometriosis lesions more effectively. Some centers in the US have started combining laparoscopy with robotic assistance, which improves accuracy and reduces recovery time.
I have seen patients return to normal activities faster after these newer procedures compared to older methods. While no surgery completely eliminates the risk of recurrence, advances in technology give women better outcomes and fewer complications.
Clinical trials and experimental therapies
Across the US, clinical trials in 2025 are testing new approaches that go beyond existing medications. Some studies focus on drugs that block nerve pathways involved in pelvic pain, while others test therapies that reduce inflammation without affecting hormones. Researchers are also exploring targeted biologic agents that may stop the spread of endometriosis tissue.
In my consultations, I often meet women who feel frustrated after exhausting standard treatments. For these patients, clinical trials sometimes offer access to promising therapies before they reach the market. While participation requires careful screening, trials give women hope and contribute to progress in the field.
Non-hormonal therapies under investigation
Not every woman wants or can tolerate hormonal therapy. Because of this, researchers are developing non-hormonal options. Early studies in 2025 highlight treatments that focus on the immune system and inflammation. One example is selective enzyme blockers that aim to reduce pelvic pain without altering estrogen levels.
I see growing interest from patients who ask for alternatives that do not disrupt natural hormone balance. While most of these therapies remain experimental, the potential is clear: giving women relief without the side effects linked to hormones. Doctors expect more progress in this area over the next few years.
Lifestyle and complementary approaches
Medical therapy forms the core of endometriosis care, but lifestyle choices can strengthen results and improve quality of life. In my experience, women who combine medical treatment with dietary changes, exercise, and stress management often feel more in control of their condition. While these steps do not replace professional care, they provide meaningful support alongside standard treatments.
Role of diet and anti-inflammatory foods
Nutrition plays an important role in managing inflammation, which drives many endometriosis symptoms. Diets rich in fruits, vegetables, whole grains, and omega-3 fatty acids may help reduce flare-ups. Foods like salmon, flaxseeds, leafy greens, and berries support the body’s natural anti-inflammatory processes.

In my practice, I encourage patients to limit processed foods, excess sugar, and red meat, as these can worsen inflammation and pain. While diet changes alone do not cure endometriosis, many women report less bloating, fewer painful cycles, and more stable energy when they adjust their eating habits. A thoughtful approach to food often complements medical treatment and helps women feel more in control of daily symptoms.
Exercise, stress management, and pelvic therapy
Regular physical activity helps many women with endometriosis feel stronger and less limited by pain. Low-impact exercises such as walking, swimming, or yoga reduce inflammation and improve blood flow in the pelvis. In my practice, I often see patients report better energy and fewer cramps after adding gentle movement to their routine.
Stress management also matters. Chronic stress can worsen hormone imbalance and make pain more intense. Techniques like meditation, breathing exercises, and mindfulness help lower stress levels and improve overall resilience.
Pelvic floor physical therapy, guided by trained specialists, offers targeted relief. Therapists use exercises and manual techniques to relax tight pelvic muscles, which often contribute to chronic pelvic pain. Many women notice improvement after just a few sessions.
Supplements and alternative treatments (acupuncture, herbal medicine)
Some women explore natural options to complement medical care. Omega-3 fatty acids, vitamin D, and curcumin are among the supplements studied for their potential to reduce inflammation and ease symptoms. While results vary, I sometimes recommend these options as safe add-ons when taken under medical supervision.
Acupuncture has shown promise in reducing pain and improving well-being. Several of my patients describe better sleep and less pelvic discomfort after regular sessions. Herbal medicine, including turmeric and green tea extracts, is also under investigation, but evidence remains limited. Doctors advise caution, since not all supplements and herbs are well studied or free of side effects.
Choosing the right treatment with your doctor
Endometriosis care works best when doctors and patients make decisions together. Every woman has different priorities — some focus on pain relief, others on fertility or minimizing side effects. In my practice, I always emphasize that treatment should match the individual, not just the diagnosis. Open discussions with a doctor help women weigh benefits and risks, and create a plan that feels both safe and realistic.
Factoring in severity of symptoms
The intensity of endometriosis symptoms plays a key role in treatment planning. Women with mild discomfort may benefit from simple measures like NSAIDs or lifestyle changes, while those with severe, daily pain often require hormonal therapy or surgery.
In my consultations, I ask patients to describe how pain affects their work, sleep, and relationships. This helps determine whether we start with conservative therapy or move quickly to advanced options. Factoring in symptom severity ensures that treatment addresses not only the medical side of endometriosis but also its impact on quality of life.
Considering fertility goals
Fertility goals strongly influence the direction of endometriosis treatment. Some women want to preserve the option of having children in the future, while others focus only on controlling pain. In my practice, I always ask early on whether pregnancy is part of the patient’s long-term plan.
