Understanding Ki-67 in Breast Cancer: What the Numbers Mean
Understanding Ki-67 in Breast Cancer: What the Numbers Mean
- Foreword
- Part 1: What Is Ki-67?
- Part 2: How Ki-67 Is Used in Breast Cancer Diagnosis
- Part 3: What Is Considered a “High” Ki-67 in Breast Cancer?
- Part 4: Ki-67 and Stage 1 Breast Cancer
- Part 5: How Ki-67 Affects Treatment Planning
- Part 6: Limitations and Controversies Around Ki-67
- Part 7: FAQs About Ki-67 in Breast Cancer
- Part 8: Final Thoughts
Foreword
When you first hear the words “Ki-67” during a breast cancer diagnosis, it can feel like one more confusing number in a sea of statistics and medical jargon. Maybe it shows up in a pathology report you’re struggling to decode. Maybe your doctor mentioned it briefly during a conversation already heavy with fear and uncertainty. However it arrives, Ki-67 matters — and understanding what it means can give you back a small piece of clarity during a time that often feels anything but clear.
Ki-67 isn’t about hope or despair. It’s a tool. One among many that doctors use to understand how a tumor behaves — how fast it’s growing, how likely it is to spread, and how aggressively it should be treated. High Ki-67 numbers can sound frightening. Low numbers can sound reassuring. But neither tell the whole story on their own. They’re part of a much bigger puzzle that includes tumor size, lymph node involvement, hormone receptor status, HER2 status, and other molecular features.
This article is here to walk you through it — not in abstract scientific terms, but in real human language. We’ll cover what Ki-67 is, why it matters, what “high” and “low” really mean, and how doctors actually use (and sometimes question) this information when helping you make treatment decisions. We’ll also talk about where Ki-67 fits — and where it doesn’t — in the bigger picture of living with breast cancer.
If you’re holding a pathology report in your hand right now, trying to make sense of a number that suddenly seems very personal, you’re in the right place. Let’s start with the basics: what is Ki-67, and why does it show up in breast cancer at all?
Part 1: What Is Ki-67?
Ki-67 is a protein found in the nucleus of cells during active cell division. But its story starts much deeper in cancer biology, where cell growth and division are crucial to understanding how tumors form, grow, and spread.
Ki-67: The Basics of Cell Division
Cell division is at the heart of both normal growth and cancer development. Normally, cells divide in an orderly way, based on the body’s needs. For example, when you get a cut, skin cells divide to repair the injury. In cancer, however, this orderly process breaks down. Tumor cells divide uncontrollably, growing faster than they should. This uncontrolled cell division is one of the defining characteristics of cancer.
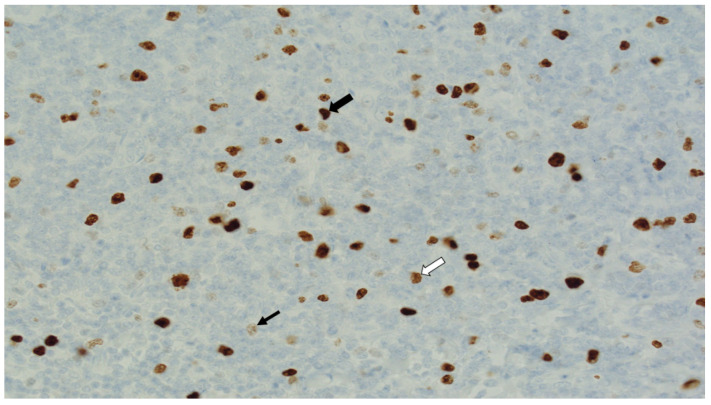
Ki-67 plays a central role in this process. It is found in proliferating cells — meaning cells that are actively in the process of dividing. Ki-67 doesn’t appear in cells that are in a resting phase (the G0 phase of the cell cycle). Instead, it’s present during the active phases of the cell cycle (G1, S, G2, and mitosis). Because of this, Ki-67 is often referred to as a proliferation marker — it acts as a sign of how quickly cells are dividing. A high Ki-67 index means the tumor is growing rapidly, while a low Ki-67 index suggests slower growth.
The Key Role of Ki-67 in Tumor Biology
Understanding Ki-67’s role in breast cancer (or any cancer) goes beyond just counting how many cells are dividing. It’s about understanding the speed of tumor progression and how aggressively the cancer is behaving. Tumors that grow quickly are more likely to spread and may be more resistant to treatment because they evolve faster, gaining new mutations that make them harder to target.
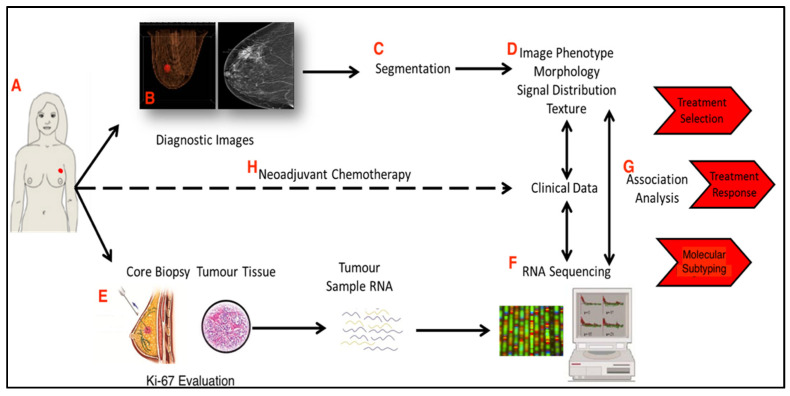
In breast cancer, Ki-67 is often used alongside other markers — like ER/PR (estrogen and progesterone receptors) and HER2 status — to give a fuller picture of the tumor’s behavior. These markers tell doctors whether the tumor is hormone-driven (ER/PR-positive), whether it has an overexpression of growth-promoting proteins (HER2-positive), and how fast it’s dividing (via Ki-67).
Ki-67 itself is also valuable because it is not dependent on hormonal influences. It’s an indicator of tumor aggressiveness and can provide crucial insight, especially in cancers that might not otherwise show clear markers for hormone therapy or targeted therapy.
Ki-67 and the Fight Against Cancer
The reason Ki-67 is such a valuable tool in breast cancer diagnosis is simple: It helps doctors understand how urgent the situation is. A high Ki-67 index often signals that a tumor is actively dividing and growing, which means the cancer could be more aggressive and more likely to spread to other parts of the body. For example, a tumor with a Ki-67 of 60% might behave much differently than one with a Ki-67 of 10% — even if both tumors are similar in size and location.
Ki-67 also provides doctors with clues about how the cancer might respond to treatment. Chemotherapy is often more effective against rapidly dividing cells. So, when a tumor has a high Ki-67, doctors may consider chemotherapy earlier in the treatment plan, even if the tumor is small or has not yet spread to lymph nodes. This is why a high Ki-67 score can sometimes lead to more aggressive treatment, while a low Ki-67 may suggest that the tumor is growing at a slower rate and may not need immediate chemotherapy.
Ki-67 and the Challenge of Tumor Heterogeneity
It’s important to note that tumors are not uniform. They can contain cells with different proliferation rates, and Ki-67 only reflects the cells that are actively dividing at the moment the biopsy was taken. So, even if a tumor has a high Ki-67 score, that doesn’t mean every cell within the tumor is dividing rapidly. Some areas of the tumor might still be relatively inactive, and treatments aimed at slowing or stopping the most aggressive cells may not address these slower-growing ones.
This issue of tumor heterogeneity can complicate treatment. For example, a tumor with a high Ki-67 might be initially responsive to chemotherapy but could become resistant as it evolves. This is why doctors continually monitor patients with high Ki-67 tumors, using imaging and blood tests to track progress and detect signs of recurrence.