If fertility is a priority, we may avoid certain hormonal therapies that suppress ovulation for long periods. Instead, surgery or assisted reproductive technologies may take a leading role. On the other hand, if a woman does not plan to have children, longer use of hormonal medications can provide steady relief without concern for reproductive effects.
Shared decision-making in endometriosis care
Successful care depends on open, two-way communication. Endometriosis often requires balancing multiple factors: pain levels, fertility goals, treatment side effects, and lifestyle preferences. Doctors bring medical expertise, but patients bring their own values and priorities.
In my consultations, I encourage women to ask questions, voice concerns, and share what matters most in their daily lives. When patients feel included in the process, they gain confidence in the plan and are more likely to stay consistent with treatment. Shared decision-making transforms medical care into a true partnership.
When to seek medical attention immediately
While many women manage endometriosis with ongoing care, certain warning signs require urgent medical attention. Recognizing these “red flag” symptoms helps prevent delays in diagnosis and ensures that serious complications do not go unnoticed. In my practice, I always remind patients that seeking help early can protect both health and fertility.
Severe, persistent pelvic pain
Pelvic pain that feels severe and does not improve with over-the-counter medication should never be ignored. If pain interferes with sleep, work, or daily activities, it signals that the disease may have progressed or that another condition requires attention.
I often meet women who endured intense pain for months, hoping it would fade. By the time they sought help, the disease had already advanced. Persistent pain is the body’s way of asking for evaluation. If discomfort escalates suddenly or continues despite treatment, seeing a gynecologist or specialist becomes urgent.
Sudden changes in bleeding patterns
Unexpected changes in menstrual bleeding deserve quick medical evaluation. If periods become much heavier, bleeding lasts longer than usual, or spotting appears between cycles, these shifts may point to complications linked to endometriosis or other gynecologic conditions.
In my practice, I advise women not to dismiss these changes as “just hormones.” Sudden bleeding differences can signal growth of endometrial tissue, fibroids, or even more serious problems. Seeking care promptly allows doctors to run the right tests and adjust treatment before issues worsen.
Infertility concerns that need early evaluation
Endometriosis often affects fertility, and waiting too long to investigate can reduce treatment options. If pregnancy does not occur after 6–12 months of regular attempts, women should see a fertility specialist. Early evaluation helps identify whether endometriosis is blocking the fallopian tubes, damaging the ovaries, or reducing egg quality.
I meet many patients who regret postponing this step, hoping time alone would solve the problem. By acting early, women increase their chances of success with options such as surgery or assisted reproductive technologies. Prompt evaluation can make the difference between years of frustration and a clear, proactive plan.
Summary table — treatment options in 2025
The table below highlights how different treatments for endometriosis compare in terms of effectiveness, benefits, and limitations. It can help patients and doctors quickly see which options may fit best in each situation.
| Treatment type | Effectiveness | Pros | Cons | Best for |
|---|---|---|---|---|
| NSAIDs (ibuprofen, naproxen) | Mild to moderate relief | Easy to access, inexpensive, works for menstrual pain | Do not treat disease itself, stomach irritation with long use | Women with mild or occasional symptoms |
| Hormonal therapy (pills, progestins, GnRH antagonists) | Moderate to high relief of pain and bleeding | Reduces flare-ups, widely available, multiple options | Side effects (mood changes, hot flashes, bone density loss) | Women seeking pain control without immediate pregnancy |
| Surgery (laparoscopy, excision) | High effectiveness for symptom relief, may improve fertility | Removes lesions directly, long-lasting relief for some | Recurrence possible, surgical risks, recovery time | Women with severe symptoms or fertility issues |
| Fertility-focused treatments (IVF, ART) | Improves pregnancy chances, bypasses blocked tubes | Direct path to conception, effective in many cases | Expensive, physically demanding, does not treat pain | Women actively trying to conceive |
| Lifestyle & complementary approaches (diet, exercise, pelvic therapy) | Supportive, varies by individual | Safe, empowers self-care, improves overall health | Not a cure, requires consistency, results differ | Women wanting additional support with medical care |
| New 2025 therapies (updated GnRH antagonists, robotic surgery) | Promising results in trials, growing clinical use | Fewer side effects, quicker recovery with surgery | Limited availability, high cost, long-term data pending | Women not responding to standard therapy, patients in specialized centers |
FAQs — Endometriosis Treatment in 2025
Expert’s Closing Note
“As a physician, I know how exhausting it can be to live with endometriosis. The pain often disrupts work, relationships, and personal goals. My advice is simple: do not ignore your symptoms. If pain becomes severe, bleeding changes suddenly, or fertility concerns arise, seek medical help promptly. Early evaluation gives you more options, peace of mind, and the best chance for long-term relief.”
— Dr. Emily Hart, MD
Board-Certified Physician in Internal Medicine