Ki-67 in Context
Ki-67 can sound intimidating, but like any diagnostic tool, its value is not in the number itself but in the context in which it’s used. It helps oncologists make informed decisions, but it’s rarely the sole factor that determines the treatment plan. Whether a tumor is high or low in Ki-67 can guide doctors to consider more aggressive therapies or decide on less invasive options — but that decision always comes after looking at the bigger picture: tumor size, hormone receptor status, HER2 expression, and the overall health of the patient.
In summary, Ki-67 is a critical part of the puzzle. It’s an indication of how fast the tumor is growing, how likely it is to spread, and how aggressive treatment needs to be. But as we’ll see in the next section, it’s rarely used alone. Doctors combine it with other clinical and pathological information to craft the most appropriate treatment strategy for each individual patient.
Part 2: How Ki-67 Is Used in Breast Cancer Diagnosis
When doctors receive the results of a breast cancer biopsy, Ki-67 is one of the key pieces of information that help them understand what they’re dealing with. But it doesn’t exist in a vacuum. Ki-67 is not just a standalone number; it’s an integral part of the broader puzzle of breast cancer diagnosis, playing a crucial role in predicting the behavior of the tumor and informing treatment decisions.
Ki-67 in the Context of Other Diagnostic Markers
Ki-67 is most often used alongside other molecular markers like ER (estrogen receptor), PR (progesterone receptor), and HER2 status. Each of these plays a role in determining how the tumor will behave and how it should be treated.
- Hormone receptor-positive (ER/PR-positive) cancers respond to hormone therapy because they rely on hormones like estrogen and progesterone to fuel their growth. These tumors tend to grow more slowly, and a low Ki-67 score in such cancers is usually a good sign, suggesting a less aggressive form of disease.
- HER2-positive breast cancers are marked by the overexpression of the HER2 protein, which promotes cancer cell growth. These cancers tend to be more aggressive, and high Ki-67 scores often reinforce the need for targeted therapies like trastuzumab (Herceptin), which specifically blocks HER2.
- Triple-negative breast cancer (TNBC) is a particularly aggressive subtype, with neither estrogen, progesterone receptors, nor HER2 expression. In these cases, Ki-67 is often higher, indicating the tumor’s aggressive behavior. Chemotherapy is typically used for treatment, and the Ki-67 score can help determine how the tumor will respond to chemotherapy and how aggressively the treatment should be.
By combining Ki-67 with these molecular markers, doctors can gauge whether a tumor is likely to be responsive to hormone therapy or if chemotherapy is needed to address its more aggressive behavior. In essence, Ki-67 helps doctors make sense of the tumor’s proliferation rate, while the other markers indicate its biological drivers.
Ki-67 as a Predictor of Tumor Behavior
While Ki-67 isn’t a perfect predictor of cancer outcomes, it can still give doctors critical insights into how the tumor might behave over time. A low Ki-67 index (typically below 10–14%) suggests a slow-growing tumor. These tumors are less likely to spread quickly, and they generally respond well to less aggressive treatments. In contrast, tumors with high Ki-67 (above 20%) are considered more aggressive. High Ki-67 tumors divide more rapidly and have a greater potential to spread to other organs. This high proliferation rate means that chemotherapy or other aggressive treatments may be recommended to try to stop the cancer from advancing.
High Ki-67 levels are often associated with poor prognosis in breast cancer, but this isn’t a universal truth. Even though high proliferation rates generally indicate a more aggressive tumor, they don’t automatically correlate with poor outcomes. Some high-Ki-67 tumors shrink well with treatment, while others can become resistant. Similarly, some tumors with low Ki-67 scores may still behave aggressively in ways that aren’t predicted by Ki-67 alone. For this reason, Ki-67 should always be considered in combination with other diagnostic tools.
Ki-67 and Risk of Recurrence
One of the most important roles Ki-67 plays in diagnosis is predicting the risk of recurrence. While tumor size, lymph node involvement, and grade are all crucial in staging breast cancer, Ki-67 gives doctors a sense of how active the cancer is. A high Ki-67 score often correlates with a higher risk of recurrence after surgery, making it a key factor in deciding whether chemotherapy, radiation, or additional treatments are necessary.
Even in early-stage cancers, where the tumor is small and the likelihood of spread to lymph nodes is low, a high Ki-67 can signal that chemotherapy is needed to eliminate microscopic cancer cells that might not be visible on scans or in biopsies. Without Ki-67 as a marker of growth potential, doctors would have a harder time justifying chemotherapy for small tumors, which could otherwise be seen as low-risk.
However, the relationship between Ki-67 and recurrence risk isn’t always straightforward. In some cases, patients with low Ki-67 tumors still experience recurrences, particularly if other factors like HER2 overexpression or lymph node involvement come into play. This is why Ki-67 is never the sole determining factor when considering treatment options. It’s part of a larger, more intricate picture that includes clinical staging, genetic testing, and patient health history.
Integrating Ki-67 with Genomic Testing
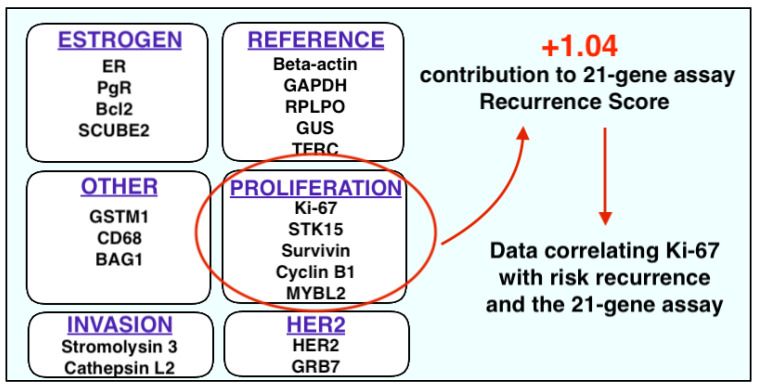
As more advanced genomic tests become widely used in breast cancer diagnosis, Ki-67 is increasingly incorporated into comprehensive multigene assays like Oncotype DX and MammaPrint. These tests provide a detailed genetic profile of the tumor, assessing how likely it is to spread and how it will respond to various therapies. Ki-67 contributes to these assessments, influencing the scores of these genomic tests and helping doctors decide whether chemotherapy is needed.
For instance, a patient with early-stage breast cancer and high Ki-67 might undergo an Oncotype DX test to better understand the likelihood of recurrence and whether chemotherapy is likely to provide benefits. If the genomic test shows a high risk of recurrence, chemotherapy might be strongly recommended despite the tumor’s small size or lack of lymph node involvement. Conversely, a low Ki-67 score paired with a favorable genomic test may lead to a decision to avoid chemotherapy and opt for hormone therapy alone.
Ki-67 is an essential tool in breast cancer diagnosis, helping doctors understand how aggressively a tumor is behaving and how it might respond to treatment. But as with any single marker, it should never be viewed in isolation. Ki-67 is part of a larger framework that includes tumor size, grade, hormonal status, HER2 status, and other markers. Only by considering all of these factors together can doctors make the most informed decisions about treatment.
As we’ve seen, Ki-67 isn’t a perfect predictor of cancer behavior, but it remains one of the most useful ways to assess how a tumor is likely to act. And for patients, understanding what Ki-67 means in the context of their own diagnosis is key to navigating treatment options with confidence and clarity.
Part 3: What Is Considered a “High” Ki-67 in Breast Cancer?
If you’re reading through a pathology report or sitting in an exam room hearing numbers thrown around, the phrase “high Ki-67” can sound alarming. But what exactly counts as “high”? And why isn’t there a single number that doctors agree on?
Generally speaking, a Ki-67 index above 20% is often considered “high” in breast cancer. That means more than 20% of the tumor cells were actively dividing at the time the sample was taken. Some studies and treatment guidelines use a lower threshold, around 14%, while others might not label a tumor as truly high-proliferation unless Ki-67 crosses 30% or even higher.
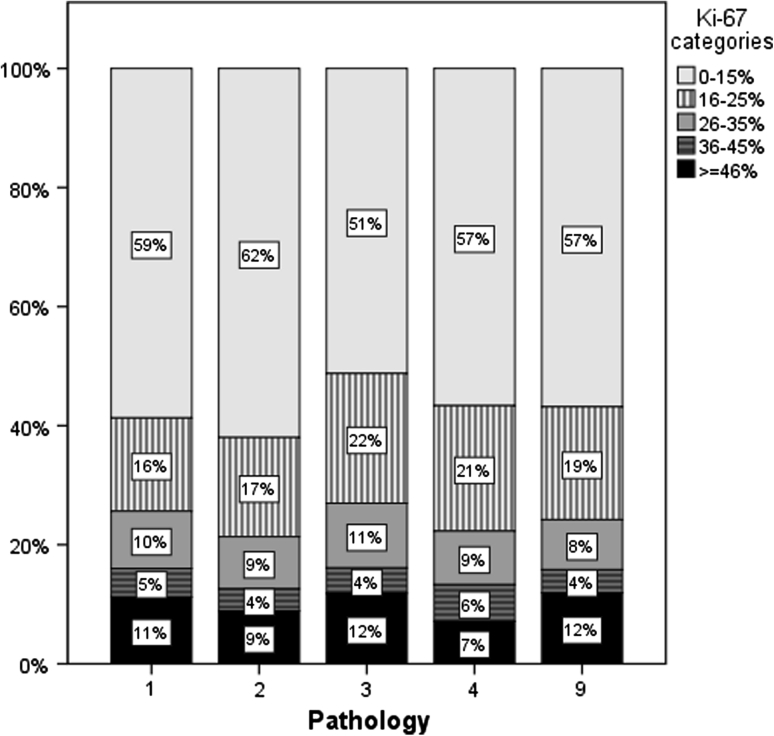
This variability comes from a few factors. Different laboratories use slightly different techniques for staining and counting Ki-67-positive cells, and human interpretation — a pathologist’s visual assessment under the microscope — inevitably introduces some degree of subjectivity. Even within the same tumor, different parts can have slightly different proliferation rates, depending on how the sample was taken.
Despite these inconsistencies, most oncologists agree on the basic principle: the higher the Ki-67, the more aggressively the tumor is growing. A tumor with a Ki-67 of 50%, for example, is likely to behave much differently than one with a Ki-67 of 5%. High Ki-67 tumors tend to grow faster, spread earlier, and, if untreated, have a higher risk of recurrence after surgery. That’s why Ki-67 often influences decisions about whether chemotherapy should be added to a treatment plan, even for early-stage breast cancers that might otherwise seem low-risk based on size alone.
It’s important to remember that Ki-67 is a spectrum, not a black-and-white label. A Ki-67 of 25% might raise eyebrows and tilt a doctor toward recommending chemotherapy, especially if other risk factors are present. A Ki-67 of 70% is a clear sign of a highly proliferative, aggressive tumor where systemic therapy is almost certainly needed. But between those extremes, interpretation often depends on the broader clinical picture: hormone receptor status, HER2 expression, lymph node involvement, patient age, and overall health.
In a way, Ki-67 is a bit like a speedometer for the tumor. A low number suggests slow movement. A high number suggests the cancer is accelerating — and treatment plans are often adjusted accordingly.
Next, we’ll talk about why high Ki-67 matters even in Stage 1 breast cancer, where the tumor is small and hasn’t spread to lymph nodes, but where its aggressive behavior can change the entire treatment conversation.
Part 4: Ki-67 and Stage 1 Breast Cancer
At first glance, Stage 1 breast cancer sounds reassuring. A small tumor, no lymph node involvement, no signs of distant spread — the kind of early catch that most people hope for. But even within Stage 1, not all cancers behave the same way. This is where Ki-67 becomes a crucial part of the story.
A small tumor with a very high Ki-67 — say, 40%, 50%, or higher — signals that the cancer is growing much faster than its size alone would suggest. In other words, while the tumor hasn’t yet had time to spread, it’s biologically aggressive. Left untreated, it would likely grow rapidly, invade nearby tissues, and potentially spread to lymph nodes or distant organs sooner rather than later.
This aggressive behavior is why doctors take high Ki-67 seriously, even when dealing with Stage 1 disease. A tiny, fast-dividing tumor can be more dangerous than a larger, slow-growing one. Treatment recommendations often reflect that reality. Patients with small but high-proliferation tumors may be offered chemotherapy in addition to surgery and radiation, even if their tumor is less than 2 centimeters and their lymph nodes are clear.
It’s not about punishing the patient with more treatment. It’s about matching the therapy to the tumor’s behavior — hitting an aggressive cancer hard before it has a chance to evolve into something much more dangerous. For patients, this can sometimes feel confusing: why is chemotherapy needed for such a small tumor? But when Ki-67 is high, size isn’t the whole story.
Real-world examples illustrate this shift in thinking. Imagine two patients, both with tumors measuring 1.5 centimeters. One tumor has a Ki-67 of 5%, is hormone receptor-positive, HER2-negative, and grade 1. The other has a Ki-67 of 60%, is triple-negative, and grade 3. Even though the tumors are the same size, their biology — and thus their treatment plans — will be completely different. One may be safely managed with surgery, radiation, and hormone therapy alone. The other will likely need aggressive chemotherapy and perhaps enrollment in clinical trials offering newer treatment options.
Stage 1 is a starting point, but it doesn’t capture the full picture. Ki-67 helps doctors see beneath the surface, identifying which small tumors carry big risks and need a bigger response.
In the next section, we’ll walk through exactly how Ki-67 levels factor into real-world treatment planning — and how doctors balance Ki-67 with all the other moving parts of a breast cancer diagnosis.
Part 5: How Ki-67 Affects Treatment Planning
Ki-67 isn’t just an academic number tucked into a pathology report. When doctors sit down with patients to build a treatment plan, Ki-67 often plays a meaningful role in shaping what comes next — especially when the path forward isn’t immediately obvious.
In many cases, a low Ki-67 score reassures both doctor and patient that a tumor is growing slowly. For a small, hormone receptor-positive, HER2-negative tumor with a low proliferation rate, the standard plan might include surgery, radiation, and hormone therapy alone, sparing the patient from the side effects and risks of chemotherapy. The tumor’s biology signals that it can be managed with a gentler approach.
But when Ki-67 is high, the conversation changes. A tumor that shows a strong drive to divide and grow may demand more aggressive action, even if it’s early-stage or node-negative. Chemotherapy might be recommended not because the tumor is large or visibly spreading, but because the cancer cells’ behavior — their relentless drive to divide — increases the risk that microscopic spread has already occurred or will occur soon.
Ki-67 can also influence the choice of systemic therapies beyond chemotherapy. In hormone receptor-positive breast cancers, a high Ki-67 score may push doctors toward combining hormone therapy with targeted agents like CDK4/6 inhibitors (for example, palbociclib (Ibrance)). These drugs specifically block the signals that drive cancer cell division, offering a more powerful blockade against aggressive tumors.
When it comes to decision-making tools like multigene assays (such as Oncotype DX or MammaPrint), Ki-67 doesn’t stand alone, but its spirit — measuring proliferation and aggressiveness — is baked into these broader genomic profiles. In some cases, a high Ki-67 will correlate with a high-risk Oncotype DX score, strengthening the recommendation for chemotherapy. In others, the full genomic analysis might reveal a lower risk than Ki-67 alone would suggest, helping patients and doctors make more nuanced decisions.
It’s important to understand that while Ki-67 is a powerful piece of information, it is not the sole driver of treatment plans. Doctors weigh it alongside tumor size, lymph node status, hormone receptor and HER2 status, tumor grade, patient age, other medical conditions, and, crucially, the patient’s own preferences and values. A high Ki-67 might push the discussion toward chemotherapy, but it doesn’t dictate it automatically.
In the real world, treatment planning is as much an art as it is a science. Ki-67 provides another lens for viewing the tumor — highlighting its urgency, its temperament, its speed. But it’s the full clinical picture that ultimately determines the best way forward.
Next, we’ll turn to an important reality check: the limitations and controversies around using Ki-67. Because as helpful as this marker can be, it isn’t perfect — and it’s important to understand where it fits and where it falls short.
Part 6: Limitations and Controversies Around Ki-67
For all the attention Ki-67 receives, it’s important to step back and recognize its limitations. Like many tools in cancer care, Ki-67 offers valuable information — but it’s not a crystal ball, and it’s not always as reliable as patients (and even some doctors) might wish.
One major challenge with Ki-67 is variability. Measuring Ki-67 isn’t a machine-read blood test; it’s a visual estimate performed by a pathologist looking at a sample under a microscope. Different labs might use slightly different staining techniques. Different pathologists might interpret the same slide a little differently. Even within a single tumor, one area might have a higher proportion of dividing cells than another, depending on where the biopsy was taken. All of this means that Ki-67 percentages can vary — not wildly, but enough that a tumor labeled “15%” in one lab might be called “20%” in another, potentially crossing the threshold from “low” to “high” in clinical decision-making.
Another limitation is lack of standardization. Unlike hormone receptor or HER2 testing, where clear international guidelines exist, Ki-67 doesn’t yet have universally agreed-upon cutoffs for what’s considered “low,” “intermediate,” or “high.” Different studies use different thresholds — 14%, 20%, 30%, or higher — and different clinical trials have drawn slightly different conclusions about its predictive power. This lack of standardization makes it harder for doctors to apply Ki-67 results consistently across different cases.
There’s also the question of what Ki-67 really predicts. A high Ki-67 score generally indicates faster-growing tumors, which often respond better to chemotherapy (which targets rapidly dividing cells). But a high Ki-67 doesn’t guarantee that chemotherapy will eliminate the cancer, nor does a low Ki-67 guarantee that the tumor is harmless. Biology is messy. Some low-proliferation tumors behave aggressively for other reasons. Some high-proliferation tumors respond beautifully to therapy and never come back.
Because of these uncertainties, many doctors treat Ki-67 as one piece of a bigger puzzle, rather than a final word. It can tilt a treatment recommendation in one direction, but rarely defines it outright. It adds nuance, not certainty.
That’s why it’s so important for patients to discuss Ki-67 results with their oncologists in the context of everything else: tumor size, lymph node status, hormone receptor status, HER2 expression, tumor grade, and overall clinical judgment. A Ki-67 score on its own tells part of the story — but never the whole story.
In the next section, we’ll shift into answering some of the most common questions patients have about Ki-67 — from whether it changes over time to what a “normal” Ki-67 really looks like.
Part 7: FAQs About Ki-67 in Breast Cancer
Even after all the technical explanations, Ki-67 tends to leave patients and families with lingering questions. Some of these questions come up in the doctor’s office. Others surface later, lying awake at night, turning over numbers and possibilities in the mind. Here, we’ll walk through some of the most common questions people ask about Ki-67 — and give clear, honest answers grounded in the realities of breast cancer care.
Is Ki-67 the same as tumor grade?
Not exactly, although they are related. Tumor grade refers to how abnormal the cancer cells look under the microscope compared to normal breast tissue. Grade 1 tumors look more like healthy cells and tend to grow slowly. Grade 3 tumors look highly abnormal and tend to grow faster. Ki-67, on the other hand, measures how many cells are actively dividing at the moment the tissue was sampled. While high-grade tumors often have high Ki-67 scores, and low-grade tumors often have low Ki-67, it’s not a perfect overlap. A tumor could be moderately graded (Grade 2) but still have a very high or very low Ki-67, influencing how aggressive the treatment plan needs to be.
What is a normal Ki-67 level?
In normal, healthy breast tissue, Ki-67 is very low — usually less than 5%. In benign (non-cancerous) breast conditions, Ki-67 remains low as well. In breast cancer, there’s no universally agreed-upon “normal” Ki-67, but tumors with Ki-67 under 10–14% are often considered low-proliferation. Above that range, doctors begin to think about increased risk and the potential need for more aggressive treatments, although the final decision always depends on multiple factors.
Can Ki-67 change over time?
Yes, it can. Ki-67 is a snapshot of what’s happening inside the tumor at the moment the sample is taken. Over time — especially after treatments like chemotherapy, targeted therapy, or hormone therapy — the Ki-67 level in a tumor can decrease if the therapy is effective. Conversely, if a tumor becomes more aggressive or stops responding to treatment, Ki-67 can increase. In some cases of recurrent or metastatic disease, doctors may re-biopsy the tumor to reassess Ki-67 and other markers, helping to guide new treatment strategies.
Does a high Ki-67 mean my cancer will definitely spread?
No — not by itself. A high Ki-67 indicates that the cancer cells are dividing more rapidly, which can increase the risk of spread or recurrence. But it’s not a guarantee. Many other factors influence whether a cancer will metastasize, including tumor size, lymph node involvement, molecular subtype (like triple-negative or HER2-positive), and how the tumor responds to initial treatment. A high Ki-67 signals higher risk, but it does not seal fate. With the right therapies, even aggressive tumors can often be brought under control.
Should treatment decisions be based only on Ki-67?
Definitely not. Ki-67 is an important piece of information, but it’s only one of many that doctors use to design treatment plans. Decisions about surgery, chemotherapy, radiation, hormone therapy, or targeted therapy depend on a complete understanding of the tumor’s biology, the patient’s health, personal preferences, and available treatment options. Ki-67 may nudge decisions in one direction, but it never tells the whole story on its own.
Numbers like Ki-67 can feel cold, clinical, and distant — until they suddenly become part of your personal story. Understanding what Ki-67 measures, how it fits into your diagnosis, and what it can and cannot predict offers something precious in the middle of a difficult journey: the ability to ask better questions, to weigh options more clearly, and to walk forward with open eyes.
Next, we’ll close this article by bringing all these ideas together — and offering a few final thoughts about what Ki-67 means, and what it doesn’t.
Part 8: Final Thoughts
Numbers can feel heavy when they’re tied to something as personal as cancer. Ki-67 is just a number on a report, but it represents something much bigger: how a tumor behaves, how it grows, how urgently it needs to be treated. It’s easy to fall into thinking that a single score defines everything — that a high Ki-67 is a guarantee of danger, or a low Ki-67 a guarantee of safety. But real life is almost never that simple.
In truth, Ki-67 is one thread in the complex weave of cancer biology. It offers doctors valuable information about how fast a tumor is dividing, helping shape treatment decisions with greater precision. It can explain why two people with similarly sized tumors might be offered very different plans. It can tilt the balance between watchful waiting and immediate action. But it doesn’t stand alone. It doesn’t predict the future with certainty. And it doesn’t erase the possibility of good outcomes even when the score is high.
Facing a Ki-67 result — especially a high one — can be frightening. But it also means that doctors have more information about the enemy they’re fighting. Fast-dividing tumors are often more sensitive to chemotherapy. Aggressive tumors caught early and treated well can still be beaten back, sometimes for many years. New therapies are continually emerging, offering new hope even for cancers once considered especially high-risk.
If Ki-67 is part of your story, let it be information, not condemnation. Use it to ask better questions, to understand your options more fully, to plan your next steps with clarity rather than fear. The number matters — but not as much as how you and your care team use it, together, to chart a path forward.









